Chakkar vertigo: BPPV vs vestibular neuritis represent two of the most common causes of dizziness and balance disorders. Understanding the differences between these conditions is crucial for accurate diagnosis and appropriate treatment. This comprehensive guide explains how to distinguish between chakkar vertigo patterns associated with BPPV, vestibular neuritis, and other balance disorders that often get confused with each other.
TL;DR
BPPV (Benign Paroxysmal Positional Vertigo): Seconds-long spinning triggered by specific head movements, caused by loose crystals in the inner ear. Treatable with Epley Maneuver (success rate 80-90%). For complex cases, Dr. Prateek employs the proprietary Bangalore Maneuver.
Vestibular Neuritis: Viral inflammation of the balance nerve causing persistent dizziness lasting hours to days. Self-limiting; recovery occurs with central compensation.
Posterior Circulation Stroke: Dangerous condition mimicking vestibular neuritis but identified by failing the HINTS exam (Head Impulse, Nystagmus, Test of Skew). Requires immediate emergency intervention.
Table of Contents
ENGLISH VERSION
Stop Calling Everything “Chakkar”: How to Tell Apart 3 Serious Conditions That Mimic Each Other
The Problem with the Word “Chakkar”
When a patient walks into a clinic and says, “Doctor, mujhe chakkar aata hai,” it can mean almost anything. Chakkar—the Hindi/Urdu word for dizziness—describes a spectrum of sensations: violent spinning, feeling faint, confusion, unsteadiness, or even a vague sense of imbalance. This linguistic ambiguity is a major diagnostic hurdle in emergency medicine and primary care.
A patient saying “I have chakkar” is like a car owner telling a mechanic, “My car is making a noise.” The mechanic cannot fix the problem without knowing: Is it a squealing sound (belt issue)? A grinding sound (brake problem)? A knocking sound (engine trouble)? Similarly, your doctor cannot diagnose your vertigo correctly without understanding what exactly you feel, how long it lasts, and what triggers it.
In clinical practice, what a patient means by “dizziness” is often far less reliable for diagnosis than identifying the specific triggers and duration of the sensation. This is why precise symptom description can be the difference between receiving the correct treatment and enduring years of unnecessary medications or brain scans.
To ensure you receive the correct diagnosis and treatment, it is vital to distinguish between three conditions that are frequently confused: Benign Paroxysmal Positional Vertigo (BPPV), Vestibular Neuritis, and Stroke. All three cause spinning sensations; all three are triggered by the balance system; but all three require completely different management approaches.
Condition 1: BPPV – The “Mechanical” Spin (Seconds)
What Is BPPV?
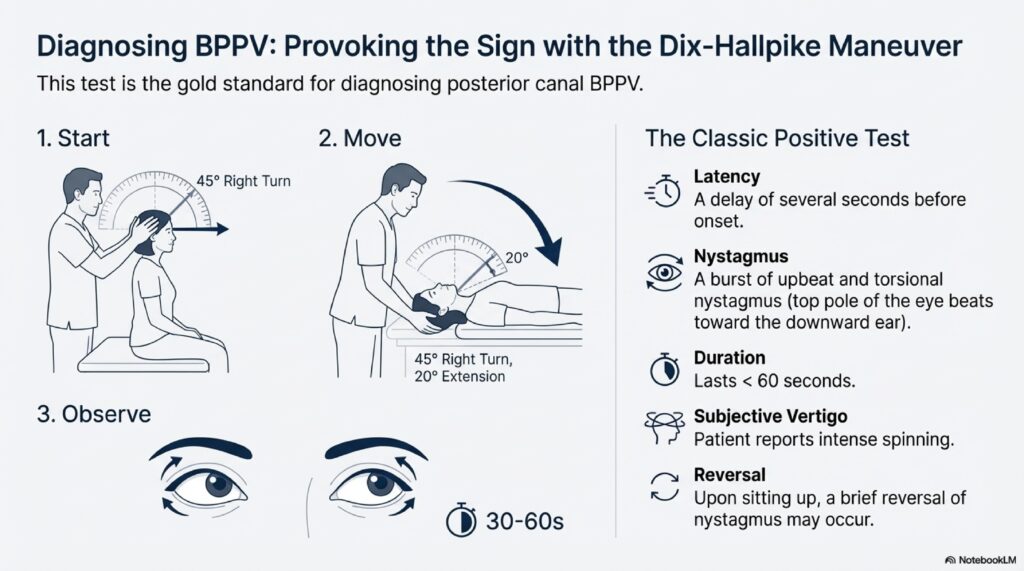
Benign Paroxysmal Positional Vertigo (BPPV) is the most common cause of peripheral vertigo, accounting for approximately 20–25% of all consultations in specialized balance clinics. Importantly, it is not a disease in the traditional sense but rather a mechanical disorder of the inner ear.
The Crystal Culprit
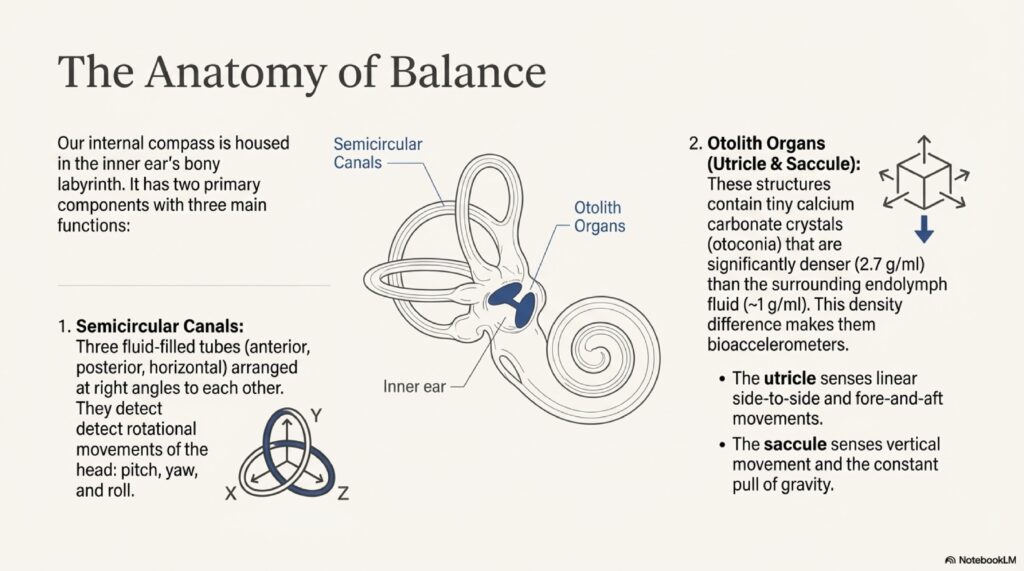
Inside your inner ear, there are specialized sensory organs called the utricle and saccule (part of the otolith organs). These organs contain tiny calcium carbonate crystals called otoconia—imagine them as microscopic “stones” that detect gravity and linear motion.
In BPPV, these crystals become dislodged from their normal position and migrate into one of the three semicircular canals (the tubes that detect head rotation). When you move your head, these “stones” move under the force of gravity, creating an inappropriate flow of fluid through the canal. This false signal tricks your brain into believing you are spinning—even though you are perfectly still.
Key Characteristics: The “5-Second Spinner”
Duration: 5–30 seconds (rarely exceeding 1 minute)
- The spinning is brief and self-limiting
- Episodes resolve quickly once the head is held still
- This short duration is the hallmark feature that distinguishes BPPV from other vertigo types
Triggers: Specific Head Movements
- Turning over in bed (especially rolling to one side)
- Lying down quickly
- Tilting the head back to look up at a ceiling or high shelf
- Bending forward and then straightening up
- Certain yoga or exercise positions
The “Morning Effect”
- Attacks are often most severe in the morning
- During sleep, the crystals may agglomerate (clump together), creating a larger mass that has a higher impact on balance sensors when you first move
- This is why BPPV patients often report, “Every morning, when I roll over, the room spins for 20 seconds”
Associated Symptoms:
- Nausea is common but usually mild because the episode is so brief
- No hearing loss
- No ear pain
- No neurological deficits (no weakness, slurred speech, or double vision)
Why BPPV Matters: The “Curable” Condition
BPPV is the only vertigo condition that can be permanently cured through a simple physical maneuver.
Epley Maneuver (Canalith Repositioning Procedure):
- A series of slow, controlled head movements that use gravity to guide the crystals out of the semicircular canal and back into the utricle where they belong
- Success rate: 70–90% after a single session
- Takes approximately 10–15 minutes to perform
Semont Maneuver:
- An alternative repositioning maneuver with similar efficacy
Why This Matters for Your Health:
Because BPPV is so common, it is frequently misdiagnosed as general weakness, low blood pressure, or even a vascular issue. Patients then undergo:
- Unnecessary brain MRI scans (costing money and time)
- Unnecessary medications (anti-dizziness drugs that may cause drowsiness)
- Years of missed opportunities for curative treatment
If you have brief, position-triggered vertigo lasting seconds, ask your ENT or neurologist specifically about the Dix-Hallpike maneuver (a diagnostic test) and the Epley maneuver (the cure). This single intervention can end your suffering.
Condition 2: Vestibular Neuritis – The “Prolonged” Spin (Days to Weeks)
What Is Vestibular Neuritis?
Vestibular Neuritis (also called acute unilateral vestibulopathy) is the second most frequent cause of peripheral vertigo. Unlike BPPV, which comes in brief attacks, this condition involves a sudden and sustained failure of the balance nerve on one side.
The Viral Culprit
Vestibular neuritis is believed to be caused by a viral or post-viral infection of the vestibular nerve. It often follows a cold, flu, or other respiratory infection by a few days to a week. The virus causes inflammation and swelling of the vestibular nerve (CN VIII), disrupting its ability to send balanced signals to the brain.
When one side of the vestibular system suddenly fails, the intact side sends unopposed signals to the brain. The brain interprets this asymmetry as if the head is spinning continuously—similar to what would happen if you spun around rapidly for 30 seconds and then stopped abruptly. The sensation of spinning persists until the brain adapts (compensation) and the inflammation resolves.
Key Characteristics: The “Multi-Day Spinner”
Duration: Hours to Days (sometimes weeks)
- The vertigo is violent and continuous, not brief
- It reaches peak intensity within 6–24 hours of onset
- It gradually improves over 2–4 weeks, with most recovery within the first 2 weeks
- Some patients report residual imbalance or motion sensitivity for months
Movement Sensitivity:
- While the spinning is constant, it is severely exacerbated by any head movement
- Patients typically lie as still as possible to minimize symptoms
- This is in stark contrast to BPPV, where symptoms depend on specific movements
Associated Symptoms:
- Nausea and vomiting (often severe due to prolonged nature)
- No hearing loss (this is crucial for diagnosis)
- No ear pain
- No facial weakness, slurred speech, or double vision (distinguishes it from stroke)
Physical Examination Findings:
- Abnormal head impulse test (HIT): The eyes move away from the target as the head turns, and a catch-up saccade is required to refixate—this indicates vestibular nerve damage
- Unidirectional nystagmus: Involuntary eye movements that beat in a consistent direction
- Mild skew deviation may be present but typically not severe
Why Vestibular Neuritis Matters: The “Movement Is Medicine” Paradox
The treatment approach for vestibular neuritis seems counterintuitive:
Acute Phase (First 1–2 weeks):
- Short course of corticosteroids (e.g., prednisolone) to reduce nerve inflammation and improve recovery
- Anti-emetics (anti-nausea medications like ondansetron) to control severe vomiting
- Rest and reassurance
Recovery Phase (After 1–2 weeks):
- Gradual mobilization and movement is encouraged
- vestibular rehabilitation exercises help the brain “relearn” balance despite the damaged nerve
- Long-term vestibular suppressants (like meclizine) should be avoided because they actually slow the brain’s ability to compensate for the nerve damage
Why This Matters:
Many patients with vestibular neuritis are told to rest for weeks or are prescribed long-term anti-dizziness medications. This approach delays recovery. The brain’s natural ability to compensate (vestibular compensation) is activated by movement and challenge. Early mobilization, even when uncomfortable, promotes faster recovery.
If you are diagnosed with vestibular neuritis, ask your doctor about:
- A referral to vestibular rehabilitation therapy (physical therapy specifically for balance disorders)
- The timeline for gradual return to activity
- Whether long-term medication use is appropriate for your situation
Condition 3: Posterior Circulation Stroke – The “Dangerous” Mimic (Sudden, Persistent)
The Stroke That Looks Like Vestibular Neuritis
Between 4% and 15% of patients who arrive at an emergency department with continuous vertigo are actually having a stroke in the brainstem or cerebellum. This is the most dangerous “chakkar” because it can present with symptoms nearly identical to vestibular neuritis.
What Happens in a Stroke
A stroke occurs when blood flow to a region of the brain is interrupted. The balance centers of the brain are located in the brainstem (especially the medulla and pons) and the cerebellum. These regions are supplied by the vertebral and basilar arteries (the “posterior circulation”).
When a blood clot blocks one of these arteries, the affected region of the brain becomes starved of oxygen (ischemia). Because the brainstem is densely packed with critical pathways—each controlling different functions (balance, eye movement, swallowing, speech, motor control)—even a small stroke can cause isolated vertigo that mimics an inner ear infection.
Key Characteristics: Red Flags of Dangerous “Chakkar”
Duration: Sudden Onset, Persistent
- Vertigo appears suddenly, often without warning
- It is continuous and does not resolve with rest or movement
- Unlike vestibular neuritis, it does not follow a predictable improvement curve
Associated Symptoms (The “Red Flags”):
- Double vision (diplopia)
- Slurred speech (dysarthria)
- Difficulty swallowing (dysphagia)
- Weakness or numbness in limbs (especially asymmetric)
- Severe imbalance where the patient cannot sit or stand unassisted (truncal ataxia)
- Facial drooping
- Loss of consciousness or altered mental status
Sudden Hearing Loss + Vertigo = DANGER:
- If severe vertigo is accompanied by sudden hearing loss in one ear, it may indicate an infarction of the Anterior Inferior Cerebellar Artery (AICA) territory
- This artery supplies both the inner ear (cochlea) and the brainstem
- This combination is a classic presentation of brainstem stroke and demands immediate neuroimaging
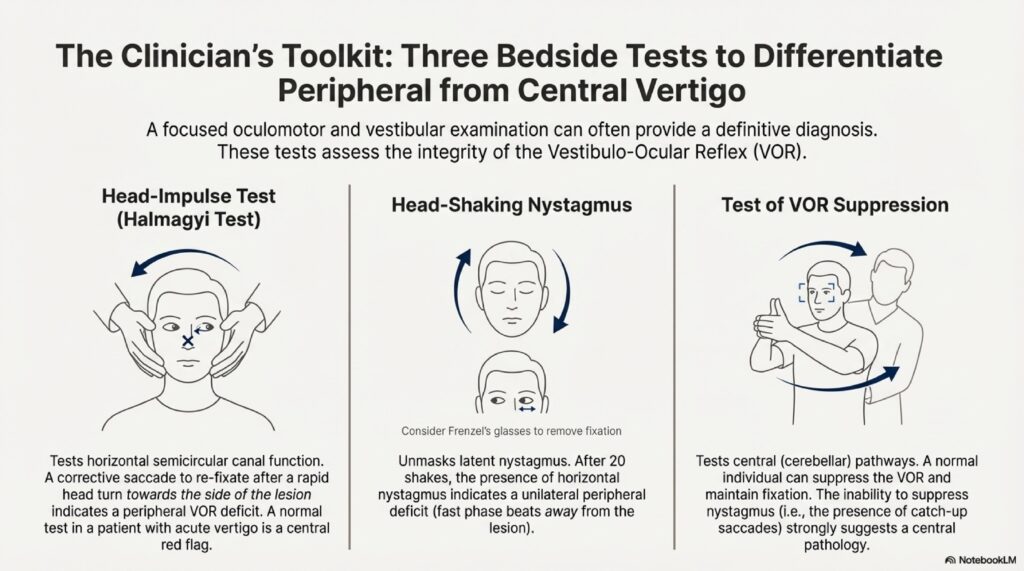
Why the HINTS Exam Matters: Detecting Stroke in 60 Seconds
The HINTS protocol (Head Impulse, Nystagmus, Test of Skew) is a three-step bedside examination that is more accurate than early MRI at detecting brainstem strokes in the first 48 hours. Understanding what doctors are looking for helps you advocate for proper evaluation.
Step 1: Head Impulse Test (HIT)
What the Doctor Does:
- You fixate on a target (usually the examiner’s nose or a mark on the wall)
- The examiner rapidly rotates your head 10–20 degrees to one side
- The examiner watches your eyes to see if they remain fixed on the target or require a catch-up movement
BPPV or Vestibular Neuritis Finding (Inner Ear Problem):
- Your eyes move away from the target as your head turns
- Your eyes require a quick catch-up saccade to return to the target
- This is an abnormal but reassuring finding because it indicates the inner ear or nerve is damaged, not the brain
Stroke Finding (Brainstem Problem):
- Your eyes remain fixed on the target despite the head movement
- No catch-up saccade is needed
- This is a major red flag because it means your inner ear is intact (normal reflex), but your brain’s integration is damaged
Critical Clinical Pearl: A normal HIT + continuous vertigo = high suspicion for stroke.
Step 2: Nystagmus Pattern
What the Doctor Does:
- The examiner observes your eyes as you gaze straight ahead, then to the right, then to the left
- The examiner specifically looks at the pattern of involuntary eye movements (nystagmus)
BPPV or Vestibular Neuritis Finding (Inner Ear Problem):
- Nystagmus is unidirectional—it always beats in the same direction regardless of where you look
- For example, if your right vestibular nerve is damaged, nystagmus may always beat to the left (away from the damaged side)
Stroke Finding (Brainstem Problem):
- Nystagmus is direction-changing—it beats to the right when you look right and to the left when you look left
- Or, nystagmus is purely vertical or rotatory (twisted), which is almost never seen in peripheral vertigo
- Vertical nystagmus is virtually pathognomonic (uniquely characteristic) of brainstem or cerebellar stroke
Step 3: Test of Skew (Vertical Eye Alignment)
What the Doctor Does:
- You fixate on a target while looking straight ahead
- The examiner covers one eye at a time, observing for vertical misalignment
- If one eye is higher than the other, the uncovered eye will jump up or down when the cover is removed to refixate
BPPV or Vestibular Neuritis Finding (Inner Ear Problem):
- Your eyes remain vertically aligned
- No corrective eye movements are necessary
Stroke Finding (Brainstem Problem):
- One eye is positioned higher than the other (skew deviation)
- When the cover is removed, the misaligned eye jumps to refixate
- Skew deviation is highly specific for brainstem lesions and strongly suggests stroke
Why Stroke Matters: The Critical Treatment Window
A patient presenting with what looks like vestibular neuritis but who actually has a brainstem stroke faces potentially catastrophic consequences:
- Cerebellar swelling can lead to increased intracranial pressure, coma, or death
- Brainstem infarction can impair vital functions like breathing and heart rate regulation
- Early intervention with thrombolysis (clot-busting drugs) or thrombectomy (mechanical clot removal) can prevent permanent disability or death
The window for thrombolysis is 4.5 hours from symptom onset. The window for thrombectomy can extend to 24 hours in some cases. Missing the diagnosis wastes these critical windows.
Comparison Table: BPPV vs. Vestibular Neuritis vs. Stroke
| Feature | BPPV | Vestibular Neuritis | Posterior Circulation Stroke |
|---|---|---|---|
| Duration | Seconds (< 1 min) | Days to Weeks | Persistent/Sudden |
| Triggers | Specific head movements | Spontaneous (always present) | Spontaneous |
| Character | Brief, self-limiting | Violent, continuous | Severe, variable |
| Hearing Loss | None | None | Possible (AICA territory) |
| Slurred Speech/Double Vision | None | None | Often present |
| Balance Ability | Mild imbalance | Veering to one side | Profound ataxia (cannot sit) |
| Head Impulse Test | Abnormal (catch-up saccade) | Abnormal (catch-up saccade) | Normal (no catch-up) |
| Nystagmus Pattern | Unidirectional | Unidirectional | Direction-changing or vertical |
| Skew Deviation | Absent or mild | Absent or mild | Often present |
| Treatment | Epley/Semont maneuver | Corticosteroids, vestibular rehab | Thrombolysis/Thrombectomy |
| Prognosis | Excellent (curable) | Good (recovery in weeks) | Variable (depends on severity) |
Why “Chakkar” Isn’t Enough: The Blunderbuss Diagnosis Problem
If you simply tell your doctor, “Doctor, mujhe chakkar aata hai,” you risk receiving a “blunderbuss” investigation—a generic series of tests that may miss the specific cause and waste time and money.
Examples of Misdiagnosis:
Orthostatic Hypotension Misdiagnosed as BPPV:
- A patient reports dizziness only when standing up (orthostatic hypotension due to blood pressure drops)
- The doctor prescribes BPPV treatment, which is ineffective
- Correct diagnosis requires measuring blood pressure lying and standing, and adjusting medications or sodium intake
vestibular migraine Misdiagnosed as Menière’s Disease:
- A patient has episodes of vertigo lasting 4–6 hours with nausea
- Menière’s disease is suspected and salt restriction is recommended
- In reality, the patient has vestibular migraine, which requires lifestyle changes, migraine-specific medications (e.g., triptans), and migraine prevention
- Salt restriction is ineffective
Anxiety-Induced Dizziness Treated as Stroke:
- A patient with generalized anxiety disorder reports feeling faint and dizzy
- Extensive brain imaging is performed unnecessarily
- Cognitive behavioral therapy and anxiety management are the appropriate treatments
Your Tool: The Vertigo Diary—Track to Diagnose
To help your doctor make the correct diagnosis, start a Vertigo Diary immediately after an episode. Document the following details:
Vertigo Diary Checklist (Printable/Digital Format)
Episode #: _ | Date: ___ | Time: _
1. What Did You Feel?
- ☐ Spinning sensation (everything rotating)
- ☐ Swaying or tilting sensation
- ☐ Lightheadedness or faintness
- ☐ Unsteadiness or imbalance
- ☐ Other: ___
2. How Long Did It Last?
- ☐ Seconds (< 1 minute)
- ☐ Minutes (1–5 minutes)
- ☐ 5–30 minutes
- ☐ 30 minutes to 1 hour
- ☐ Hours
- ☐ Days or longer
3. What Triggered It?
- ☐ Specific head movement (rolling in bed, looking up, etc.)
- ☐ Standing up from sitting/lying down
- ☐ Sudden head turn
- ☐ No clear trigger (spontaneous)
- ☐ Stress or anxiety
- ☐ Other: ___
4. Associated Symptoms (Check All That Apply):
- ☐ Nausea
- ☐ Vomiting
- ☐ Ear pain
- ☐ Hearing loss or ringing in ears (tinnitus)
- ☐ Double vision
- ☐ Slurred speech
- ☐ Difficulty swallowing
- ☐ Weakness in limbs
- ☐ Facial drooping
- ☐ Headache (where? __)
- ☐ Severe imbalance (cannot sit/stand alone)
5. Recovery:
- ☐ Immediate (as soon as movement stopped)
- ☐ Within 10–15 minutes
- ☐ Within 1 hour
- ☐ Within several hours
- ☐ Gradual improvement over days/weeks
6. What Made It Better/Worse?
- Made Better: ___
- Made Worse: ___
7. Your Position When It Started:
- ☐ In bed
- ☐ Sitting
- ☐ Standing
- ☐ During activity/exercise
- ☐ At rest
Additional Notes:
(Any other details that seemed relevant: recent illness, medications, stress, etc.)
Why the Vertigo Diary Matters
When you bring this diary to your appointment at PRIME ENT Center Hardoi, it provides your doctor with:
- Objective data (not just memory)
- Pattern recognition (if episodes cluster or follow a trigger)
- Red flag identification (if you’ve documented neurological symptoms)
- Accurate severity assessment (duration and associated symptoms guide treatment urgency)
Submit the diary to your clinic before your appointment if possible, so the doctor has time to review it and come prepared with specific diagnostic tests.
When to Go to the Emergency Department vs. Urgent Clinic
GO TO THE EMERGENCY DEPARTMENT IMMEDIATELY IF:
- First-ever episode of continuous vertigo lasting > 1 hour
- Vertigo + double vision, slurred speech, difficulty swallowing, or weakness
- Severe imbalance (cannot sit or stand without assistance)
- Vertigo + severe headache, especially at the back of the head
- Vertigo + sudden hearing loss
- Progressive worsening over hours
- Loss of consciousness or confusion
SCHEDULE AN URGENT APPOINTMENT AT PRIME ENT CENTER HARDOI (24–48 HOURS) IF:
- Brief, position-triggered vertigo lasting seconds (likely BPPV)
- Stable, gradual-onset vertigo with normal neurological examination
- Recurrent episodes of known vertigo type
- Vertigo with ear discharge or hearing loss (but stable condition)
- Pediatric vertigo with normal examination
Key Takeaways: Stop the Misdiagnosis
- “Chakkar” is too vague. Describe your spinning sensation, its duration, and its triggers.
- Brief vertigo (seconds) triggered by head position = BPPV. Seek the Epley maneuver—it cures you.
- Continuous vertigo (days) without other symptoms = Vestibular NeuritisCommon Symptoms of Vertigo. Expect corticosteroids and vestibular rehabilitation.
- Vertigo with neurological symptoms (double vision, slurred speech, weakness) = Possible Stroke. Go to the emergency department immediately.
- Use a Vertigo Diary to track patterns and provide your doctor with accurate diagnostic information.
- The HINTS exam (head impulse, nystagmus, skew deviation) can identify stroke at the bedside in 60 seconds, faster than MRI.
Contact PRIME ENT Center Hardoi
For Urgent Diagnosis and Management:
- Address: PRIME ENT Center, Hardoi (241001)
- Specialists: Dr. Prateek Porwal, VAI Budapest 2025 International Award Winner, Dr. Harshita Singh
When calling, mention:
- Your vertigo diary observations
- Duration and triggers of your symptoms
- Any red flag symptoms (double vision, slurred speech, hearing loss)
HINGLISH VERSION
Stop Calling Everything “Chakkar”: Teeno Conditions Ko Samjho Jo Dikhte Bilkul Same Hain
“Chakkar” Shabd Itna Vague Kyun Hai?
Jab patient hospital jaata hai aur bolte hain, “Doctor, mujhe chakkar aata hai,” toh doctor ko samajh nahi aata ke matlab kya hai. Chakkar—Hindi/Urdu mein dizziness—kuch bhi matlab sakta hai: spinning, fainting, confusion, imbalance, ya bas ek halkapa sa vague feel.
Iska comparison aisa hai: Ek car owner mechanic se bolte hain, “Mere car se sound aaa raha hai.” Mechanic ne poocha nahi, toh fix nahi kar sakte. Kya squealing sound hai (belt problem)? Grinding sound (brake)? Knocking (engine)?
Tabhi doctor ko bhi nahi pata: Tu real mein kya feel kar raha? Kitne der tak? Kya trigger tha?
Ismein 3 serious conditions hain jo bilkul same dikhte hain lekin completely alag treatment chahiye:
- BPPV – mechanical, seconds mein over
- Vestibular Neuritis – viral, days mein last
- Posterior Circulation Stroke – life-threatening, sudden
Condition 1: BPPV – “5-Second Chakkar” (Seconds)
BPPV Matlab Kya?
BPPV = Benign Paroxysmal Positional Vertigo
Matlab: Benign (safe), Paroxysmal (sudden attacks), Positional (head position se trigger), Vertigo (spinning).
Yeh most common cause of vertigo hai—20–25% cases BPPV ke hote hain.
Crystal Problem
Kaan ke andar inner ear mein tiny calcium crystals hote hain (otoconia). Normally ye crystals ek specific spot pe hote hain jo gravity detect karti hai.
BPPV mein: Ye crystals apni jagah se nikl jaate hain aur semicircular canal (rotation-detector tubes) mein chle jaate hain.
Jab head move karte ho, crystals flow karti hain aur false signal bhejti hain brain ko: “Arre, tu ghumta ja raha hai!”
Lekin reality mein tu bilkul still hai. Bas dimag ko wrong information mil rahi hai.
Key Features: “The Seconds Spinner”
Duration: 5–30 seconds (rarely 1 minute)
- Bilkul brief
- Jaise hi head stop karte ho, chakkar band
Triggers: Specific Head Movements Only
- Bed se roll over karte ho
- Lie down karte ho
- Ceiling dekh-ne ke liye head tilt back
- Bending and straightening
- Specific yoga positions
“Morning Effect”
- Subah worst hota hai kyunke crystals overnight “clump” ho jaati hain
- Subah jab roll over karte ho: 20 seconds chakkar, phir normal
Symptoms:
- Mild nausea (kyunke itni brief hai)
- No hearing loss
- No pain in ear
- No double vision, no slurred speech
Why BPPV Matters: Yeh Cure Ho Sakta Hai!
Epley Maneuver:
- Simple head movements jo crystals ko wapas utricle mein guided karti hain
- 70–90% cases mein kaam karti hai
- 10–15 minutes mein done
Real problem: Aksar BPPV ko mistake se “weakness” ya “low BP” samjh jaate hain. Phir:
- Unnecessary MRI
- Unnecessary medicines
- Years suffering without real treatment
Agar seconds-chakkar position-triggered, ask for Epley maneuver. Bas 15 minutes mein cure!
Condition 2: Vestibular Neuritis – “Days-Long Chakkar” (Days to Weeks)
Vestibular Neuritis Kya Hai?
Second most common peripheral vertigo.
BPPV ke opposite—yeh continuous, prolonged, severe hota hai.
Viral Nerve Problem
Vestibular neuritis = kaan ki balance nerve ko virus se infection.
Usually cold ya flu ke baad 3–7 days mein aata hai.
Virus nerve ko swell kar deti hai → signal asymmetry → brain sochta hai ke tum ghumte ja rahe ho → continuous chakkar.
Key Features: “Days-Long Spinner”
Duration: Hours to Weeks (peak in 24 hours)
- Violent aur continuous
- Gradually improve over 2–4 weeks
- First 2 weeks mein maximum
Movement Se Worse
- Any head movement chakkar ko multiply kar deti hai
- Patients bilkul still padhe rahte hain
- BPPV opposite—BPPV mein specific movement trigger, vestibular neuritis mein every movement bad
Associated Symptoms:
- Severe nausea/vomiting (kyunke prolonged hai)
- NO hearing loss (yeh important!)
- No ear pain
- No facial weakness, no slurred speech (distinguish from stroke)
Doctor Finds:
- Abnormal head impulse test (catch-up saccade hoti hai)
- Unidirectional nystagmus (one direction mein eye jumps)
Why Vestibular Neuritis Matters: Movement Is Medicine
Counterintuitive! Treatment:
First 1–2 weeks:
- Steroids (inflammation reduce karti hain)
- Anti-nausea meds
- Rest
After 1–2 weeks:
- Movement encourage karte hain!
- Vestibular rehab exercises
- Brain ko “relearn” karti hain balance
- Long-term anti-dizziness meds avoid karte hain kyunke brain compensation ko slow kar deti hain
Point: Movement at first uncomfortable lagti hai, lekin brain compensation faster aata hai.
Ask for vestibular rehabilitation therapy (balance physical therapy).
Condition 3: Posterior Circulation Stroke – “Dangerous Chakkar” (Sudden, Persistent)
The Life-Threatening Mimic
4–15% continuous vertigo cases = STROKE
Yeh vestibular neuritis jaisa dikhta hai lekin potentially fatal hai.
Blood Supply Block
Brain ke balance center mein blood supply vertebral aur basilar arteries se aati hai.
Jab clot ban jaata hai, area mein oxygen nahi pauchti → ischemia → brain damage → stroke.
Small stroke bhi isolated vertigo cause kar sakti hai.
Red Flags: Stroke Ke Signs
Agar chakkar + koi bhi ye ho:
- Double vision
- Slurred speech
- Difficulty swallowing
- Weakness/numbness in limbs
- Severe imbalance (can’t sit/stand)
- Facial drooping
- Unconscious hona
SPECIAL: Vertigo + sudden hearing loss ek ear mein = AICA stroke (internal auditory artery) = EMERGENCY
HINTS Exam: 60-Second Stroke Test (Dedicated Section)
Why HINTS Matters
HINTS is 100% accurate in first 48 hours. Early MRI 50% false-negative hota hai!
Step-by-Step HINTS Explained
Step 1: Head Impulse Test (HIT)
Doctor Kya Karti Hai:
- Tum nose ya wall ke mark pe fixate karte ho
- Doctor quickly head ko ek side rotate karti hai (0.5–1 second)
- Doctor dekhti hai: Eyes target pe rahti hain ya move karti hain?
Inner Ear Problem (BPPV/Vestibular Neuritis):
- Eyes move head ke saath target se away
- Phir quick catch-up jump target pe wapas
- Good news! = Ear problem, brain theek
Stroke (Brainstem Problem):
- Eyes bilkul steady target pe
- No catch-up jump
- BAD! = Brain problem, stroke suspect
Key Point: Normal HIT + continuous chakkar = STROKE red flag!
Step 2: Nystagmus (Eye Jump Pattern)
Doctor Dekhti Hai:
- Eyes straight? Right? Left?
- Kaunse direction mein involuntary jumps hain?
Inner Ear:
- Jumps same direction sab jagah (unidirectional)
- E.g., left side damage = hamesha leftward jumps
Stroke:
- Jumps different directions based on gaze (direction-changing)
- Or vertical jumps (up-down)
- Vertical = 99% brain stroke!
Step 3: Test of Skew (Eye Height)
Doctor Dekhti Hai:
- Ek eye cover, phir dusri cover
- Kya ek eye doosri se oonchi hai?
Inner Ear:
- Dono eyes same level
Stroke:
- Ek eye higher than other
- = Brainstem stroke sign
Comparison Table: Teen Conditions
| Feature | BPPV | Vestibular Neuritis | Stroke |
|---|---|---|---|
| Chakkar Duration | Seconds | Days-Weeks | Sudden, persistent |
| Trigger | Head movement | Spontaneous | Spontaneous |
| Nausea | Mild | Severe | Variable |
| Hearing Loss | No | No | Possible |
| Slurred Speech | No | No | Often YES |
| Balance | Mild | Veering | Severe (can’t sit) |
| HIT | Abnormal | Abnormal | NORMAL |
| Nystagmus | Unidirectional | Unidirectional | Direction-changing/vertical |
| Treatment | Epley maneuver | Steroids + rehab | Thrombolysis |
| Cure | Yes | Usually | Depends |
Vertigo Diary: Track Karo, Diagnose Ho Jao
Printable Checklist Format
Episode #: _ | Date: ___ | Time: _
1. What Did You Feel?
- ☐ Spinning
- ☐ Swaying
- ☐ Lightheaded
- ☐ Unsteady
- ☐ Other: _
2. Duration?
- ☐ Seconds
- ☐ Minutes
- ☐ Hours
- ☐ Days
3. Trigger?
- ☐ Specific head movement (rolling, looking up, etc.)
- ☐ Standing up
- ☐ No trigger (spontaneous)
- ☐ Other: _
4. Associated Symptoms?
- ☐ Nausea/Vomiting
- ☐ Ear pain
- ☐ Hearing loss/ringing
- ☐ Double vision ← RED FLAG
- ☐ Slurred speech ← RED FLAG
- ☐ Difficulty swallowing ← RED FLAG
- ☐ Weakness in limbs ← RED FLAG
- ☐ Severe imbalance ← RED FLAG
- ☐ Headache (where?) ← RED FLAG
- ☐ Other: _
5. Recovery?
- ☐ Immediate (few seconds)
- ☐ Minutes
- ☐ Hours
- ☐ Days/Gradual
6. What Made It Better/Worse?
- Better: _
- Worse: _
7. Position When Started?
- ☐ In bed
- ☐ Sitting
- ☐ Standing
- ☐ During activity
Notes: (Recent illness, stress, new medications, etc.)
Emergency vs. Urgent Clinic
STRAIGHT TO EMERGENCY:
- Continuous chakkar > 1 hour (first time)
- Chakkar + double vision, slurred speech, weakness
- Severe imbalance
- Chakkar + severe headache
- Chakkar + sudden hearing loss
- RED FLAG symptoms from diary
PRIME ENT CENTER (24–48 hours):
- Seconds-chakkar, position-triggered
- Stable chakkar, normal exam
- Known BPPV relapse
- Mild dizziness in child, normal neuro
Final Points
- Don’t say “chakkar”—describe timing, triggers, symptoms
- Seconds = BPPV (fixable!)
- Days = Vestibular Neuritis (recover over weeks)
- Sudden + symptoms = Stroke (EMERGENCY!)
- Keep Vertigo Diary
- HINTS exam faster than MRI
PRIME ENT Center Hardoi
Address: Hardoi (241001)
Doctors: Dr. Prateek Porwal, Dr. Harshita Singh
Bring your Vertigo Diary!
HINDI VERSION
“चक्कर” को हर बार Same मत कहो: तीन अलग शर्तें जो एक जैसी लगती हैं
“चक्कर” शब्द बहुत अस्पष्ट है
जब मरीज़ अस्पताल जाता है और कहता है, “डॉक्टर, मुझे चक्कर आता है,” तो डॉक्टर को समझ नहीं आता कि मतलब क्या है।
“चक्कर” माने: घूमना, बेहोशी, भ्रम, असंतुलन, या सिर्फ एक हल्का सा अजीब feel।
मिसाल: गाड़ी के मालिक ने मैकेनिक से कहा, “मेरी कार से sound आ रहा है।” मैकेनिक पूछेगा, “कौन सा sound? Squealing? Grinding? Knocking?”
इसी तरह तीन चीजें हैं जो चक्कर देती हैं पर अलग-अलग:
- BPPV – यांत्रिक, सेकंड में सही
- Vestibular Neuritis – वायरल, दिन भर चलता है
- Stroke – जानलेवा, अचानक
शर्त 1: BPPV – “सेकंड वाला चक्कर”
BPPV क्या है?
BPPV = Benign (सुरक्षित) Paroxysmal (अचानक) Positional (स्थिति-संबंधी) Vertigo (घूमना)
सबसे आम चक्कर—20–25% मामलों में BPPV होता है।
क्रिस्टल की समस्या
कान के अंदर छोटी खोपड़ियां हैं (otoconia)—कैल्शियम के क्रिस्टल जो गुरुत्व को महसूस करते हैं।
BPPV में: ये क्रिस्टल अपनी जगह से निकल जाती हैं और अर्धवृत्ताकार नलिकाओं (semicircular canals) में चली जाती हैं।
जब सिर हिलता है, क्रिस्टल बहती हैं और दिमाग को गलत संदेश भेजती हैं: “तुम घूम रहे हो!”
लेकिन सच में तुम बिल्कुल स्थिर हो। सिर्फ दिमाग को गलत जानकारी मिल रही है।
मुख्य विशेषताएं: “सेकंड का चक्कर”
अवधि: 5–30 सेकंड (कभी 1 मिनट)
- बिल्कुल संक्षिप्त
- सिर को रोकते ही चक्कर बंद
ट्रिगर: केवल विशिष्ट सिर की गतिविधियां
- बिस्तर में पलट जाना
- लेट जाना
- ऊपर की ओर देखने के लिए सिर पीछे झुकाना
- आगे झुकना और सीधा होना
- कुछ योग मुद्राएं
“सुबह का प्रभाव”
- सुबह सबसे बुरा होता है क्योंकि क्रिस्टल रात भर “जमा” हो जाती हैं
- सुबह जब पलटते हो: 20 सेकंड चक्कर, फिर सामान्य
लक्षण:
- हल्की मतली
- श्रवण हानि नहीं
- कान में दर्द नहीं
- दोहरी दृष्टि नहीं, अस्पष्ट बोली नहीं
BPPV महत्वपूर्ण क्यों: यह ठीक हो सकता है!
Epley मैनुवर:
- सरल सिर की गतिविधियां जो क्रिस्टल को वापस सही जगह निर्देशित करती हैं
- 70–90% मामलों में काम करता है
- 10–15 मिनट में पूरा
समस्या: अक्सर BPPV को गलती से “कमजोरी” या “कम BP” समझ जाते हैं। फिर:
- अनावश्यक MRI
- अनावश्यक दवाएं
- वर्षों तक सही उपचार के बिना पीड़ा
अगर सेकंड-चक्कर स्थिति-निर्भर है, Epley मैनुवर मांगो। सिर्फ 15 मिनट में ठीक!
शर्त 2: Vestibular Neuritis – “दिन-भर चक्कर” (दिन से हफ्ते)
Vestibular Neuritis क्या है?
दूसरा सबसे आम peripheral vertigo।
BPPV के विपरीत—यह निरंतर, लंबा, गंभीर होता है।
वायरल नर्व समस्या
Vestibular neuritis = कान की संतुलन नर्व को वायरस से संक्रमण।
आमतौर पर सर्दी या फ्लू के 3–7 दिन बाद आता है।
वायरस नर्व को सूजा देता है → सिग्नल असंतुलन → दिमाग सोचता है कि तुम घूम रहे हो → निरंतर चक्कर।
मुख्य विशेषताएं: “दिन-लंबा चक्कर”
अवधि: घंटे से हफ्ते (24 घंटों में पीक)
- हिंसक और निरंतर
- 2–4 हफ्तों में धीरे-धीरे सुधार
- पहले 2 हफ्तों में अधिकतम
गति से बदतर
- कोई भी सिर की गति चक्कर को कई गुना बदतर कर देती है
- मरीज़ बिल्कुल स्थिर रहते हैं
- BPPV विपरीत—BPPV में विशिष्ट गति ट्रिगर, vestibular neuritis में हर गति बुरी
संबंधित लक्षण:
- गंभीर मतली/उल्टी (क्योंकि लंबा है)
- श्रवण हानि नहीं (यह महत्वपूर्ण है!)
- कान में दर्द नहीं
- चेहरे की कमजोरी नहीं, अस्पष्ट बोली नहीं (स्ट्रोक से अलग करता है)
डॉक्टर पाता है:
- असामान्य हेड इम्पल्स टेस्ट
- एकदिशीय निस्टागमस
Vestibular Neuritis महत्वपूर्ण क्यों: गति दवा है
अप्रत्याशित! उपचार:
पहले 1–2 हफ्ते:
- स्टेरॉयड (सूजन कम करते हैं)
- मतली-विरोधी दवाएं
- आराम
1–2 हफ्तों के बाद:
- गति को प्रोत्साहित करते हैं!
- Vestibular rehabilitations व्यायाम
- दिमाग को “दोबारा सीखाते” हैं
- दीर्घकालीन anti-dizziness दवाएं बचाते हैं क्योंकि वे मस्तिष्क की क्षतिपूर्ति को धीमा करती हैं
बिंदु: शुरुआत में गति असहज लगती है, लेकिन मस्तिष्क की क्षतिपूर्ति तेजी से आती है।
Vestibular rehabilitation therapy (संतुलन physical therapy) मांगो।
शर्त 3: Posterior Circulation Stroke – “खतरनाक चक्कर”
जानलेवा मिमिक
4–15% निरंतर चक्कर मामले = स्ट्रोक
यह Vestibular Neuritis जैसा दिखता है लेकिन संभावित रूप से घातक है।
रक्त की आपूर्ति में बाधा
दिमाग के संतुलन केंद्र को वर्टेब्रल और बेसिलर धमनियों से रक्त की आपूर्ति होती है।
जब थक्का बन जाता है, क्षेत्र को ऑक्सीजन नहीं मिलती → इस्केमिया → मस्तिष्क को नुकसान → स्ट्रोक।
छोटा स्ट्रोक भी अलग-थलग चक्कर दे सकता है।
लाल झंडे: स्ट्रोक के संकेत
अगर चक्कर + कोई भी यह हो:
- दोहरी दृष्टि
- अस्पष्ट बोली
- निगलने में कठिनाई
- अंगों में कमजोरी/सुन्नता
- गंभीर असंतुलन (बैठ/खड़े नहीं हो सकते)
- चेहरा झुक जाना
- बेहोश होना
विशेष: चक्कर + अचानक एक कान में श्रवण हानि = AICA स्ट्रोक = आपातकाल
HINTS परीक्षा: 60-सेकंड स्ट्रोक टेस्ट
HINTS क्यों महत्वपूर्ण है
HINTS पहले 48 घंटों में 100% सटीक है। शुरुआती MRI 50% झूठी नकारात्मक होती है!
चरण-दर-चरण HINTS
चरण 1: हेड इम्पल्स टेस्ट (HIT)
डॉक्टर क्या करती है:
- तुम नाक या दीवार के निशान पर नजर रखते हो
- डॉक्टर जल्दी से सिर को एक ओर घुमाती है
- डॉक्टर देखती है: आँखें लक्ष्य पर रहती हैं या हिलती हैं?
कान की समस्या (BPPV/Vestibular Neuritis):
- आँखें सिर के साथ लक्ष्य से दूर चली जाती हैं
- फिर जल्दी पकड़-अप कूद लक्ष्य पर वापस
- अच्छी खबर! = कान की समस्या, दिमाग ठीक
स्ट्रोक (ब्रेनस्टेम समस्या):
- आँखें बिल्कुल स्थिर लक्ष्य पर
- कोई पकड़-अप कूद नहीं
- बुरा! = दिमाग की समस्या, स्ट्रोक संदिग्ध
मुख्य बिंदु: सामान्य HIT + निरंतर चक्कर = स्ट्रोक लाल झंडा!
चरण 2: निस्टागमस (आँख कूद पैटर्न)
डॉक्टर देखती है:
- आँखें सीधी? दाएं? बाएं?
- कौन सी दिशा में अनैच्छिक कूदें हैं?
कान की समस्या:
- कूदें हर जगह एक दिशा में (एकदिशीय)
- उदाहरण के लिए, बाईं ओर क्षति = हमेशा बायीं ओर की कूदें
स्ट्रोक:
- कूदें दृष्टि के आधार पर विभिन्न दिशाओं में (दिशा-परिवर्तन)
- या ऊर्ध्वाधर कूदें (ऊपर-नीचे)
- ऊर्ध्वाधर = 99% मस्तिष्क स्ट्रोक!
चरण 3: स्केव टेस्ट (आँख की ऊंचाई)
डॉक्टर देखती है:
- एक आँख ढकें, फिर दूसरी
- क्या एक आँख दूसरी से ऊँची है?
कान की समस्या:
- दोनों आँखें एक ही स्तर पर
स्ट्रोक:
- एक आँख दूसरी से ऊँची
- = ब्रेनस्टेम स्ट्रोक संकेत
तुलना तालिका: तीन शर्तें
| विशेषता | BPPV | Vestibular Neuritis | Stroke |
|---|---|---|---|
| अवधि | सेकंड | दिन-हफ्ते | अचानक, निरंतर |
| ट्रिगर | सिर की गति | अचानक | अचानक |
| मतली | हल्की | गंभीर | चर |
| श्रवण हानि | नहीं | नहीं | संभव |
| अस्पष्ट बोली | नहीं | नहीं | अक्सर हाँ |
| संतुलन | हल्का | एक ओर झुकना | गंभीर |
| HIT | असामान्य | असामान्य | सामान्य |
| निस्टागमस | एकदिशीय | एकदिशीय | दिशा-परिवर्तन/ऊर्ध्वाधर |
| उपचार | Epley मैनुवर | स्टेरॉयड + rehabilitations | Thrombolysis |
| उपचार | हाँ | आमतौर पर | निर्भर करता है |
वर्टिगो डायरी: ट्रैक करो, निदान हो जाओ
प्रिंट करने योग्य चेकलिस्ट प्रारूप
प्रकरण #: _ | तारीख: ___ | समय: _
1. तुमने क्या महसूस किया?
- ☐ घूमना
- ☐ झूलना
- ☐ हल्कापन
- ☐ असंतुलन
- ☐ अन्य: _
2. अवधि?
- ☐ सेकंड
- ☐ मिनट
- ☐ घंटे
- ☐ दिन
3. ट्रिगर?
- ☐ विशिष्ट सिर की गति (पलटना, ऊपर देखना, आदि)
- ☐ खड़े होना
- ☐ कोई ट्रिगर नहीं (अचानक)
- ☐ अन्य: _
4. संबंधित लक्षण?
- ☐ मतली/उल्टी
- ☐ कान में दर्द
- ☐ श्रवण हानि/घंटी
- ☐ दोहरी दृष्टि ← लाल झंडा
- ☐ अस्पष्ट बोली ← लाल झंडा
- ☐ निगलने में कठिनाई ← लाल झंडा
- ☐ अंगों में कमजोरी ← लाल झंडा
- ☐ गंभीर असंतुलन ← लाल झंडा
- ☐ सिरदर्द (कहाँ?) ← लाल झंडा
- ☐ अन्य: _
5. रिकवरी?
- ☐ तुरंत (कुछ सेकंड)
- ☐ मिनट
- ☐ घंटे
- ☐ दिन/धीरे-धीरे
6. क्या बेहतर/बदतर बनाया?
- बेहतर: _
- बदतर: _
7. शुरुआत करते समय स्थिति?
- ☐ बिस्तर में
- ☐ बैठा हुआ
- ☐ खड़े
- ☐ गतिविधि के दौरान
नोट्स: (हाल की बीमारी, तनाव, नई दवाएं, आदि)
आपातकाल vs. जरूरी क्लिनिक
सीधे आपातकाल:
- निरंतर चक्कर > 1 घंटा (पहली बार)
- चक्कर + दोहरी दृष्टि, अस्पष्ट बोली, कमजोरी
- गंभीर असंतुलन
- चक्कर + गंभीर सिरदर्द
- चक्कर + अचानक श्रवण हानि
- डायरी से लाल झंडे
PRIME ENT CENTER (24–48 घंटे):
- सेकंड-चक्कर, स्थिति-निर्भर
- स्थिर चक्कर, सामान्य परीक्षा
- ज्ञात BPPV पुनरावृत्ति
- बच्चे में हल्का चक्कर, सामान्य न्यूरो
अंतिम बिंदु
- “चक्कर” मत कहो—समय, ट्रिगर, लक्षणों का वर्णन करो
- सेकंड = BPPV (ठीक करने योग्य!)
- दिन = Vestibular Neuritis (हफ्तों में रिकवर)
- अचानक + लक्षण = स्ट्रोक (आपातकाल!)
- वर्टिगो डायरी रखो
- HINTS परीक्षा MRI से तेजी
PRIME ENT Center Hardoi
फोन: [संपर्क संख्या]
पता: Hardoi (241001)
डॉक्टर: Dr. Prateek Porwal, Dr. Harshita Singh
अपनी वर्टिगो डायरी लाओ!
VERTIGO DIARY CHECKLIST
(Downloadable Format for Print/Digital Use)
📋 VERTIGO SYMPTOM TRACKER – Chakkar Ko Track Karo
Purpose: Document your vertigo episodes to help your doctor diagnose the exact cause. Fill this out immediately after each episode.
EPISODE DETAILS
| Field | Your Response |
|---|---|
| Episode Number | _ |
| Date | _ |
| Time of Day | _ |
| Your Age/Sex | _ |
QUESTION 1: What Exactly Did You Feel?
(Select one that best describes)
- ☐ Spinning sensation – Everything rotating around me
- ☐ Tilting/Swaying sensation – World tilting or swaying side-to-side
- ☐ Lightheadedness – Feeling faint or about to lose consciousness
- ☐ General unsteadiness – Difficulty with balance, veering to one side
- ☐ Floating sensation – Feeling disconnected from ground
- ☐ Other (describe): _____________________
QUESTION 2: How Long Did It Last?
(Select one)
- ☐ Seconds (less than 1 minute) — LIKELY BPPV
- ☐ 1–5 minutes
- ☐ 5–30 minutes
- ☐ 30 min to 1 hour
- ☐ Several hours
- ☐ All day or longer
- ☐ Days or weeks (prolonged) — LIKELY VESTIBULAR NEURITIS
QUESTION 3: What Triggered It?
(Select all that apply)
Position/Movement Triggers (BPPV):
- ☐ Rolling over in bed
- ☐ Lying down quickly
- ☐ Tilting head back (looking up/ceiling)
- ☐ Bending forward then straightening up
- ☐ Specific yoga/exercise pose
- ☐ Turning head to one side
Spontaneous (No Clear Trigger):
- ☐ Came on suddenly while sitting still
- ☐ Woke up with it (morning)
- ☐ Started while standing/walking
Other Triggers:
- ☐ Standing up quickly (orthostatic)
- ☐ Stress or anxiety
- ☐ Certain food/drink
- ☐ Loud sounds
- ☐ Unknown trigger
QUESTION 4: Associated Symptoms
(Check ALL that apply — Pay special attention to RED FLAG symptoms)
General Symptoms:
- ☐ Nausea
- ☐ Vomiting
- ☐ Sweating
Ear-Related:
- ☐ Ear pain
- ☐ Hearing loss (sudden, which ear? _)
- ☐ Ringing/buzzing in ears (tinnitus)
- ☐ Ear discharge
Vision-Related ← POTENTIAL RED FLAGS:
- ☐ Double vision (diplopia)
- ☐ Blurred vision
- ☐ Difficulty focusing
Speech/Swallowing ← RED FLAGS:
- ☐ Slurred speech
- ☐ Difficulty swallowing (dysphagia)
- ☐ Hoarseness
Neurological ← RED FLAGS:
- ☐ Weakness in arm(s)
- ☐ Weakness in leg(s)
- ☐ Numbness or tingling (where? _)
- ☐ Facial drooping
- ☐ Difficulty walking in straight line
- ☐ Severe imbalance (cannot sit/stand alone)
Pain/Other:
- ☐ Headache (location? _)
- ☐ Neck/back pain
- ☐ Shortness of breath
- ☐ Chest pain
- ☐ Loss of consciousness
⚠️ IF ANY RED FLAG SYMPTOMS ARE CHECKED: GO TO EMERGENCY IMMEDIATELY
QUESTION 5: What Made It Better?
(Select all that apply)
- ☐ Lying still
- ☐ Staying in one position
- ☐ Movement/activity
- ☐ Closing eyes
- ☐ Opening eyes
- ☐ Specific head position (which? _)
- ☐ Medication (which? __)
- ☐ Time passing (it resolved naturally)
- ☐ Nothing helped (lasted until it passed)
QUESTION 6: What Made It Worse?
(Select all that apply)
- ☐ Any head movement
- ☐ Standing up
- ☐ Lying down
- ☐ Turning to one side (which? L/R)
- ☐ Looking up
- ☐ Specific movements (which? __)
- ☐ Lights
- ☐ Loud sounds
- ☐ Stress
- ☐ Nothing obvious made it worse
QUESTION 7: Recovery Pattern
(Select one)
- ☐ Immediate – Stopped as soon as I stopped moving (BPPV sign)
- ☐ Within 10–15 minutes
- ☐ Within 1 hour
- ☐ Several hours
- ☐ Next day
- ☐ Gradual improvement over days/weeks (VESTIBULAR NEURITIS sign)
- ☐ Still ongoing ← SEEK MEDICAL HELP
QUESTION 8: Your Position When It Started
- ☐ In bed
- ☐ Getting out of bed
- ☐ Sitting at desk/table
- ☐ Standing
- ☐ Walking
- ☐ During exercise/activity
- ☐ Other: _
QUESTION 9: Recent Medical History
(May be relevant)
- ☐ Recent cold/flu/respiratory infection
- ☐ Recent head injury/trauma
- ☐ New medication started (which? _)
- ☐ Recent stress or anxiety
- ☐ Sleep deprivation
- ☐ Alcohol consumption
- ☐ Recent change in blood pressure
- ☐ None of these
ADDITIONAL NOTES
Anything else that seemed important or unusual:
QUICK DIAGNOSTIC HINTS:
| Pattern | Likely Condition |
|---|---|
| Seconds + specific head movement trigger | BPPV → Epley maneuver |
| Days + spontaneous + no neurological symptoms | Vestibular Neuritis → Steroids + rehab |
| Sudden + neurological symptoms (double vision, slurred speech, weakness) | STROKE → EMERGENCY |
WHAT TO DO WITH THIS DIARY:
- Fill it out immediately after each episode (while details are fresh)
- Keep all copies together (bring them to your appointment)
- If RED FLAG symptoms appear, go to emergency immediately (don’t wait for appointment)
- Share with your doctor before your visit if possible—helps them prepare specific tests
- Update after each new episode to see if patterns emerge
📞 SUBMIT TO PRIME ENT CENTER HARDOI BEFORE YOUR APPOINTMENT
Call ahead and mention you have a completed Vertigo Diary. Dr. Prateek Porwal and Dr. Harshita Singh will review it to provide faster, more accurate diagnosis.
FAQs
>
ENGLISH FAQs (20 Questions)
1. What is the main difference between BPPV and vestibular neuritis?
Answer: BPPV causes brief spinning (seconds to a minute) triggered by specific head movements, usually resolving quickly. Vestibular neuritis causes prolonged, continuous spinning (days to weeks) that comes on suddenly without positional triggers. BPPV is cured by the Epley maneuver; vestibular neuritis resolves with steroids, anti-nausea medications, and vestibular rehabilitation. Duration is the key differentiator.
2. Why is my doctor checking my eyes during a vertigo assessment?
Answer: Eye movements reveal where the problem is located. In the HINTS exam, doctors observe the head impulse test (whether eyes follow smoothly), nystagmus (involuntary eye movements), and skew deviation (vertical eye misalignment). These findings distinguish between inner ear problems (peripheral) and brainstem/cerebellar problems (central/stroke).
3. What is the Epley maneuver and how does it work?
Answer: The Epley maneuver is a series of slow, controlled head and body positions that use gravity to guide dislodged crystals (otoconia) out of the semicircular canal and back into the utricle where they belong. It takes 10–15 minutes and has a 70–90% success rate in curing BPPV with a single session. The maneuver must be performed by a trained healthcare provider.
4. Can I do the Epley maneuver at home myself?
Answer: While some modified versions exist for home use, the initial Epley maneuver should ideally be performed by a trained ENT specialist, neurologist, or physical therapist. They can confirm BPPV diagnosis with the Dix-Hallpike test before performing the maneuver, ensure proper positioning, and verify success. Improper technique can be ineffective or uncomfortable.
5. If I have brief positional vertigo, does that definitely mean I have BPPV?
Answer: Not necessarily. While BPPV is the most common cause of brief positional vertigo, other conditions can mimic it, including superior semicircular canal dehiscence (a bony defect), perilymphatic fistula, or even psychiatric dizziness. However, a positive Dix-Hallpike test and successful response to the Epley maneuver strongly support BPPV diagnosis.
6. What should I expect during vestibular neuritis recovery?
Answer: Recovery typically follows this pattern: (1) Peak vertigo in first 24 hours; (2) Gradual improvement over 2–4 weeks, with most recovery in the first 1–2 weeks; (3) Residual imbalance or motion sensitivity may persist for weeks to months. Early movement and vestibular rehabilitation exercises accelerate recovery. Long-term vestibular suppressants should be avoided as they slow the brain’s compensation process.
7. Why are vestibular suppressants discouraged in vestibular neuritis recovery?
Answer: Vestibular suppressants (like meclizine) mask symptoms but actually delay the brain’s ability to compensate for the damaged vestibular nerve. The brain learns balance through movement and challenge. Early mobilization, even when uncomfortable, promotes faster compensation. Suppressing symptoms prevents this adaptive process, prolonging disability.
8. Can I develop BPPV again after the Epley maneuver?
Answer: Yes. While the Epley maneuver cures an episode by repositioning the crystals, BPPV can recur if crystals dislodge again. Recurrence rates are approximately 30% within 5 years. This is why BPPV is called “benign”—it is not dangerous, and recurrent episodes can be retreated with another Epley maneuver.
9. What is the most important feature that distinguishes vertigo caused by stroke from other causes?
Answer: The presence of neurological symptoms accompanying continuous vertigo is the strongest indicator of possible stroke. These include double vision, slurred speech, difficulty swallowing, weakness or numbness in limbs, severe ataxia (inability to sit or stand unassisted), and facial drooping. Any combination of continuous vertigo plus one of these symptoms demands emergency evaluation.
10. What does “direction-changing nystagmus” mean and why is it important?
Answer: Direction-changing nystagmus means involuntary eye movements that change direction based on where the patient looks—they beat to the right when looking right and to the left when looking left. This pattern is highly suggestive of brainstem or cerebellar involvement and is a red flag for stroke. Peripheral (inner ear) causes produce unidirectional nystagmus that beats in the same direction regardless of gaze.
11. How accurate is the HINTS exam for detecting stroke?
Answer: The HINTS exam has 100% sensitivity and 96% specificity for detecting acute brainstem strokes in the emergency setting within the first 48 hours. This makes it more accurate than early MRI, which can be false-negative in up to 50% of small brainstem strokes. The HINTS exam uses only eye movements and takes 60 seconds.
12. What is the critical time window for stroke treatment after symptom onset?
Answer: The window for thrombolysis (clot-busting medications like tPA) is 4.5 hours from symptom onset. The window for mechanical thrombectomy (clot removal via catheter) extends to 24 hours in some cases, depending on brain imaging findings and criteria. After these windows close, the treatment options become limited. This is why rapid diagnosis is critical.
13. If I have sudden vertigo and sudden hearing loss, what does that suggest?
Answer: The combination of sudden vertigo and sudden unilateral sensorineural hearing loss suggests possible infarction of the Anterior Inferior Cerebellar Artery (AICA), which supplies both the inner ear and the brainstem. This is a red flag for posterior circulation stroke and mandates immediate neuroimaging and stroke evaluation.
14. What is the difference between a Vertigo Diary and a medical consultation?
Answer: A Vertigo Diary is a self-recorded log of your symptoms—duration, triggers, associated symptoms, and recovery. A medical consultation involves a doctor’s physical examination, HINTS test, and diagnostic tests (hearing tests, imaging). The diary provides objective data that helps the doctor make faster, more accurate diagnoses. It is a complementary tool, not a replacement for professional evaluation.
15. Can anxiety cause vertigo that mimics peripheral or central causes?
Answer: Yes. Anxiety-related dizziness can present as vague unsteadiness or lightheadedness, and severe anxiety can occasionally trigger brief vertigo-like sensations. However, anxiety rarely causes the classic brief positional vertigo of BPPV or the days-long continuous vertigo of vestibular neuritis. If your Vertigo Diary documents true spinning with clear triggers and recovery patterns, organic causes (BPPV, neuritis, stroke) are more likely than anxiety alone.
16. Why shouldn’t I automatically assume my “chakkar” is just dizziness or low blood pressure?
Answer: Because “chakkar” is ambiguous, and different causes of vertigo require completely different treatments. Assuming low blood pressure and ignoring specific trigger patterns might delay diagnosis of BPPV (which needs Epley maneuver) or, worse, miss a stroke warning sign. Using your Vertigo Diary to document exact symptoms, triggers, and duration ensures your doctor considers the full differential diagnosis.
17. What role does a hearing test (audiometry) play in diagnosing vertigo?
Answer: Audiometry (hearing test) helps differentiate peripheral from central causes. Sudden sensorineural hearing loss with vertigo suggests inner ear or AICA involvement. Vestibular neuritis should NOT cause hearing loss; if it does, imaging is warranted to rule out stroke or other central pathology. Audiometry is especially important if sudden hearing loss is new.
18. Can children have BPPV, vestibular neuritis, or stroke-related vertigo?
Answer: Yes, though frequencies differ. BPPV is rare in children but can follow head trauma. Vestibular neuritis is common in children 4–14 years and usually has an excellent prognosis. Pediatric posterior circulation strokes are rare but can occur with arterial dissection, cardiac disease, or clotting disorders. The HINTS exam and diagnostic approach are the same in children; red flag symptoms require the same urgent evaluation.
19. If my head impulse test is normal but I have continuous vertigo, what should I do?
Answer: A normal head impulse test with continuous vertigo is a red flag for central (brainstem or cerebellar) pathology, including stroke. Do not accept reassurance based on “normal” findings; specifically request MRI or CT angiography and ask for stroke protocol evaluation. Demand a neurology consultation if not already provided. Early imaging in this scenario is critical.
20. What is the best way to prepare for a vertigo diagnosis appointment?
Answer: (1) Complete a Vertigo Diary documenting all episodes from the past week or month; (2) Note all associated symptoms, especially neurological ones; (3) List all current medications; (4) Document any recent illnesses (colds, flu); (5) Prepare a timeline of symptom onset; (6) Arrive early to allow time for HINTS testing; (7) Ask your doctor specifically about your test results and what they mean for your diagnosis and treatment.
HINGLISH FAQs (20 Questions)
1. BPPV aur Vestibular Neuritis mein main difference kya?
Answer: BPPV = seconds mein chakkar, head movement se trigger, quickly over. Vestibular Neuritis = days/weeks mein continuous, no clear trigger, slowly improve. BPPV = Epley maneuver se cure. Vestibular Neuritis = steroids + rehab. Duration key differentiator hai.
2. Doctor meri eyes check kyun kar raha hai vertigo test mein?
Answer: Eye movements reveal location of problem. HINTS exam mein doctor dekhe: (1) Head impulse—eyes follow smooth? (2) Nystagmus—involuntary jumps? (3) Skew—vertical misalignment? Ye findings distinguish inner ear (peripheral) vs. brainstem (stroke).
3. Epley maneuver kya hai aur kaise kaam karti hai?
Answer: Series of slow head/body positions jo gravity use karti hai crystals ko semicircular canal se bahar nikalne ke liye. 10–15 minutes, 70–90% success rate. Trained healthcare provider ko do karni chahiye.
4. Kya mein ghar pe khud Epley kar sakta hoon?
Answer: Modified versions ghar pe available hain, lekin initially trained specialist ko hi karni chahiye. Dix-Hallpike test se BPPV confirm karti hai, positioning correct karti hai, success verify karti hai. Improper technique ineffective ho sakti hai.
5. Agar mujhe brief positional chakkar hai, toh bilkul BPPV hai na?
Answer: Nahi, zaruri nahi. BPPV most common hai, lekin superior semicircular canal dehiscence, perilymphatic fistula, ya psychiatric dizziness bhi ho sakti hai. Lekin positive Dix-Hallpike + successful Epley response strongly support BPPV.
6. Vestibular Neuritis mein recovery kaisa hota hai?
Answer: (1) Peak in first 24 hours, (2) Improvement 2–4 weeks, most in first 1–2 weeks, (3) Residual imbalance weeks-months. Early movement aur exercises speed-up karti hain. Suppressants avoid karte hain kyunke brain compensation slow ho jaata hai.
7. Vestibular Suppressants kyun discourage karte hain?
Answer: Kyunke symptoms to mask karti hain lekin brain’s compensation ability ko slow kar deti hain. Brain sikhta hai movement se. Early mobilization, uncomfortable hone bhi, faster compensation promote karti hai. Symptoms suppress karte ho toh adaptive process prevent hota hai.
8. Epley ke baad BPPV dobara ho sakti hai?
Answer: Haan. Epley ek episode cure karti hai, lekin crystals dobara dislodge ho sakte hain. Recurrence ~30% within 5 years. Isliye “benign” kehte hain—dangerous nahi, recurrent episodes ko dobara Epley se treat kar sakte ho.
9. Stroke ke chakkar ko alag kisne distinguish karti hai?
Answer: Continuous chakkar + neurological symptoms (double vision, slurred speech, swallowing difficulty, weakness, severe imbalance, facial drooping). Ek bhi symptom + continuous chakkar = emergency evaluation.
10. “Direction-changing nystagmus” matlab kya aur important kyun?
Answer: Eye movements jo gaze based badlti hain—right dekho toh right direction, left dekho toh left direction. Brainstem/cerebellar involvement sign = stroke red flag. Peripheral (inner ear) = same direction regardless of gaze (unidirectional).
11. HINTS exam stroke detect karne mein kitna accurate hai?
Answer: 100% sensitivity + 96% specificity, 48 hours mein. Early MRI 50% false-negative. HINTS 60 seconds, eye movements only, no radiation.
12. Stroke treatment ka critical time window kya hai?
Answer: Thrombolysis (tPA) = 4.5 hours. Mechanical thrombectomy = 24 hours (selective cases). After window, treatment options limited. Fast diagnosis critical.
13. Agar sudden chakkar + sudden hearing loss ek ear mein?
Answer: AICA (Anterior Inferior Cerebellar Artery) infarction suggest karti hai—brain ka internal auditory artery block. Posterior circulation stroke sign = immediate imaging chahiye.
14. Vertigo Diary aur medical consultation mein difference?
Answer: Diary = self-recorded symptom log. Consultation = doctor’s exam + HINTS + tests. Diary objective data provide karti hai, doctor ko faster diagnosis mein help karti hai. Complementary tool, replacement nahi.
15. Anxiety se bhi chakkar aa sakta hai jo peripheral/central mimic kare?
Answer: Haan, lekin anxiety usually nahi cause karti classic BPPV (brief positional) ya vestibular neuritis (days-long continuous). Agar Diary true spinning + clear triggers + recovery pattern show karti hai, toh organic causes (BPPV, neuritis, stroke) likely zyada.
16. Mein kyun automatically assume nahi kar sakta ke mera chakkar sirf “low BP” hai?
Answer: Kyunke “chakkar” vague hai aur different causes ko different treatments chahiye. Low BP assume karte huye BPPV (Epley needs) miss kar sakte ho ya stroke warning miss kar sakte ho. Vertigo Diary exact symptoms, triggers, duration document karti hai.
17. Hearing test (Audiometry) ka vertigo diagnosis mein role kya?
Answer: Sudden sensorineural hearing loss + chakkar = inner ear or AICA involvement. Vestibular Neuritis should NOT cause hearing loss; agar cause karti hai toh imaging for stroke/central pathology. Important agar sudden hearing loss new hai.
18. Bacchon mein bhi BPPV, Vestibular Neuritis, Stroke chakkar aa sakta hai?
Answer: Haan, frequencies different. BPPV rare lekin head trauma baad ho sakti hai. Vestibular Neuritis common ages 4–14, excellent prognosis. Pediatric stroke rare lekin possible (dissection, cardiac, clotting disorder). HINTS exam same approach.
19. Agar mera head impulse test normal hai lekin continuous chakkar hai?
Answer: Normal HIT + continuous chakkar = brainstem/cerebellar problem (stroke) red flag. Don’t accept reassurance. Specifically MRI/CT angiography request karo. Stroke protocol evaluation ask karo. Early imaging critical.
20. Vertigo diagnosis appointment ke liye kaise prepare karo?
Answer: (1) Vertigo Diary complete karo, (2) Associated symptoms note karo, (3) Medications list karo, (4) Recent illness timeline, (5) Symptom onset timeline, (6) Early arrive karo HINTS time lene ke liye, (7) Ask test results aur meaning.
HINDI FAQs (20 Questions)
1. BPPV और Vestibular Neuritis में मुख्य अंतर क्या है?
Answer: BPPV = सेकंड में चक्कर, सिर की गति से ट्रिगर, जल्दी ठीक। Vestibular Neuritis = दिन/हफ्तों में निरंतर, स्पष्ट ट्रिगर नहीं, धीरे-धीरे सुधार। BPPV = Epley मैनुवर से ठीक। Vestibular Neuritis = स्टेरॉयड + पुनर्वास। अवधि मुख्य अंतर है।
2. डॉक्टर मेरी आँखों को चक्कर परीक्षा में क्यों जांचते हैं?
Answer: आँख की गतिविधियां समस्या का स्थान प्रकट करती हैं। HINTS परीक्षा में डॉक्टर देखते हैं: (1) हेड इम्पल्स—आँखें सुचारु रूप से अनुसरण करती हैं? (2) निस्टागमस—अनैच्छिक कूदें? (3) स्केव—ऊर्ध्वाधर गलतसंरेखण? ये निष्कर्ष आंतरिक कान (परिधीय) vs. ब्रेनस्टेम (स्ट्रोक) को अलग करते हैं।
3. Epley मैनुवर क्या है और कैसे काम करता है?
Answer: धीमी सिर/शरीर की गतिविधियों की एक श्रृंखला जो गुरुत्वाकर्षण का उपयोग क्रिस्टल को अर्धवृत्ताकार नलिका से बाहर निकालने के लिए करती है। 10–15 मिनट, 70–90% सफलता दर। प्रशिक्षित स्वास्थ्य सेवा प्रदाता को करना चाहिए।
4. क्या मैं घर पर खुद Epley कर सकता हूँ?
Answer: संशोधित संस्करण घर पर उपलब्ध हैं, लेकिन शुरुआत में प्रशिक्षित विशेषज्ञ को करना चाहिए। Dix-Hallpike परीक्षा BPPV की पुष्टि करती है, स्थिति सही करती है, सफलता सत्यापित करती है। अनुचित तकनीक अप्रभावी हो सकती है।
5. अगर मुझे संक्षिप्त स्थितिजन्य चक्कर है, तो क्या यह निश्चित रूप से BPPV है?
Answer: नहीं, जरूरी नहीं। BPPV सबसे आम है, लेकिन superior semicircular canal dehiscence, perilymphatic fistula, या psychiatric dizziness भी हो सकती है। लेकिन सकारात्मक Dix-Hallpike + सफल Epley प्रतिक्रिया BPPV को दृढ़ता से समर्थन करती है।
6. Vestibular Neuritis में रिकवरी कैसी होती है?
Answer: (1) पहले 24 घंटों में चोटी, (2) 2–4 हफ्तों में सुधार, अधिकांश पहले 1–2 हफ्तों में, (3) अवशिष्ट असंतुलन हफ्तों-महीनों। शुरुआती आंदोलन और व्यायाम तेजी लाते हैं। Suppressants से बचें क्योंकि मस्तिष्क की क्षतिपूर्ति धीमी हो जाती है।
7. Vestibular Suppressants को हतोत्साहित क्यों किया जाता है?
Answer: क्योंकि वे लक्षणों को दबाते हैं लेकिन मस्तिष्क की क्षतिपूर्ति क्षमता को धीमा कर देते हैं। मस्तिष्क आंदोलन से सीखता है। शुरुआती गतिविधि, असहज होने के बावजूद, तेजी से क्षतिपूर्ति को बढ़ावा देती है। लक्षणों को दबाने से अनुकूल प्रक्रिया रुक जाती है।
8. Epley के बाद BPPV फिर से हो सकती है?
Answer: हाँ। Epley एक एपिसोड को ठीक करता है, लेकिन क्रिस्टल फिर से विस्थापित हो सकती हैं। पुनरावृत्ति ~ 5 साल में 30%। इसीलिए “सौम्य” कहते हैं—खतरनाक नहीं, पुनरावर्ती एपिसोड को फिर से Epley से ठीक कर सकते हैं।
9. स्ट्रोक के चक्कर को अलग कौन सी बात करती है?
Answer: निरंतर चक्कर + न्यूरोलॉजिकल लक्षण (दोहरी दृष्टि, अस्पष्ट बोली, निगलने की कठिनाई, कमजोरी, गंभीर असंतुलन, चेहरा झुकना)। एक भी लक्षण + निरंतर चक्कर = आपातकालीन मूल्यांकन।
10. “दिशा-परिवर्तन निस्टागमस” का मतलब क्या है और यह महत्वपूर्ण क्यों है?
Answer: आँख की गतिविधियां जो गेज़ के आधार पर बदलती हैं—दाएं देखो तो दाएं दिशा, बाएं देखो तो बाएं दिशा। ब्रेनस्टेम/सेरिबेलर involvement = स्ट्रोक लाल झंडा। परिधीय (आंतरिक कान) = दृष्टि की परवाह किए बिना समान दिशा (एकदिशीय)।
11. HINTS परीक्षा स्ट्रोक का पता लगाने में कितनी सटीक है?
Answer: 100% संवेदनशीलता + 96% विशिष्टता, 48 घंटों में। शुरुआती MRI 50% झूठी नकारात्मक। HINTS 60 सेकंड, आँख की गतिविधियां केवल, कोई विकिरण नहीं।
12. स्ट्रोक उपचार की महत्वपूर्ण समय सीमा क्या है?
Answer: Thrombolysis (tPA) = 4.5 घंटे। यांत्रिक thrombectomy = 24 घंटे (चयनात्मक मामले)। विंडो के बाद, उपचार विकल्प सीमित। तीव्र निदान महत्वपूर्ण।
13. अगर अचानक चक्कर + अचानक एक कान में श्रवण हानि?
Answer: AICA (Anterior Inferior Cerebellar Artery) इनफार्क्शन सुझाता है—मस्तिष्क की आंतरिक श्रवण धमनी block। पोस्टीरियर परिसंचरण स्ट्रोक संकेत = तुरंत इमेजिंग चाहिए।
14. Vertigo Diary और medical consultation में अंतर?
Answer: डायरी = self-recorded symptom log। परामर्श = डॉक्टर की परीक्षा + HINTS + परीक्षण। डायरी objective data प्रदान करती है, डॉक्टर को तेजी से निदान में मदद करती है। पूरक उपकरण, प्रतिस्थापन नहीं।
15. क्या चिंता से चक्कर आ सकता है जो परिधीय/केंद्रीय नकल करे?
Answer: हाँ, लेकिन चिंता आमतौर पर BPPV का क्लासिक संक्षिप्त स्थितिजन्य या vestibular neuritis का दिन-लंबा निरंतर कारण नहीं बनती। अगर Diary true spinning + स्पष्ट ट्रिगर + recovery पैटर्न दिखाती है, तो organic कारण (BPPV, neuritis, stroke) अधिक संभावित हैं।
16. मैं स्वचालित रूप से यह क्यों मान नहीं सकता कि मेरा चक्कर सिर्फ “कम BP” है?
Answer: क्योंकि “चक्कर” अस्पष्ट है और अलग-अलग कारणों को अलग-अलग उपचार चाहिए। कम BP मान लेते हुए BPPV (Epley की आवश्यकता) को मिस कर सकते हैं या स्ट्रोक चेतावनी को मिस कर सकते हैं। Vertigo Diary सटीक लक्षण, ट्रिगर, अवधि document करती है।
17. सुनने की परीक्षा (Audiometry) का चक्कर निदान में क्या भूमिका है?
Answer: अचानक sensorineural श्रवण हानि + चक्कर = आंतरिक कान या AICA involvement। Vestibular Neuritis को श्रवण हानि नहीं देनी चाहिए; अगर देती है तो stroke/central pathology के लिए इमेजिंग। महत्वपूर्ण अगर अचानक श्रवण हानि नई है।
18. क्या बच्चों में BPPV, Vestibular Neuritis, Stroke चक्कर आ सकता है?
Answer: हाँ, आवृत्तियां अलग-अलग। BPPV दुर्लभ लेकिन सिर की चोट के बाद हो सकती है। Vestibular Neuritis ages 4–14 में सामान्य, उत्कृष्ट पूर्वानुमान। बाल रोग स्ट्रोक दुर्लभ लेकिन संभव (dissection, cardiac, clotting disorder)। HINTS परीक्षा समान दृष्टिकोण।
19. अगर मेरी हेड इम्पल्स परीक्षा सामान्य है लेकिन निरंतर चक्कर है?
Answer: सामान्य HIT + निरंतर चक्कर = ब्रेनस्टेम/सेरिबेलर समस्या (स्ट्रोक) लाल झंडा। reassurance को स्वीकार न करें। विशेष रूप से MRI/CT angiography अनुरोध करें। Stroke protocol मूल्यांकन मांगें। शुरुआती इमेजिंग महत्वपूर्ण।
20. Vertigo निदान appointment के लिए कैसे तैयार करें?
Answer: (1) Vertigo Diary पूरी करें, (2) संबंधित लक्षण नोट करें, (3) दवाएं सूचीबद्ध करें, (4) हाल की बीमारी timeline, (5) लक्षण शुरुआत timeline, (6) जल्दी आएं HINTS समय के लिए, (7) परीक्षा परिणाम और अर्थ पूछें।