The vertigo medication trap dizziness pills trap is real: most dizziness pills delay your recovery, not accelerate it. This comprehensive guide explains why vestibular suppressant medications (antihistamines, benzodiazepines, anticholinergics) create a cycle of dependency and how to escape it safely.
🎯 TL;DR (Too Long; Didn’t Read)
- Main trap: Vestibular suppressants (antihistamines, benzodiazepines, anticholinergics) provide SHORT-TERM relief but PREVENT the brain’s natural healing process (central compensation)
- 72-hour rule: Suppressants appropriate ONLY for first 24–72 hours of acute vertigo attack; beyond that, they delay recovery by months
- BPPV reality: Physical repositioning maneuvers (Epley, Semont) cure 80–90% of cases; NO medication can move ear crystals back to normal position
- Rebound dizziness: Abrupt medication withdrawal causes temporary severe dizziness, BUT this is a sign the brain is waking up—not disease recurrence
- Safe exit: Gradual medication taper + early mobilization + vestibular rehabilitation therapy (VRT) = true recovery (60–80% improvement)
- Elderly risk: Suppressants dramatically increase fall risk, cognitive slowing, and drug-induced Parkinsonism in adults 65+
- Action plan: If on dizziness pills >72 hours without diagnosis, ask for vestibular evaluation (Dix-Hallpike, HINTS) and supervised medication taper
Table of Contents
ENGLISH VERSION
The Vertigo Medication Trap: Why These Pills Are Making You Dizzy (Not Better)
Introduction: The Well-Intentioned Trap
Vertigo and dizziness are among the most common reasons patients seek medical advice, accounting for up to 30% of consultations in neurology and ear, nose, and throat (ENT) clinics. The sensation of a spinning world is terrifying, and the immediate instinct to reach for a pill is completely understandable. Yet this instinct leads countless patients into a medication trap where the treatment intended to help actually prevents the brain from healing.
A typical patient journey: A patient experiences an acute vertigo attack. Their doctor prescribes meclizine (Antivert), diazepam (Valium), or scopolamine. The patient feels better immediately—the spinning subsides, nausea diminishes, and they can function again. Gratefully, they continue the medication. Weeks pass. They expect full recovery, but instead find themselves still dizzy, still dependent on pills, with no clear path forward.
This is the medication trap. And it affects millions of patients globally.
The Paradox of Dizziness Medication
To understand why this trap exists, one must understand a fundamental principle: vertigo medications do not treat the underlying cause. They suppress the symptom.
Patients suffering from vertigo experience an array of sensations—violent rotation, floating, lightheadedness, or unsteadiness. In clinical settings, these varied symptoms are often treated with a broad category of drugs known as vestibular suppressants. While these medications can provide temporary relief from the intense nausea and spinning of an acute attack, they do not address the underlying dysfunction. Instead, they work by “quieting” the brain’s balance centers, which is exactly the opposite of what the brain needs to recover long-term.
This is the paradox: Suppressants feel good in the moment but prevent recovery over time.
Who Are the Culprits? Understanding the Classes of Suppressants
The medications most commonly implicated in the vertigo trap fall into three main pharmacological classes. Understanding each class is essential for informed decision-making about medication use.
1. Antihistamines: Common, Sedating, Ineffective Long-Term
Medications in this class:
- Meclizine (Antivert) – Most commonly prescribed for vertigo
- Cyclizine – Slightly less sedating than meclizine
- Dimenhydrinate (Dramamine) – Available over-the-counter
Mechanism:
- Block H1 (histamine) receptors in the vestibular nuclei of the brainstem
- Reduce the vestibular system’s responsiveness to motion and balance signals
- Also have anticholinergic properties (dry mouth, urinary retention)
Short-term benefit:
- Reduce motion sensitivity and nausea within 30 minutes
- Allow rest during an acute attack
Long-term problems:
- Sedation: Patients report brain fog, fatigue, difficulty concentrating
- Dry mouth, blurred vision, constipation: Common side effects
- Cognitive effects: Especially problematic in elderly patients
- Prolongs recovery: Clinical studies show meclizine extends the duration of illness by delaying central compensation
- Tolerance: Over weeks, the brain adapts; higher doses become necessary for same effect
- Rebound symptoms: Withdrawal causes temporary worsening of dizziness
Clinical reality: Antihistamines are appropriate for maybe 24–48 hours during a severe acute attack. Beyond that, they become obstacles to recovery.
2. Benzodiazepines: Powerful, Addictive, Dangerous Long-Term
Medications in this class:
- Diazepam (Valium) – Long-acting; used for acute and chronic vertigo
- Lorazepam (Ativan) – Medium-acting; preferred in hospitals
- Alprazolam (Xanax) – Short-acting; sometimes prescribed
Mechanism:
- Enhance gamma-aminobutyric acid (GABA), the primary inhibitory neurotransmitter in the central nervous system
- Suppress activity throughout the vestibular system and brainstem
- Produce profound sedation and muscle relaxation
Short-term benefit:
- Highly effective at suppressing severe vertigo (especially useful during violent Menière’s attacks)
- Reduce anxiety associated with dizziness
- Allow sleep during acute episodes
Long-term problems—CRITICAL:
- Addiction risk: Benzodiazepines are highly addictive; tolerance develops within days
- Cognitive impairment: Persistent memory problems, confusion, difficulty processing information
- Fall risk: Dramatically increases in elderly patients; a leading cause of fractures and death in age 65+
- Dependency: Even patients who follow dosing instructions can become dependent within weeks
- Withdrawal is dangerous: Abrupt discontinuation can cause seizures; tapering must be slow (weeks to months)
- Paradoxical effects: Some patients experience anxiety and dizziness with continued use
- Interaction with other drugs: Particularly dangerous combined with alcohol or opioids
- Delays recovery: Like antihistamines, benzodiazepines suppress the vestibular signals the brain needs to compensate
Clinical reality: Benzodiazepines are appropriate for perhaps 24–72 hours during a severe, acute attack. Long-term use (more than 1–2 weeks) is unjustifiable for vertigo and carries serious risks.
3. Anticholinergics: Effective for Motion Sickness, Dangerous for Elderly
Medications in this class:
- Scopolamine (transdermal patch) – Most effective for motion sickness; used for some vertigo
- Atropine – Systemic anticholinergic; rarely used for vertigo
Mechanism:
- Block muscarinic acetylcholine receptors
- Reduce signal transmission in the vestibular nuclei
- Highly effective at suppressing motion-induced nausea and spinning
Short-term benefit:
- One of the most effective drugs for preventing motion sickness
- Scopolamine patch provides continuous delivery for days
- Can be useful during acute Menière’s attacks
Long-term problems—SEVERE in elderly:
- Anticholinergic toxicity: Causes confusion, delirium, agitation, hallucinations
- Urinary retention: Particularly dangerous; can lead to urinary tract infections and acute kidney injury
- Dry mouth and blurred vision: Reduces tear production (risk of corneal damage)
- Cognitive decline: Anticholinergics are associated with increased dementia risk in elderly patients
- Constipation: Can be severe; may require hospitalization
- Increased heart rate and eye pressure: Problematic in patients with glaucoma or cardiac disease
- “Anticholinergic burden”: Cumulative risk when combined with other anticholinergic drugs
Clinical reality: Scopolamine patches are sometimes appropriate for motion sickness prevention during travel, but should NOT be used as chronic vertigo management. In elderly patients, anticholinergics are particularly dangerous.
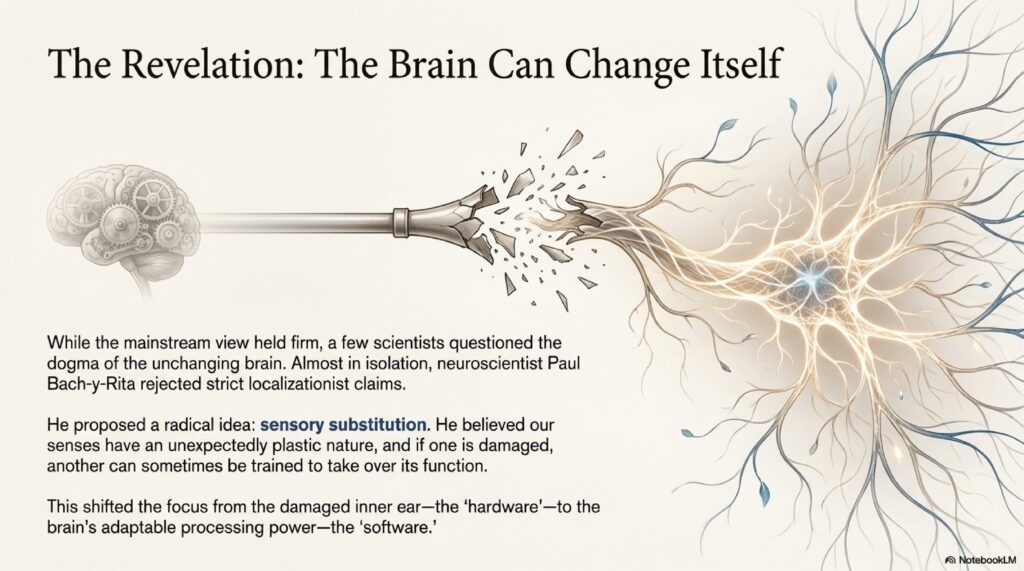
The “Central Compensation” Process: How the Brain Heals
To understand why these medications are problematic, one must understand how the brain naturally repairs a damaged balance system. This process is called central compensation, and it is the key to true, long-term recovery.
What Is Central Compensation?
When an inner ear is injured—such as during vestibular neuritis, post-traumatic BPPV, or a Menière’s attack—the brain receives asymmetric and confusing signals from the balance organs. One ear may be sending normal signals while the other sends weak or absent signals. This imbalance is what creates the sensation of spinning.
Fortunately, the central nervous system has a remarkable ability to recalibrate itself. The brain essentially “learns” to ignore the missing or incorrect signals from the damaged ear and relies more heavily on:
- Vision: The eyes help confirm that the world is actually still
- Proprioception: The feeling of the floor beneath the feet, body position in space
- Vestibular input from the healthy ear: The normal side takes over
- Cerebellar adaptation: The cerebellum rewires neural pathways to compensate for asymmetry
The Recovery Timeline with Central Compensation
Natural recovery from vestibular neuritis (without suppressants):
- Days 1–3: Severe vertigo, nausea (body’s natural inflammatory response)
- Days 4–7: Gradual improvement as central compensation begins
- Weeks 2–4: Noticeable improvement with daily activity; exercises accelerate recovery
- Weeks 4–8: 80–90% resolution of dizziness; residual imbalance improving with VRT
- Months 2–3: Full functional recovery in most cases
With continuous suppressants (blocking central compensation):
- Days 1–3: Symptomatic relief
- Weeks 2–8: Continued dizziness (compensation blocked)
- Months 2–12: Chronic dizziness, medication dependency, little improvement
- Years: Some patients remain dizzy indefinitely, trapped in medication use
The Key: Sensory Mismatch
Central compensation requires a crucial element: the brain must experience the dizziness in order to learn how to fix it. This is called “sensory mismatch”—the brain detects an inconsistency between what the damaged vestibular system is reporting and what vision and proprioception are reporting. This mismatch is the signal that triggers adaptation.
When suppressants remove this signal, the brain has nothing to adapt to. The brain cannot learn. Compensation cannot begin. Recovery is stalled.
How Suppressants Jam the Repair Shop
The fundamental problem with vestibular suppressants is beautifully captured in this analogy: Imagine your car’s check engine light is on. Instead of fixing the engine, you simply tape over the warning light. The light is gone, but the engine is still broken—and now it’s getting worse.
Vestibular suppressants work similarly. They silence the signals the brain is receiving about imbalance, but they do not fix the underlying vestibular dysfunction.
Clinical Evidence
Multiple clinical trials and meta-analyses have conclusively demonstrated:
- Short-term efficacy: Vestibular suppressants reduce symptoms in the first 24–48 hours
- Long-term inefficacy: Continued use beyond 72 hours does NOT improve total recovery time; it actually prolongs it
- Compensation delay: Patients on prolonged suppressants show delayed or absent central compensation on vestibular testing
- Extended illness: Patients on suppressants for weeks or months remain symptomatic longer than those who receive early VRT without medication
The Cycle of the Trap
This is how patients become trapped:
- Acute attack: Patient experiences severe vertigo
- Medication prescribed: Doctor prescribes suppressant; patient feels better
- Patient continues medication: Assuming medication is helping recovery
- Compensation blocked: Suppressant prevents the brain’s natural healing
- Dizziness persists: Because compensation hasn’t occurred
- Patient interprets persistence as need for more medication: “I’m still dizzy, so I need to keep taking this”
- Months pass: Patient remains on medication, still dizzy
- Medication dependency develops: Patient feels worse when trying to stop
- Chronic dizziness: Patient may remain symptomatic for months or years
The Elderly Factor: A Heightened Risk
The risks of long-term suppressant use are exponentially higher in patients over the age of 65. This is where the medication trap becomes a genuine public health crisis.
Why Elderly Patients Are Vulnerable
Natural age-related decline:
- Vestibular function naturally declines with age (vestibular hair cell loss, reduced proprioception)
- Vision may be compromised (cataracts, age-related macular degeneration)
- Proprioceptive function is reduced (neuropathy, reduced joint proprioceptors)
The medication on top of decline:
- Adding sedating suppressants to this already-compromised system creates a “perfect storm”
- The brain has fewer compensatory mechanisms available; suppressants block the few it has
- Result: Severe, persistent imbalance and dizziness
Falls: The Critical Risk
Falls in elderly patients are a leading cause of injury and death.
- One-third of adults age 65+ fall each year
- Falls are the leading cause of both unintentional injury death and nonfatal trauma
- Fall-related hip fractures often lead to loss of independence and premature death
Suppressants dramatically increase fall risk:
- Sedation and cognitive impairment affect balance and reaction time
- Anticholinergics cause blurred vision (further impairing proprioception)
- Benzodiazepines increase fall risk by 50–80% in elderly patients
Example: A 78-year-old patient with mild vestibular neuritis is prescribed meclizine. While on meclizine, the patient experiences brain fog and dizziness. During an attempt to get up at night, the patient falls, fractures a hip, and loses independence. The medication intended to prevent dizziness actually caused a catastrophic injury.
Drug-Induced Parkinsonism
Antihistamines and anticholinergics can cause “extrapyramidal symptoms” that mimic Parkinson’s disease:
- Tremors
- Muscle rigidity (stiffness)
- Bradykinesia (slow movement)
- Shuffling gait
- Postural instability
Many elderly patients are misdiagnosed with “age-related decline,” “vascular dementia,” or “Parkinson’s disease” when their symptoms are actually drug-induced and reversible.
Withdrawal and Rebound: Why Stopping Is Hard
Once a patient has been on vestibular suppressants for more than a few days, the body begins to adapt to the drug’s presence. If the medication is stopped abruptly, the patient may experience a “rebound” effect.
Rebound Vertigo: The Misunderstanding
What happens: When a suppressant is suddenly discontinued, the brain—which has been artificially quieted—suddenly “wakes up.” The suppressed vestibular signals return in force. The patient experiences:
- Acute vertigo (often worse than the original attack)
- Nausea and vomiting
- Anxiety
- Panic (patient thinks the disease is returning)
What this means: This is NOT a sign that the disease is active. This is a sign that the brain is waking up. It is a GOOD sign. The rebound effect is temporary—usually lasting 24–72 hours—and indicates that the medication is clearing.
The Trap Deepens
Unfortunately, many patients interpret rebound as disease recurrence:
- Patient feels worse after stopping medication
- Patient becomes frightened
- Patient returns to the medication to make the rebound stop
- The trap deepens; the patient feels more dependent on the medication
- Years of medication use may follow a single incident of rebound dizziness
Benzodiazepine Withdrawal: More Serious
For patients on benzodiazepines, withdrawal is more complex and potentially dangerous:
Benzodiazepine withdrawal syndrome includes:
- Severe anxiety and panic
- Tremors
- Seizures (in severe cases)
- Psychological dependence (feeling unable to function without the drug)
Benzodiazepines must be tapered slowly (over weeks to months), not discontinued abruptly. The tapering process itself is often uncomfortable and requires medical supervision.
Conditions Where Pills Often Fail Entirely
It is crucial to recognize that for many common causes of dizziness, vestibular suppressants are not effective even in the short term. In these cases, medications are not just unhelpful—they actively delay diagnosis and proper treatment.
1. BPPV: Mechanical Problem, Not Chemical
Benign Paroxysmal Positional Vertigo is the most common cause of recurrent vertigo (20–40% of all vertigo). Yet suppressants are completely ineffective for BPPV.
Why: BPPV is a mechanical problem. Tiny calcium carbonate crystals have migrated into the wrong part of the inner ear (semicircular canal). When the head moves, these crystals shift, triggering false rotation signals.
Why pills don’t work: No pill can move crystals back to their correct location. The crystals are physical objects; they require physical repositioning.
What actually works:
- Dix-Hallpike maneuver (diagnostic test)
- Epley maneuver or Semont maneuver (physical repositioning)
- Cure rate: 80–90% with a single maneuver
The trap: A patient with BPPV is prescribed meclizine. The meclizine reduces nausea slightly but does NOT cure BPPV. The patient takes meclizine for weeks, still experiencing positional vertigo. If the patient had received an Epley maneuver on Day 1, they would have been cured in 5 minutes.
2. PPPD: Pills Make It Worse
Persistent Postural-Perceptual Dizziness (PPPD), also called functional or psychogenic dizziness, is increasingly recognized as a common cause of chronic vertigo.
What is PPPD:
- The brain’s balance system is functioning normally
- But the brain’s “balance filter” is stuck in a heightened state of alert
- The patient perceives minor movements and sensory fluctuations as dizziness
- Usually follows a vestibular trigger (BPPV, neuritis, migraine) but persists after that trigger has resolved
Why suppressants fail:
- Suppressants cannot reset a “stuck” balance filter
- The sedation and cognitive effects of suppressants actually worsen brain fog and fatigue (which are core PPPD symptoms)
- PPPD responds much better to cognitive-behavioral therapy (CBT), exposure therapy, and VRT
The trap: A patient with PPPD is prescribed benzodiazepines. The patient experiences brain fog and fatigue from the medication. The patient’s PPPD symptoms worsen because they are now more sedentary and anxious (from medication side effects). The patient mistakenly thinks they need higher doses.
3. Vestibular Migraine: Medication for Prevention, Not Suppression
Vestibular migraine is a common cause of recurrent vertigo, often with associated headache. While some medications can help prevent migraine attacks, suppressants do not address the underlying mechanism.
What works for vestibular migraine:
- Preventative medications: Propranolol, topiramate, amitriptyline, CGRP monoclonal antibodies
- VRT
- Migraine trigger avoidance
- Lifestyle optimization
When Are Vertigo Pills Appropriate? The 72-Hour Rule
There is a narrow window where suppressants are medically appropriate. The 72-Hour Rule is a useful framework:
The 72-Hour Rule
First 24 hours of acute severe vertigo attack:
- Suppressants are appropriate and often necessary
- Goal: Stop active vomiting, allow rest, prevent dehydration
- Appropriate medications: Antihistamines (meclizine) or short-term benzodiazepines (lorazepam)
- Expected outcome: Symptomatic relief
24–72 hours:
- Suppressants may still be needed if symptoms are severe
- Transition phase: Begin gentle mobilization and exercises even while on medication
- Plan for medication taper should begin
Beyond 72 hours:
- Suppressants should be tapered and discontinued
- Goal shifts to promoting central compensation
- VRT should begin
- Gentle activity is encouraged
- Medication withdrawal symptoms are expected and normal
Conditions That Require Longer Medication Use
Very rare exceptions where suppressants may be needed beyond 72 hours:
- Severe Menière’s attack with persistent vomiting: If the patient cannot keep fluids down, medication may be needed longer (but 1–2 weeks maximum)
- Hospitalized acute vestibular neuritis: If severe enough to require hospitalization, medication may be used for several days during acute phase
- Severe migraine-associated vertigo: If migraine is severe and uncontrolled, migraine-specific medications (not suppressants) are indicated
What NOT to do:
- ❌ Do not remain on suppressants for weeks without a specific diagnosis
- ❌ Do not remain on suppressants without concurrent VRT
- ❌ Do not dismiss medication side effects as acceptable trade-offs
- ❌ Do not assume suppressants are causing recovery
The Exit Strategy: How to Reclaim Your Balance
If you find yourself stuck in the vertigo medication trap—taking pills for weeks or months with little improvement—recovery is still possible. The path forward involves three essential pillars.
Pillar 1: Tapering Under Supervision
Never stop suppressants abruptly. Work with a physician to gradually reduce suppressed medications. This prevents severe withdrawal and rebound symptoms.
Antihistamine taper (meclizine, cyclizine):
- These have less severe withdrawal than benzodiazepines
- Can typically be reduced every 3–5 days
- Taper over 1–2 weeks
- Expect mild rebound dizziness for 24–72 hours after stopping
Benzodiazepine taper (diazepam, lorazepam):
- MUST be tapered slowly to avoid seizures and severe withdrawal
- Typical taper: Reduce dose by 10% per week
- May take 2–3 months or longer
- Requires close medical supervision
- Expect anxiety, tremors, and rebound dizziness during taper
- These symptoms will resolve as the taper completes
Anticholinergic taper (scopolamine):
- Transdermal patches can be reduced by using smaller patch or removing for shorter periods
- Taper over 1–2 weeks
- Expect cognitive sharpening as medication clears
Pillar 2: Early Mobilization
The brain needs movement to heal. Even if it makes you feel slightly dizzy, gentle activity and keeping the head moving are the strongest triggers for central compensation.
What to do:
- Walking: Even 10–15 minutes of gentle walking 2–3 times per day
- Head movements: Gentle rotations left and right, flexion and extension
- Visual tracking: Follow a moving object with your eyes while keeping your head still
- Balance challenges: Standing on one leg (if safe), walking heel-to-toe on a line
- Gradual progression: As tolerance improves, increase intensity and duration
Why this works:
- Each time the brain experiences dizziness and nothing bad happens, it recalibrates
- Movement provides the “sensory mismatch” the brain needs to adapt
- Studies show early mobilization shortens recovery by 50% compared to bed rest
What NOT to do:
- ❌ Remain sedentary in a dark room
- ❌ Wear a neck collar or other immobilizing device
- ❌ Avoid all activity out of fear
- ❌ Use suppressants as an excuse to avoid movement
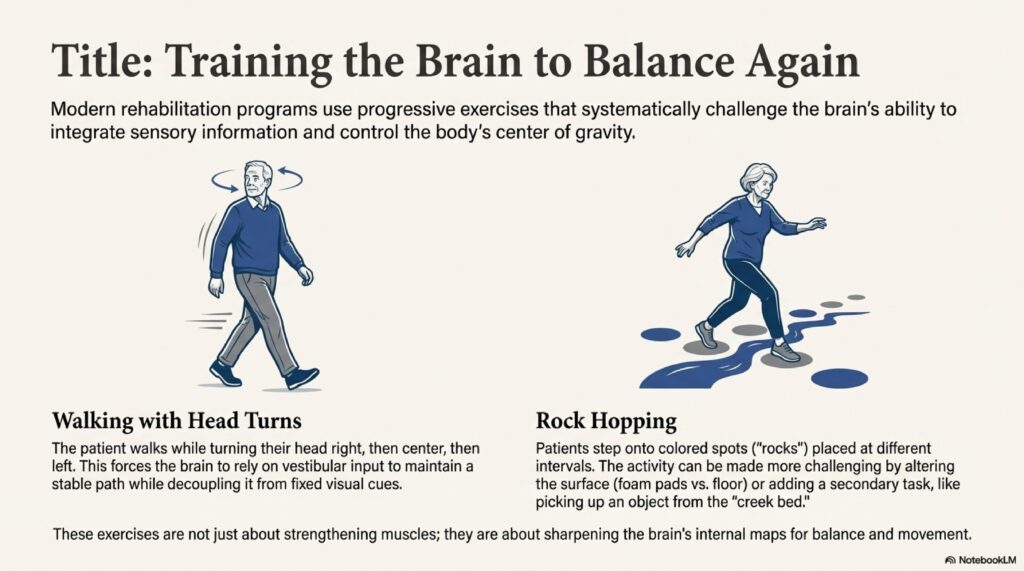
Pillar 3: Vestibular Rehabilitation Therapy (VRT)
VRT is a specialized exercise program designed to speed up the brain’s ability to adapt. These exercises involve specific head and eye movements that retrain the balance system.
What VRT includes:
- Gaze stabilization exercises: Improve eye fixation during head movement (e.g., VOR exercises)
- Balance training: Standing on unstable surfaces, tandem stance, single-leg stance
- Habituation exercises: Gradual exposure to motion-provocative stimuli
- Proprioceptive training: Improving awareness of body position in space
- Functional training: Practice with activities that provoke dizziness (driving, crowds, escalators)
Efficacy:
- Effective in 60–80% of patients with peripheral vestibular dysfunction
- Best results when started early (within first 2 weeks)
- Often combined with early mobilization
Typical progression:
- Weeks 1–2: Basic gaze stabilization and balance exercises at home
- Weeks 2–4: Progression to more challenging exercises, introduction to vestibular PT if available
- Weeks 4–8: Advanced functional training, return to normal activities
- Weeks 8–12: Fine-tuning, prevention of recurrence
Medication Safety Table: Comparing Common Vertigo Suppressants
| Medication Class | Drug Name | Mechanism | Short-Term Efficacy | Onset | Duration | Common Side Effects | Risk of Dependency | Appropriate Duration | When to STOP |
|---|---|---|---|---|---|---|---|---|---|
| Antihistamine | Meclizine (Antivert) | H1 receptor blockade | Moderate (30–60% nausea reduction) | 30–60 min | 4–6 hours | Sedation, dry mouth, blurred vision, constipation | Low | 24–72 hours | Day 3–4; taper over 1–2 weeks |
| Antihistamine | Dimenhydrinate (Dramamine) | H1 receptor blockade + anticholinergic | Moderate | 20–40 min | 4–6 hours | Sedation (stronger than meclizine), dry mouth, urinary retention | Low | 24–48 hours | Day 2–3; taper over 3–5 days |
| Antihistamine | Cyclizine | H1 receptor blockade (less anticholinergic) | Moderate | 30 min | 4–6 hours | Sedation (milder), dry mouth | Low | 24–72 hours | Day 3–4; taper over 1–2 weeks |
| Benzodiazepine | Diazepam (Valium) | GABA enhancement (long-acting) | High (excellent nausea suppression) | 15–30 min | 6–12 hours (long-acting) | Sedation, cognitive impairment, ataxia, dependence | VERY HIGH | 24–72 hours MAX | Day 3–4; slow taper over weeks |
| Benzodiazepine | Lorazepam (Ativan) | GABA enhancement (medium-acting) | High (excellent nausea suppression) | 10–20 min | 4–6 hours | Sedation, cognitive impairment, ataxia, dependence | VERY HIGH | 24–72 hours MAX | Day 3–4; slow taper over weeks |
| Benzodiazepine | Alprazolam (Xanax) | GABA enhancement (short-acting) | Moderate–High | 15–30 min | 4–6 hours | Anxiety rebound, sedation, dependence | VERY HIGH | Not recommended for vertigo | Avoid entirely; taper if prescribed |
| Anticholinergic | Scopolamine (Transdermal Patch) | Muscarinic receptor blockade | Very High (motion sickness) | 4–8 hours (slow absorption) | 72 hours per patch | Confusion, delirium, urinary retention, dry mouth, blurred vision | Moderate | 24–72 hours (travel only) | After travel; taper over 1–2 weeks |
| Anticholinergic | Atropine (IV/IM) | Muscarinic receptor blockade | High (systemic) | Minutes | 2–4 hours | Severe anticholinergic toxicity, confusion, hallucinations | Moderate | Rarely used for vertigo | Discontinue after acute phase |
Safe Medication Taper Protocol: Step-by-Step
If You’ve Been on Suppressants for Less Than 1 Week
Most likely scenario: You took meclizine or a benzodiazepine for the first few days of an acute attack.
Taper plan:
- Days 1–3: Continue current dose (if helping nausea)
- Day 4: Reduce dose by 50% (e.g., meclizine from 25 mg 3× daily to 25 mg 1–2× daily)
- Day 6: Reduce to 25 mg as-needed only (not scheduled)
- Day 8: Stop completely (if manageable; if not, continue 1–2 more days)
- After stopping: Expect mild rebound dizziness for 24–72 hours; this is NORMAL and indicates medication clearing
- Simultaneously: Begin gentle mobilization and exercises even while on medication
If You’ve Been on Suppressants for 1–4 Weeks
Likely scenario: You were prescribed medication after an acute attack but haven’t started VRT yet.
Taper plan:
- Week 1: Continue current dose; simultaneously begin gentle head movements and light walking (even if on medication)
- Week 2: Reduce dose by 25% (e.g., meclizine from 25 mg 3× daily to 25 mg 2× daily)
- Week 3: Reduce to 25 mg 1× daily (morning) or as-needed
- Week 4: Stop completely
- After stopping: Expect rebound dizziness for 24–72 hours; increase mobilization and exercise intensity
- Weeks 5–12: Engage in structured VRT with physical therapist if possible
For benzodiazepines:
- Reduce by 10–25% per week (slower taper required)
- Expect withdrawal symptoms (anxiety, tremors); these are temporary
- May take 3–8 weeks to taper completely
- Medical supervision strongly recommended
If You’ve Been on Suppressants for More Than 4 Weeks
Alert situation: You may be trapped in the medication cycle.
What to do immediately:
- Schedule a vestibular evaluation with an ENT or neurologist
- Ask for: Dix-Hallpike test (if positional vertigo), HINTS exam (if constant vertigo)
- Request VRT referral from a physical therapist specializing in vestibular disorders
- Discuss medication taper with your doctor; provide this protocol
- Don’t stop medication abruptly; taper under supervision
Taper plan for long-term use:
- Months 1–2: Reduce dose by 10–25% per week (benzodiazepines very slowly: 10% per week)
- Months 2–3: Continue gradual reduction
- Simultaneously: Intensive VRT 2–3 times per week
- Support: Counseling or cognitive-behavioral therapy helpful for anxiety during taper
- Medical supervision: Essential for safe, successful taper
Conclusion: Breaking Free from the Medication Trap
Vertigo medication is a double-edged sword. While suppressants provide necessary relief during the most violent phases of an attack, their long-term use is one of the most common barriers to full recovery. If you have been taking “dizziness pills” for weeks or months and still do not feel steady, you may be stuck in the trap.
Real recovery comes not from suppressing the system, but from challenging it to find its balance again.
The three pillars—supervised medication taper, early mobilization, and vestibular rehabilitation—form the evidence-based pathway to true recovery. Recovery is possible. The trap can be escaped. And the brain, given the chance to heal without chemical suppression, is far more capable of adaptation than most patients realize.
HINGLISH VERSION
Vertigo Medication Trap: Kaise Ye Pills Aapko Dizzy Bana Rahe Hain (Sahi Nahi Ho)
Introduction: Well-Intentioned Trap
Vertigo = most common reason लोग doctor देखते हैं (neurology, ENT में 30% consultations)। Spinning world = terrifying। Instinct = immediately pill लेना। Lekin exactly यह instinct millions को medication trap में डालती है।
Typical journey: Acute vertigo attack → Doctor prescribes meclizine/Valium/scopolamine → Better लगता है → Weeks pass → Still dizzy → Still medication पर dependent!
यही है medication trap।
The Paradox of Dizziness Medication
Key truth: Vertigo medications treat symptom, NOT underlying cause।
Patients = varied sensations (violent rotation, floating, lightheaded)। Clinical settings में = “vestibular suppressants” prescribe किया जाता है। Short-term = relief (nausea reduce)। Long-term = recovery block होता है।
Paradox: Medicine feel good now, but prevent recovery later।
Who Are the Culprits? Understanding the Classes of Suppressants
1. Antihistamines: Common, Sedating, Bad Long-Term
Drugs:
- Meclizine (Antivert) – Most common
- Cyclizine, Dimenhydrinate (Dramamine) – OTC available
How:
- H1 receptors block करते हैं vestibular nuclei में
- Motion sensitivity reduce
Benefits:
- Nausea कम, 30 min में effect
Problems:
- Sedation, brain fog, dry mouth, blurred vision
- Recovery delay करते हैं
- Tolerance develop होता है (higher dose needed)
- Rebound symptoms (stopping = worse dizziness)
Reality: 24–48 hours appropriate; उससे ज्यादा = recovery obstacle।
2. Benzodiazepines: Powerful, Addictive, DANGEROUS
Drugs:
- Diazepam (Valium), Lorazepam (Ativan), Alprazolam (Xanax)
How:
- GABA enhance करते हैं (inhibitory neurotransmitter)
- Severe vestibular suppression
Benefits:
- Very effective short-term (violent Menière’s में)
- Sleep help
Problems—CRITICAL:
- Addiction: Tolerance days में develop होता है
- Cognitive impairment: Memory, confusion
- Falls: Elderly में especially—fractures, deaths
- Dependency: Weeks में हो सकता है
- Dangerous withdrawal: Abrupt stop = seizures
- Slow taper needed: Weeks–months
- Recovery delay: Suppressants block brain’s healing
Reality: 24–72 hours maximum; weeks–months use unjustifiable!
3. Anticholinergics: Effective Motion Sickness, Dangerous Elderly
Drugs:
- Scopolamine (patch), Atropine
How:
- Muscarinic receptors block
Benefits:
- Motion sickness सबसे effective drug
Problems—SEVERE in 65+:
- Anticholinergic toxicity: Confusion, delirium, hallucinations
- Urinary retention: UTI, kidney damage
- Cognitive decline: Dementia risk increase
- Vision blur: Tear production reduce
- Constipation: Severe
Reality: Travel motion sickness okay; chronic vertigo में NO।
Central Compensation: Brain की Healing Process
कैसे Brain Heal होता है?
Inner ear injury → asymmetric signals → dizziness।
Brain’s remarkable ability: Central compensation।
Brain learn करता है:
- Damaged ear के signals ignore करना
- Vision rely करना
- Proprioception (floor feeling) rely करना
- Healthy ear signals use करना
Recovery Timeline (without suppressants)
- Days 1–3: Severe vertigo (body’s natural response)
- Days 4–7: Central compensation शुरू
- Weeks 2–4: Noticeable improvement
- Weeks 4–8: 80–90% resolution
- Months 2–3: Full functional recovery
With continuous suppressants: Months या years chronic dizziness!
Key: Sensory Mismatch
Brain को dizziness experience करना पड़ता है सीखने के लिए। Suppressants हटा देते हैं signal → brain learn नहीं कर सकता।
How Suppressants Block Recovery
Analogy: Car का check engine light on है। Instead of fixing engine, light tape कर दो। Light gone लेकिन engine broken!
Suppressants same: Silence signals but don’t fix problem।
Clinical Evidence
- Short-term: Symptoms reduce
- Long-term: Recovery PROLONG होता है (not improve!)
- Central compensation: Delayed या absent
- Result: Longer illness
The Cycle
- Acute attack
- Suppressant → Better
- Patient continue medicine
- Compensation blocked → Dizziness persist
- Patient = “still dizzy, so need more medicine”
- Months pass, medication dependent
- Chronic dizziness (months/years)
Elderly: Heightened Risk
65+ में suppressants = PUBLIC HEALTH CRISIS।
Why Vulnerable?
Age-related decline:
- Vestibular function naturally decrease
- Vision compromise
- Proprioception reduce
Suppressant add करो = PERFECT STORM।
Falls: CRITICAL RISK
- 1/3 adults 65+ fall yearly
- Leading cause death/injury
- Hip fracture = loss independence
Suppressants 50–80% fall risk increase करते हैं!
Example: 78-year-old mild vestibular neuritis → meclizine → brain fog → night = fall → hip fracture → independent नहीं! Medicine = injury का कारण बन गई!
Drug-Induced Parkinsonism
Antihistamines/anticholinergics:
- Tremors
- Rigidity
- Slow movement
- Shuffling gait
Many elderly = misdiagnosed “Parkinson’s” actually DRUG-INDUCED (reversible!)।
Withdrawal and Rebound: Stopping Kaise Mushkil?
Suppressant लेने के बाद days में body adapt करता है। Abruptly stop → rebound।
Rebound Vertigo: The Misunderstanding
What happens: Brain suppress के बाद suddenly awake → signals return strong → acute vertigo फिर से (worse भी हो सकता है) + nausea + anxiety।
What it means: NOT disease recurrence! Brain WAKING UP! GOOD SIGN!
Duration: Usually 24–72 hours, then resolves।
The Trap Deepens
Patient misunderstands:
- Worse लगता है after stopping
- Scared हो जाता है
- Medicine फिर से शुरू करता है
- Rebound disappears (medication suppress किया)
- Patient = “Medicine ही save करता है!”
- Years of use follow!
Benzodiazepine Withdrawal: MORE SERIOUS
Benzodiazepines:
- Severe anxiety, panic
- Tremors
- Seizures (severe cases)
- Psychological dependence
Must taper slowly (weeks–months), NOT abruptly।
Conditions Where Pills Completely Fail
1. BPPV: Mechanical, Not Chemical
Most common (20–40% vertigo)। Suppressants = completely ineffective।
Why: BPPV = calcium crystals wrong place में। Physical problem = physical solution need।
Pills क्या कर सकते हैं: Nothing!
What works:
- Dix-Hallpike test (diagnose)
- Epley या Semont maneuver (cure)
- Success: 80–90% single maneuver से!
The trap: BPPV patient → meclizine → crystals अभी wrong position में → weeks मeclizine लेता है लेकिन Epley कभी नहीं! If Epley दिया जाता Day 1 पे = 5 minute cure!
2. PPPD: Pills Worse कर देते हैं
PPPD (Persistent Postural-Perceptual Dizziness) = brain’s balance filter “stuck” in alert state।
Why suppressants fail:
- Can’t reset stuck filter
- Sedation + cognitive effects = PPPD symptoms WORSE
- Better responds to CBT, exposure, VRT
Trap: PPPD patient → benzodiazepines → brain fog, fatigue worse → symptoms worse → higher doses!
3. Vestibular Migraine: Prevention, Not Suppression
Migraine + vertigo। Suppressants ≠ help।
What works:
- Preventative: Propranolol, topiramate, CGRP
- VRT
- Trigger avoidance
When Appropriate? The 72-Hour Rule
First 24 hours:
- Suppressants appropriate
- Goal: Stop vomiting, rest
- Drugs: Meclizine, short-term lorazepam
24–72 hours:
- Still may be needed if severe
- Begin gentle mobilization simultaneously
- Plan for taper
Beyond 72 hours:
- STOP!
- Suppressants discontinue/taper
- VRT begin
- Activity encouraged
Rare exceptions (>72 hours):
- Severe Menière’s unable keep fluids (max 1–2 weeks)
- Hospitalized severe vestibular neuritis (acute phase only)
- Uncontrolled migraine (migraine-specific meds, NOT suppressants)
Exit Strategy: 3 Pillars
Pillar 1: Supervised Taper
Never abrupt stop!
Antihistamines (Meclizine):
- Reduce every 3–5 days
- 1–2 weeks taper
- Mild rebound 24–72 hours (normal!)
Benzodiazepines (Valium, Ativan):
- SLOW taper: 10% per week
- 2–3 months या longer
- Medical supervision required
- Expect anxiety, tremors (temporary)
Anticholinergics (Scopolamine):
- Smaller patch या shorter duration
- 1–2 weeks
- Cognitive sharpening as clears
Pillar 2: Early Mobilization
Brain needs movement to heal! Even slightly dizzy, gentle activity = strongest compensation trigger।
What to do:
- Walking: 10–15 min, 2–3× daily
- Head movements: Gentle rotations, flexion/extension
- Visual tracking: Follow moving object
- Balance challenges: One-leg stand, heel-to-toe
- Progress gradually: Increase as tolerate
Why: Each dizziness experience where nothing bad happens = brain recalibration।
What NOT:
- ❌ Bed rest में बैठना dark room में
- ❌ Neck collar
- ❌ Activity avoid करना fear से
Pillar 3: Vestibular Rehabilitation Therapy (VRT)
Specialized exercises = brain adaptation speed up.
Includes:
- Gaze stabilization: Eye fixation during head movement
- Balance training: Unstable surfaces, tandem stance
- Habituation: Motion-provocative stimuli exposure
- Proprioceptive training: Body position awareness
- Functional training: Real activities (driving, crowds)
Efficacy: 60–80% पeri peripheral vestibular dysfunction में।
Timeline:
- Weeks 1–2: Basic home exercises
- Weeks 2–4: PT if available
- Weeks 4–8: Advanced training
- Weeks 8–12: Fine-tuning
Medication Safety Table (Hinglish + Key Data)
| Medicine | Type | कैसे काम करता है | Short-Term | Side Effects | Addiction | Duration | Stop कब करो |
|---|---|---|---|---|---|---|---|
| Meclizine | Antihistamine | H1 block | Moderate | Sedation, brain fog | Low | 24–72 hrs | Day 3–4, taper 1–2 week |
| Dramamine | Antihistamine | H1 + anticholinergic | Moderate | Stronger sedation | Low | 24–48 hrs | Day 2–3, taper |
| Diazepam | Benzodiazepine | GABA enhance | HIGH | Sedation, cognitive issues | VERY HIGH | 24–72 hrs MAX | Day 3–4, slow weeks–months |
| Lorazepam | Benzodiazepine | GABA enhance | HIGH | Sedation, dependence | VERY HIGH | 24–72 hrs MAX | Day 3–4, slow weeks–months |
| Scopolamine | Anticholinergic | Muscarinic block | Very High | Confusion, retention | Moderate | 72 hrs (patch) | After travel, taper 1–2 week |
Safe Taper Protocol
Less Than 1 Week पर हो:
- Days 1–3: Continue dose
- Day 4: 50% reduce (e.g., 25 mg 3× = 25 mg 1–2×)
- Day 6: As-needed only
- Day 8: Stop
- After: Rebound dizziness 24–72 hours (NORMAL!)
- Simultaneously: Begin head movements, walking
1–4 Weeks पर हो:
- Week 1: Continue + gentle mobilization शुरू करो
- Week 2: 25% reduce
- Week 3: 1× daily या as-needed
- Week 4: Stop
- After: Rebound expect करो, exercise intensity increase करो
- Weeks 5–12: VRT with PT
Benzodiazepines: 10–25% per week (slower), medical supervision।
4+ Weeks पर हो (TRAPPED):
- Vestibular evaluation schedule करो
- Dix-Hallpike या HINTS माँगो
- VRT referral लो
- Taper protocol discuss करो
- Don’t stop abruptly!
Taper: 10–25% per week (benzodiazepines: 10% केवल)।
Support: Counseling, CBT helpful।
Supervision: Medical required.
Conclusion
Vertigo medicine = double-edged sword। Short-term relief ✓। Long-term trap ✓।
If weeks–months medicine take करते हो और still dizzy? Trap में हो।
Real recovery = suppression से नहीं, challenge से।
3 pillars = evidence-based path:
- Supervised taper
- Early mobilization
- VRT
Recovery possible है। Trap escape कर सकते हो। Brain adapt करने capable है।
HINDI VERSION
Vertigo Medication Trap: कैसे ये Pills आपको Dizzy बना रहे हैं (Not Better)
Introduction: अच्छे इरादों का Trap
Vertigo = सबसे common reason लोग doctor देखते हैं (neurology, ENT में 30% consultations)। Spinning world = terrifying। Instinct = तुरंत pill लेना। लेकिन बिल्कुल यह instinct millions को medication trap में डालती है।
Typical journey: Acute vertigo attack → Doctor prescribes meclizine/Valium/scopolamine → अच्छा लगता है → Weeks pass → Still dizzy → Still medication पर dependent!
यह है medication trap।
The Paradox of Dizziness Medication
Key truth: Vertigo medications treat लक्षण, NOT underlying cause।
Patients = varied sensations (violent rotation, floating, lightheaded)। Clinical settings में = “vestibular suppressants” prescribe किए जाते हैं। Short-term = relief (nausea कम)। Long-term = recovery block होती है।
Paradox: Medicine अभी अच्छा लगता है, but later recovery prevent करता है।
कौन हैं Culprits? Understanding the Classes
1. Antihistamines: Common, Sedating, Bad Long-Term
Drugs:
- Meclizine (Antivert) – Most common
- Cyclizine, Dimenhydrinate (Dramamine) – OTC available
कैसे काम करता है:
- H1 receptors block करते हैं vestibular nuclei में
- Motion sensitivity कम करता है
Benefits:
- Nausea कम, 30 min में effect
Problems:
- Sedation, brain fog, dry mouth, blurred vision
- Recovery delay करते हैं
- Tolerance develop होता है (higher dose needed)
- Rebound symptoms (stopping = worse dizziness)
Reality: 24–48 hours appropriate; उससे ज्यादा = recovery obstacle।
2. Benzodiazepines: Powerful, Addictive, DANGEROUS
Drugs:
- Diazepam (Valium), Lorazepam (Ativan), Alprazolam (Xanax)
कैसे काम करता है:
- GABA enhance करते हैं (inhibitory neurotransmitter)
- Severe vestibular suppression
Benefits:
- Very effective short-term (violent Menière’s में)
- Sleep में मदद
Problems—CRITICAL:
- Addiction: Tolerance days में develop होता है
- Cognitive impairment: Memory, confusion
- Falls: Elderly में especially—fractures, deaths
- Dependency: Weeks में हो सकता है
- Dangerous withdrawal: Abrupt stop = seizures
- Slow taper needed: Weeks–months
- Recovery delay: Suppressants block brain की healing
Reality: 24–72 hours maximum; weeks–months use unjustifiable!
3. Anticholinergics: Effective Motion Sickness, Dangerous Elderly
Drugs:
- Scopolamine (patch), Atropine
कैसे काम करता है:
- Muscarinic receptors block
Benefits:
- Motion sickness का सबसे effective drug
Problems—SEVERE in 65+:
- Anticholinergic toxicity: Confusion, delirium, hallucinations
- Urinary retention: UTI, kidney damage
- Cognitive decline: Dementia risk increase
- Vision blur: Tear production reduce
- Constipation: Severe
Reality: Travel motion sickness ठीक है; chronic vertigo में NO।
Central Compensation: Brain की Healing Process
Brain कैसे Heal होता है?
Inner ear injury → asymmetric signals → dizziness।
Brain की remarkable ability: Central compensation।
Brain सीखता है:
- Damaged ear के signals ignore करना
- Vision पर rely करना
- Proprioception (floor की feeling) पर rely करना
- Healthy ear की signals use करना
Recovery Timeline (without suppressants)
- Days 1–3: Severe vertigo (body का natural response)
- Days 4–7: Central compensation शुरू होता है
- Weeks 2–4: Noticeable improvement
- Weeks 4–8: 80–90% resolution
- Months 2–3: Full functional recovery
With continuous suppressants: Months या years chronic dizziness!
Key: Sensory Mismatch
Brain को dizziness experience करनी पड़ती है सीखने के लिए। Suppressants हटा देते हैं signal → brain सीख नहीं सकता।
How Suppressants Block Recovery
Analogy: Car का check engine light on है। Instead of engine fix करने के, light को tape कर दो। Light gone लेकिन engine broken है—और worse हो रहा है!
Suppressants same: Silence signals लेकिन problem fix नहीं करता।
Clinical Evidence
- Short-term: Symptoms कम होते हैं
- Long-term: Recovery PROLONG होता है (improve नहीं!)
- Central compensation: Delayed या absent
- Result: Longer illness
The Cycle
- Acute attack
- Suppressant → Better
- Patient continue medicine
- Compensation blocked → Dizziness persist
- Patient = “still dizzy, so need more medicine”
- Months pass, medication dependent
- Chronic dizziness (months/years)
Elderly: Heightened Risk
65+ में suppressants = PUBLIC HEALTH CRISIS।
Why Vulnerable?
Age-related decline:
- Vestibular function naturally decrease
- Vision compromise
- Proprioception reduce
Suppressant add करो = PERFECT STORM।
Falls: CRITICAL RISK
- 1/3 adults 65+ fall yearly
- Leading cause death/injury
- Hip fracture = loss of independence
Suppressants 50–80% fall risk increase करते हैं!
Example: 78-year-old mild vestibular neuritis → meclizine → brain fog → night = fall → hip fracture → independent नहीं! Medicine = injury का कारण बन गई!
Drug-Induced Parkinsonism
Antihistamines/anticholinergics:
- Tremors
- Rigidity
- Slow movement
- Shuffling gait
Many elderly = misdiagnosed “Parkinson’s” actually DRUG-INDUCED (reversible!)।
Withdrawal and Rebound: Stopping कैसे Mushkil?
Suppressant लेने के बाद days में body adapt करता है। Abruptly stop → rebound।
Rebound Vertigo: The Misunderstanding
क्या होता है: Brain suppress के बाद suddenly awake → signals return strong → acute vertigo फिर से (worse भी हो सकता है) + nausea + anxiety।
इसका मतलब: NOT disease recurrence! Brain WAKING UP! GOOD SIGN!
Duration: Usually 24–72 hours, फिर resolve।
The Trap Deepens
Patient misunderstands:
- Worse लगता है after stopping
- Scared हो जाता है
- Medicine फिर से शुरू करता है
- Rebound disappears (medication suppress किया)
- Patient = “Medicine ही save करता है!”
- Years of use follow!
Benzodiazepine Withdrawal: MORE SERIOUS
Benzodiazepines:
- Severe anxiety, panic
- Tremors
- Seizures (severe cases)
- Psychological dependence
Must taper slowly (weeks–months), NOT abruptly।
Conditions Where Pills Completely Fail
1. BPPV: Mechanical, Not Chemical
Most common (20–40% vertigo)। Suppressants = completely ineffective।
क्यों: BPPV = calcium crystals wrong place में। Physical problem = physical solution चाहिए।
Pills क्या कर सकते हैं: Nothing!
क्या काम करता है:
- Dix-Hallpike test (diagnose)
- Epley या Semont maneuver (cure)
- Success: 80–90% single maneuver से!
The trap: BPPV patient → meclizine → crystals अभी wrong position में → weeks meclizine लेता है लेकिन Epley कभी नहीं! If Epley दिया जाता Day 1 पे = 5 minute cure!
2. PPPD: Pills Worse कर देते हैं
PPPD (Persistent Postural-Perceptual Dizziness) = brain की balance filter “stuck” in alert state में।
क्यों suppressants fail:
- Can’t reset stuck filter
- Sedation + cognitive effects = PPPD symptoms WORSE
- Better respond करता है CBT, exposure, VRT को
Trap: PPPD patient → benzodiazepines → brain fog, fatigue worse → symptoms worse → higher doses!
3. Vestibular Migraine: Prevention, Not Suppression
Migraine + vertigo। Suppressants ≠ help।
क्या काम करता है:
- Preventative: Propranolol, topiramate, CGRP
- VRT
- Trigger avoidance
कब Appropriate है? The 72-Hour Rule
First 24 hours:
- Suppressants appropriate
- Goal: Stop vomiting, rest
- Drugs: Meclizine, short-term lorazepam
24–72 hours:
- Still may be needed अगर severe
- Begin gentle mobilization simultaneously
- Plan for taper
Beyond 72 hours:
- STOP!
- Suppressants discontinue/taper करो
- VRT begin करो
- Activity encourage करो
Rare exceptions (>72 hours):
- Severe Menière’s unable keep fluids (max 1–2 weeks)
- Hospitalized severe vestibular neuritis (acute phase only)
- Uncontrolled migraine (migraine-specific meds, NOT suppressants)
Exit Strategy: 3 Pillars
Pillar 1: Supervised Taper
Never abrupt stop!
Antihistamines (Meclizine):
- Reduce every 3–5 days
- 1–2 weeks taper
- Mild rebound 24–72 hours (normal!)
Benzodiazepines (Valium, Ativan):
- SLOW taper: 10% per week
- 2–3 months या longer
- Medical supervision required
- Expect anxiety, tremors (temporary)
Anticholinergics (Scopolamine):
- Smaller patch या shorter duration
- 1–2 weeks
- Cognitive sharpening as clears
Pillar 2: Early Mobilization
Brain को movement चाहिए heal होने के लिए! Even slightly dizzy, gentle activity = strongest compensation trigger।
क्या करो:
- Walking: 10–15 min, 2–3× daily
- Head movements: Gentle rotations, flexion/extension
- Visual tracking: Follow moving object
- Balance challenges: One-leg stand, heel-to-toe
- Progress gradually: Increase as tolerate
क्यों: Each dizziness experience जहाँ कुछ bad नहीं होता = brain recalibration।
क्या NOT करो:
- ❌ Bed rest में बैठना dark room में
- ❌ Neck collar
- ❌ Activity avoid करना fear से
Pillar 3: Vestibular Rehabilitation Therapy (VRT)
Specialized exercises = brain adaptation speed up करते हैं।
Includes:
- Gaze stabilization: Eye fixation during head movement
- Balance training: Unstable surfaces, tandem stance
- Habituation: Motion-provocative stimuli exposure
- Proprioceptive training: Body position awareness
- Functional training: Real activities (driving, crowds)
Efficacy: 60–80% peripheral vestibular dysfunction में।
Timeline:
- Weeks 1–2: Basic home exercises
- Weeks 2–4: PT अगर available
- Weeks 4–8: Advanced training
- Weeks 8–12: Fine-tuning
Medication Safety Table (Hindi + Key Data)
| Medicine | Type | कैसे काम करता है | Short-Term | Side Effects | Addiction | Duration | कब Stop करो |
|---|---|---|---|---|---|---|---|
| Meclizine | Antihistamine | H1 block | Moderate | Sedation, brain fog | Low | 24–72 hrs | Day 3–4, taper 1–2 week |
| Dramamine | Antihistamine | H1 + anticholinergic | Moderate | Stronger sedation | Low | 24–48 hrs | Day 2–3, taper |
| Diazepam | Benzodiazepine | GABA enhance | HIGH | Sedation, cognitive issues | VERY HIGH | 24–72 hrs MAX | Day 3–4, slow weeks–months |
| Lorazepam | Benzodiazepine | GABA enhance | HIGH | Sedation, dependence | VERY HIGH | 24–72 hrs MAX | Day 3–4, slow weeks–months |
| Scopolamine | Anticholinergic | Muscarinic block | Very High | Confusion, retention | Moderate | 72 hrs (patch) | After travel, taper 1–2 week |
Safe Taper Protocol
Less Than 1 Week पर हो:
- Days 1–3: Continue dose
- Day 4: 50% reduce (e.g., 25 mg 3× = 25 mg 1–2×)
- Day 6: As-needed only
- Day 8: Stop
- After: Rebound dizziness 24–72 hours (NORMAL!)
- Simultaneously: Begin head movements, walking
1–4 Weeks पर हो:
- Week 1: Continue + gentle mobilization शुरू करो
- Week 2: 25% reduce
- Week 3: 1× daily या as-needed
- Week 4: Stop
- After: Rebound expect करो, exercise intensity increase करो
- Weeks 5–12: VRT with PT
Benzodiazepines: 10–25% per week (slower), medical supervision।
4+ Weeks पर हो (TRAPPED):
- Vestibular evaluation schedule करो
- Dix-Hallpike या HINTS माँगो
- VRT referral लो
- Taper protocol discuss करो
- Don’t stop abruptly!
Taper: 10–25% per week (benzodiazepines: 10% केवल)।
Support: Counseling, CBT helpful।
Supervision: Medical required.
Conclusion
Vertigo medicine = double-edged sword। Short-term relief ✓। Long-term trap ✓।
अगर weeks–months medicine लेते हो और still dizzy? Trap में हो।
Real recovery = suppression से नहीं, challenge से।
3 pillars = evidence-based path:
- Supervised taper
- Early mobilization
- VRT
Recovery possible है। Trap escape कर सकते हो। Brain adapt करने capable है।
MEDICATION COMPARISON TABLE: SAFETY, EFFICACY, TIMELINE
(Reference Guide for Patients and Clinicians)
Complete Drug Comparison Matrix
| Drug Class | Specific Drug | Generic/Brand | Onset (Minutes) | Duration per Dose | Efficacy for Nausea | Efficacy for Vertigo | Sedation Level | Cognitive Impact | Fall Risk (Elderly) | Addiction Potential | Rebound Severity | Taper Duration | Special Precautions |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Antihistamine | Meclizine | Antivert | 30–60 | 4–6 hours | Moderate (60%) | Low–Moderate (30–50%) | Moderate | Mild (brain fog) | Moderate (2–3× baseline) | Low | Mild | 1–2 weeks | Avoid in glaucoma, urinary retention |
| Antihistamine | Dimenhydrinate | Dramamine (OTC) | 20–40 | 4–6 hours | Moderate–High (70%) | Low–Moderate (35–60%) | High (stronger than meclizine) | Moderate (memory issues) | Moderate–High (3–5× baseline) | Low | Mild–Moderate | 3–7 days | Anticholinergic side effects stronger |
| Antihistamine | Cyclizine | Marezine | 30 | 4–6 hours | Moderate (60%) | Low–Moderate (40–50%) | Low–Moderate (milder) | Mild | Low–Moderate | Low | Mild | 1–2 weeks | Least anticholinergic of antihistamines |
| Benzodiazepine | Diazepam | Valium (long-acting) | 15–30 | 6–12 hours | Very High (90–95%) | Very High (80–90%) | Very High (profound) | Significant (memory, confusion) | Very High (5–8× baseline) | Very High | Severe | 4–12 weeks (slow) | Never abrupt stop; seizure risk |
| Benzodiazepine | Lorazepam | Ativan (medium-acting) | 10–20 | 4–6 hours | Very High (90–95%) | Very High (80–90%) | Very High (profound) | Significant | Very High (5–8× baseline) | Very High | Severe | 4–12 weeks (slow) | Requires close supervision during taper |
| Benzodiazepine | Alprazolam | Xanax (short-acting) | 15–30 | 4–6 hours | Moderate–High | Moderate–High | High | Moderate–Significant | High (4–6× baseline) | Extremely High | Severe | NOT recommended for vertigo | Avoid; high abuse potential |
| Anticholinergic | Scopolamine | Transdermal patch | 4–8 (slow absorption) | 72 hours per patch | Very High (95%+) | Very High (80–90%) | Minimal (systemic) | Significant (confusion, delirium) | Very High in elderly (6–10× baseline) | Moderate | Moderate | 1–2 weeks | Contraindicated in glaucoma, urinary obstruction; elderly toxicity risk HIGH |
| Anticholinergic | Atropine | IV/IM systemic | Immediate (IV) | 2–4 hours | High | High | Minimal | Very High (hallucinations, delirium) | Very High | Moderate | Moderate | Variable | Rarely used for vertigo; anticholinergic toxicity prominent |
| Anticholinergic | Promethazine | Phenergan (also antihistamine) | 15–30 | 4–6 hours | Very High (90%) | High (75–85%) | Very High | Moderate–Significant | High (5–7× baseline) | Low | Moderate | 1–2 weeks | Potent anticholinergic; black box warning in pediatric <2 years |
Key Clinical Decision Points
For Acute Vertigo (First 24–72 Hours):
- Best short-term efficacy: Benzodiazepines (lorazepam, diazepam) or promethazine
- Less addictive alternative: Meclizine (if moderate symptoms)
- Dose: As needed during acute phase only
- Stop by: Day 3–4 latest
For Ongoing Management (If Needed Beyond 72 Hours):
- ❌ Do NOT continue benzodiazepines (addiction risk)
- ❌ Do NOT use scopolamine patches (anticholinergic toxicity)
- ✅ Early mobilization + VRT is superior
- ✅ Switch to vestibular-specific treatment (not chemical suppression)
For Elderly Patients:
- ⚠️ Meclizine: Acceptable short-term (24–48 hours) only
- ⚠️⚠️ Benzodiazepines: HIGH RISK (falls, cognitive decline, mortality increase)
- ⚠️⚠️⚠️ Anticholinergics (scopolamine, atropine, promethazine): EXTREME RISK (delirium, falls, urinary retention)
- ✅ Best option: Non-pharmacological (VRT, mobilization) if possible
SAFE MEDICATION TAPER PROTOCOL: STEP-BY-STEP
(Patient & Clinician Reference)
Protocol for <1 Week of Use (Most Common)
DAY 1–3: Take medication as prescribed
↓
DAY 4: Reduce dose by 50% (morning dose only, or skip midday dose)
↓
DAY 6: Take only as-needed doses (not scheduled)
↓
DAY 8: Discontinue
↓
AFTER DISCONTINUATION: Expect mild rebound dizziness 24–72 hours (normal!)
↓
SIMULTANEOUSLY: Begin head movements, walking (5–10 min, 2–3×/day)Expected timeline: 8 days to full discontinuation
Rebound severity: Mild (manageable at home)
Next step: Start VRT if symptoms persist >1 week
Protocol for 1–4 Weeks of Use
WEEK 1: Continue current dose + BEGIN gentle mobilization
• Walk 10–15 min daily
• Gentle head rotations
• Do NOT remain bedbound
↓
WEEK 2: Reduce dose by 25%
• Example: Meclizine 25 mg 3× daily → 25 mg 2× daily
• Monitor for rebound (should be mild at this point)
↓
WEEK 3: Further reduce to minimal (25 mg 1× daily OR as-needed only)
↓
WEEK 4: Discontinue medication
↓
AFTER DISCONTINUATION: Expect mild–moderate rebound dizziness 24–72 hours
↓
WEEKS 5–12: Structured VRT (PT 2–3×/week if available)Expected timeline: 4 weeks to full discontinuation
Rebound severity: Mild–Moderate (may need some rest, but functional)
Medical supervision: Recommended (phone check-ins)
VRT: Essential
Protocol for 4+ Weeks of Use (TRAPPED IN CYCLE)
IMMEDIATE: Schedule vestibular evaluation
• Dix-Hallpike test (if positional vertigo)
• HINTS exam (if continuous vertigo)
• Confirm diagnosis
↓
WEEKS 1–2: Medication tapering + VRT initiation
• Reduce dose 10–25% per week
• VRT PT 2–3×/week
↓
WEEKS 2–4: Continue taper + intensive VRT
• Exercise increase in difficulty
• Mobility increase
↓
WEEKS 4–8: VRT continues; medication reduced further
↓
MONTHS 2–3: Full discontinuation expected
• Some residual dizziness may persist (from deconditioning)
• VRT should continue 8–12 weeks total
↓
AFTER 3 MONTHS: Most patients 80–90% improvedExpected timeline: 8–12 weeks to full discontinuation + recovery
Medical supervision: REQUIRED (complex taper, multiple medication interactions possible)
VRT: Essential; work with PT specializing in vestibular
Psychological support: Consider if anxiety or depression concurrent
Special Protocol: BENZODIAZEPINE TAPER (>1 Week Use)
⚠️ CRITICAL: Benzodiazepines require slower taper than other drugs
WEEK 1–2: Continue current dose
• Discuss taper plan with doctor
• Establish baseline anxiety level
• Begin gentle mobilization (walking, head movements)
↓
WEEKS 3 ONWARD: Reduce dose by 10% per week MAXIMUM
• Example: Diazepam 10 mg 3× daily (30 mg total)
Week 3: Reduce to 27 mg/day
Week 4: Reduce to 24 mg/day
Week 5: Reduce to 21.6 mg/day
(Continuing ~10% reduction each week)
↓
EXPECTED TAPER DURATION: 8–16 weeks (sometimes 24 weeks for high doses)
↓
DURING TAPER: Expect intermittent anxiety, tremors, rebound dizziness
• These are TEMPORARY
• Symptoms peak before dose reduction, then improve
• NEVER stop suddenly (seizure risk)
↓
SUPPORT STRATEGIES DURING TAPER:
• Cognitive-behavioral therapy (CBT) helpful
• Stress management, sleep hygiene
• Supportive counseling
• Group support for people tapering benzodiazepines
• Avoid alcohol, other CNS depressants
↓
MEDICAL SUPERVISION: Required for entire taper
• Weekly or biweekly phone/in-person check-ins
• Medication adjustment if withdrawal symptoms severe
• Psychiatric referral if anxiety uncontrolled
↓
AFTER DISCONTINUATION: Recovery continues
• Brain neuroplasticity takes weeks to months
• Cognitive and emotional improvements gradual
• Sleep improvement may take 2–3 months
↓
LONG-TERM (6–12 MONTHS): Most patients achieve full baseline
• Mood, cognition, sleep normalize
• VRT should continue through this period
• Vestibular compensation completesKey point: Benzodiazepine tapering is a marathon, not a sprint. Patience and medical support are essential.
FAQs
>
ENGLISH FAQs (20 Questions)
1. Why do vertigo medications actually prevent recovery?
Answer: Vertigo medications work by suppressing the vestibular system—essentially “quieting” the signals from the inner ear and brainstem. However, true recovery requires a process called “central compensation,” where the brain learns to rely on other senses (vision, proprioception) to compensate for inner ear dysfunction. Suppressants block this natural healing process by removing the sensory signals the brain needs to adapt. In the short term (24–72 hours), suppressants feel good by reducing nausea. In the long term (weeks–months), they prolong dizziness by preventing central compensation from occurring.
2. Is the 72-hour rule absolute, or can medications be used longer?
Answer: The 72-hour rule is a guideline, not an absolute cutoff. In most cases, suppressants should be discontinued by 72 hours because beyond that point, they delay recovery more than they help. However, there are rare exceptions: (1) Severe Menière’s attacks with persistent vomiting—medication may be needed 1–2 weeks if the patient cannot keep fluids down; (2) Hospitalized acute vestibular neuritis—medications used during the acute phase only; (3) Uncontrolled migraine with severe vertigo—migraine-specific medications (not suppressants) may be needed. The key is: If a patient is on suppressants beyond 72 hours WITHOUT a specific diagnosis or concurrent VRT, they are likely in the trap.
3. Why do patients experience severe dizziness when they stop taking vertigo medications?
Answer: This is called “rebound dizziness,” and it is a sign that the brain is recovering, not a sign of disease recurrence. When suppressants are active, the vestibular system is chemically quieted. When the medication is discontinued, the brain—which has been artificially suppressed—suddenly “wakes up.” The re-emergence of vestibular signals, combined with the brain’s recalibration, causes temporary severe dizziness, usually lasting 24–72 hours. This is temporary and self-limited. Many patients mistakenly interpret rebound as disease recurrence and resume medication, deepening the trap. Patient education about rebound is critical to successful medication discontinuation.
4. Can BPPV be treated with medication?
Answer: No. BPPV is a mechanical problem—calcium carbonate crystals have migrated into the wrong part of the inner ear. No medication can move these crystals back to their correct location. Suppressants may reduce nausea slightly, but they do NOT cure BPPV and do NOT allow the crystals to reposition naturally. The only effective treatment is a physical maneuver: the Epley or Semont maneuver, which has an 80–90% cure rate in a single session. A patient with BPPV should be referred for diagnostic Dix-Hallpike testing and immediate Epley maneuver, not prescribed suppressants. If a patient is on suppressants for BPPV and has not received a Dix-Hallpike test or Epley maneuver, the treatment approach needs to be revised immediately.
5. Why are benzodiazepines so dangerous for elderly patients?
Answer: Benzodiazepines significantly increase fall risk, cognitive decline, and mortality in elderly patients (age 65+). The mechanism is multifaceted: (1) Sedation and cognitive impairment reduce balance and reaction time; (2) Elderly patients already have natural decline in vestibular, visual, and proprioceptive function—adding benzodiazepines on top creates a “perfect storm”; (3) Benzodiazepines increase fall risk by 50–80% in elderly, and falls are a leading cause of death in this age group; (4) Long-term use is associated with dementia-like cognitive decline and depression. For elderly patients with vestibular disorders, benzodiazepines should be avoided if possible. If absolutely necessary for severe acute attacks, duration should not exceed 48 hours. Non-pharmacological approaches (VRT, early mobilization) are far safer and more effective.
6. Is meclizine safe for long-term use?
Answer: No. While meclizine is often prescribed as “safer” than benzodiazepines, it is NOT appropriate for long-term use. Long-term meclizine causes: (1) Persistent sedation and brain fog; (2) Dry mouth, blurred vision, constipation; (3) Tolerance—the body adapts and higher doses become necessary; (4) Delayed central compensation—the brain’s natural healing is blocked. Clinical studies show that patients on meclizine for more than 1–2 weeks have prolonged dizziness compared to those who receive early VRT without medication. Meclizine is appropriate for perhaps 24–48 hours during an acute attack, then should be tapered. If a patient is on meclizine for weeks or months, it should be discontinued and VRT initiated.
7. What is anticholinergic toxicity and why are anticholinergic drugs dangerous?
Answer: Anticholinergic drugs (scopolamine, atropine, some antihistamines) block acetylcholine in the brain and body, causing a distinctive syndrome called “anticholinergic toxicity.” Symptoms include confusion, delirium, agitation, hallucinations, urinary retention, dry mouth, blurred vision, constipation, and increased heart rate. Elderly patients are extremely vulnerable. Anticholinergic burden (accumulation of multiple anticholinergic medications) is associated with increased dementia risk and falls. Scopolamine patches, which are very effective for motion sickness, are particularly problematic when used chronically because they deliver continuous anticholinergic effects for 72 hours per patch. Scopolamine should be used only for travel-related motion sickness (brief duration) and never for chronic vertigo management.
8. What is the difference between rebound dizziness and the disease worsening?
Answer: Rebound dizziness (good sign): Occurs within 24 hours of medication discontinuation; temporary (usually resolves in 24–72 hours); worsens then improves; patient can function; no new neurological symptoms. This indicates the brain is waking up after chemical suppression.
Disease worsening (bad sign): Progressive over days–weeks; persistent beyond 72 hours; accompanied by new symptoms (weakness, speech difficulty, vision loss, severe headache); patient progressively less functional. This requires urgent imaging (MRI brain) to rule out central causes.
Key: If dizziness worsens immediately after stopping medication but then improves over 72 hours, it is rebound. If dizziness worsens progressively days after stopping, it may indicate disease and requires medical evaluation.
9. Can a patient safely taper benzodiazepines at home without medical supervision?
Answer: No. Benzodiazepine tapering must be done under medical supervision because: (1) Abrupt discontinuation can cause seizures; (2) Slow tapering (10% per week) requires medical guidance and dose adjustment; (3) Withdrawal anxiety and physical symptoms need monitoring; (4) Comorbid depression or anxiety may worsen during taper, requiring medication adjustment or psychiatric support. Benzodiazepines should never be stopped “cold turkey.” A supervised taper over 8–16 weeks is necessary. Medical supervision can be via phone for follow-ups, but initial assessment and taper plan require in-person evaluation. Some patients benefit from psychiatric support or cognitive-behavioral therapy during benzodiazepine withdrawal.
10. What should a patient do if they’ve been on vertigo medications for months or years?
Answer: (1) Schedule a vestibular evaluation: Dix-Hallpike test (if positional), HINTS exam (if constant). Confirm actual diagnosis. (2) Request VRT referral: Physical therapy specializing in vestibular disorders. Start immediately, even while on medication. (3) Discuss medication taper with doctor: Use the taper protocol provided. For benzodiazepines, taper 10% per week over 8–16 weeks. For antihistamines/anticholinergics, taper faster (1–2 weeks). (4) Begin early mobilization: Even while on medication, encourage gentle walking, head movements. (5) Expect rebound: When medication is stopped, dizziness may worsen temporarily (24–72 hours). This is normal. (6) Monitor symptoms: If new neurological symptoms develop (weakness, speech difficulty, vision loss), seek urgent care. (7) Long-term plan: VRT should continue 8–12 weeks minimum. Most patients achieve 80–90% improvement with combined supervised taper + VRT.
11. Are there any vertigo medications that actually help recovery (not just suppress)?
Answer: Most “vertigo medications” suppress rather than heal. However, certain medications address underlying causes: (1) Migraine-preventative medications (for vestibular migraine): Propranolol, topiramate, amitriptyline, CGRP monoclonal antibodies—these address the migraine mechanism, not vertigo per se, but reduce migraine-associated dizziness; (2) Diuretics (for Menière’s disease): Reduce endolymphatic fluid pressure; moderate evidence of benefit. (3) Vestibular-specific rehabilitation: Not a medication, but VRT combined with appropriate positioning maneuvers (Epley for BPPV) actually treats the underlying problem. For most common causes of vertigo (BPPV, vestibular neuritis), the goal should be early diagnosis + physical treatment (maneuvers, VRT), not medication.
12. What is the difference between vestibular suppressants and migraine-preventative medications?
Answer: Vestibular suppressants (antihistamines, benzodiazepines, anticholinergics) chemically quiet the vestibular system. They do not address underlying causes and delay central compensation. They are appropriate only for 24–72 hours of acute severe vertigo.
Migraine-preventative medications address the physiological mechanism of migraine (neuronal hyperexcitability, inflammation, neurotransmitter imbalance). Examples: propranolol (beta-blocker), topiramate (anticonvulsant), amitriptyline (tricyclic antidepressant), CGRP monoclonal antibodies (newer class). These medications reduce migraine frequency and severity, including vestibular migraine attacks. They take weeks–months to become effective and are meant for long-term use in patients with recurring migraines.
Key difference: Suppressants block symptoms; preventatives reduce disease recurrence. For vestibular migraine, preventatives are appropriate long-term; suppressants are not.
13. How does VRT (vestibular rehabilitation therapy) compare to medication for treating vertigo?
Answer: VRT is superior to medication for most vertigo conditions:
- Efficacy: VRT is effective in 60–80% of patients with peripheral vestibular disorders; suppressive medications delay recovery by prolonging illness duration
- Mechanism: VRT promotes central compensation (the brain’s natural healing); suppressants block it
- Timeline to improvement: VRT effects visible in weeks; medication provides only temporary symptomatic relief
- Side effects: VRT causes no serious side effects; medications cause sedation, cognitive impairment, fall risk, addiction
- Dependency: VRT requires patient engagement but no dependency; suppressants create psychological and physical dependency
- Cost-effectiveness: VRT upfront cost is modest; medication + prolonged illness + complications becomes expensive
- Long-term outcome: VRT patients achieve normal balance function; medication-trapped patients remain dysfunctional long-term
Evidence-based approach: Early VRT (within 2 weeks of vestibular event) + minimal medication (only if necessary for severe acute nausea, <72 hours) = best outcomes.
14. Why do some doctors continue prescribing vertigo suppressants despite the evidence?
Answer: Several reasons: (1) Tradition: Older prescribing patterns persist despite updated evidence; (2) Symptomatic relief: Doctors see immediate patient relief from medication and assume it is helping recovery; (3) Lack of vestibular training: Many primary care doctors and even some specialists lack formal training in vestibular disorders and may not be familiar with central compensation physiology; (4) Convenience: Prescribing a pill takes seconds; recommending VRT requires patient education, referral coordination, and time; (5) Insurance/access barriers: VRT may not be accessible in all areas; medication is always available; (6) Patient expectations: Patients expect medication and may resist non-pharmacological recommendations. Change is occurring: Vestibular specialists increasingly recognize that suppressants delay recovery, and guidelines are shifting toward earlier, earlier VRT and minimal medication use.
15. Can someone become addicted to antihistamines like meclizine?
Answer: Meclizine has low addiction potential in the classic sense (no reward-seeking behavior, no euphoria). However, patients can develop psychological dependence: (1) They experience rebound dizziness when stopping → mistakenly interpret as disease recurrence → resume medication; (2) They become fearful of dizziness and use medication as a safety blanket; (3) They never develop central compensation because medication prevents it → they genuinely cannot function without medication (because their brain never learned to compensate). This is the medication trap: Not true addiction, but functional dependence + perpetuated dizziness. Breaking the cycle requires supervised taper + aggressive VRT + patient education about rebound.
16. Is there a safe way to transition from suppressive medication to VRT?
Answer: Yes. The transition should be gradual and supervised: (1) Weeks 1–2: Continue medication at current dose; simultaneously start VRT (physical therapy 2–3×/week). Begin gentle home exercises (walking, gaze stabilization). (2) Weeks 2–4: Gradually reduce medication dose while increasing VRT intensity and frequency. (3) Weeks 4–8: Further medication reduction; VRT continues and progresses to more challenging exercises. (4) Week 8 onward: Medication discontinued; VRT continues until symptoms resolve (typically 8–12 weeks total). The key principle: Do not stop medication abruptly; simultaneously initiate and progress VRT so the patient never experiences the shock of sudden medication withdrawal. With this approach, rebound is mild and manageable because the brain has already begun adapting through VRT.
17. What role does exercise play in vertigo recovery while on suppressants?
Answer: Exercise is essential, even while on suppressants. When patients are on medication, they often assume they should rest quietly. In fact, the opposite is true: (1) Early mobilization triggers compensation: Even while medicated, gentle movement (walking, head rotations) provides sensory input the brain needs to adapt; (2) Exercise prevents deconditioning: Bed rest while on suppressants leads to deconditioning, anxiety, and prolonged dizziness; (3) VRT accelerates recovery: Structured vestibular exercises during medication taper speed up central compensation; (4) Activity builds confidence: Gentle activity while medicated builds patient confidence that dizziness is manageable, reducing fear and anxiety. Recommendation: Even during the acute phase when medication is appropriate, encourage at least 10–15 minutes of gentle walking and head movements daily. This “active recovery” combined with early medication taper and VRT produces the best outcomes.
18. Can scopolamine patches be used safely for chronic vertigo?
Answer: No. Scopolamine patches are FDA-approved for motion sickness prevention and are very effective (95%+ efficacy). However, they are NOT appropriate for chronic vertigo management because: (1) Anticholinergic toxicity: Patches deliver continuous anticholinergic effects for 72 hours; with repeated or chronic use, toxicity accumulates (confusion, delirium, urinary retention); (2) Elderly risk: Especially dangerous in age 65+; significantly increases falls, delirium, and dementia-like symptoms; (3) Central compensation blocked: Like other suppressants, patches prevent the brain from learning to compensate; (4) Tolerance: Over time, higher doses or more frequent patches become necessary. Appropriate use: Single patch for air travel or brief motion exposure; not for weekly or monthly use; absolutely not for chronic vertigo management.
19. What is the relationship between medication-induced dizziness and true vertigo?
Answer: Medication-induced dizziness is a side effect of drugs that cause sedation, cognitive impairment, orthostatic hypotension, or anticholinergic effects. Common culprits: benzodiazepines, anticholinergics, some antihistamines, tricyclic antidepressants, antipsychotics. This dizziness is a direct effect of the medication and typically improves after discontinuation or dose reduction.
True vertigo is a pathological condition (BPPV, vestibular neuritis, migraine) that creates a sensation of spinning or movement. True vertigo requires treatment of the underlying condition, not medication to suppress it.
The trap: A patient with true vertigo is prescribed suppressants → medication causes additional dizziness/sedation as a side effect → patient feels worse overall → patient takes higher doses → worsens further. A patient may actually have BOTH true vertigo AND medication-induced dizziness. Diagnosis requires: Determining which symptoms are from the underlying vestibular disorder and which are medication side effects. This is why obtaining a clear diagnosis (Dix-Hallpike, HINTS) BEFORE prescribing long-term medication is critical.
20. If I’ve been taking vertigo medication for a long time, is recovery still possible?
Answer: Yes, absolutely. Recovery is possible even after prolonged medication use. The brain retains neuroplasticity and capacity to adapt, even after months or years of suppression. The pathway to recovery: (1) Correct diagnosis: Vestibular evaluation with Dix-Hallpike, HINTS, and if needed, vestibular testing or imaging; (2) Medication taper: Slow, supervised discontinuation (antihistamines: 1–2 weeks; benzodiazepines: 8–16 weeks); (3) VRT initiation: Physical therapy specializing in vestibular disorders, 2–3×/week for 8–12 weeks; (4) Early mobilization: Walking, head movements, balance exercises daily; (5) Patience: Recovery may take 3–6 months after medication discontinuation, but 80–90% of patients achieve functional recovery with this approach. Typical timeline: 1 month for medication taper + 2–3 months for active VRT = 3–4 months to functional recovery. The longer you’ve been on suppressants, the more time central compensation takes, but the outcome is still very positive.
HINGLISH FAQs (20 Questions)
1. Kyun vertigo medications actually recovery prevent करती हैं?
Answer: Vertigo medications = vestibular system suppress करती हैं (essence में “quiet” करती हैं inner ear + brainstem signals)। Lekin true recovery = “central compensation” process, जहाँ brain other senses पर rely सीखता है (vision, proprioception) compensate करने के लिए। Suppressants = natural healing process block करती हैं क्योंकि वो brain के signals हटा देती हैं जो brain को adapt करने चाहिए। Short-term (24–72 hours) = suppressants अच्छा लगता है (nausea कम)। Long-term (weeks–months) = dizziness PROLONG होती है क्योंकि central compensation नहीं हो पाता।
2. 72-hour rule absolute है या longer use हो सकता है?
Answer: 72-hour rule = guideline, absolute नहीं। Most cases में suppressants discontinue होनी चाहिए 72 hours में क्योंकि beyond = recovery delay more than help करता है। Rare exceptions: (1) Severe Menière’s persistent vomiting—1–2 weeks medication if keep fluids नहीं रख सकता; (2) Hospitalized acute vestibular neuritis—acute phase दौरान medication; (3) Uncontrolled migraine severe vertigo—migraine-specific meds (NOT suppressants) may needed। Key = अगर patient suppressants पर है 72 hours से बिना diagnosis या concurrent VRT के = likely TRAP में है।
3. Kyun patients को medication stop करने से severe dizziness होता है?
Answer: यह “rebound dizziness” कहलाती है = sign that brain recovering है, NOT disease recurrence। Suppressants active जब brain chemically quiet होता है। Stop करने पर brain suddenly “awake” होता है। Re-emergence of vestibular signals + brain recalibration = temporary severe dizziness, usually 24–72 hours। Temporary, self-limited। Many patients misunderstand करते हैं rebound as disease recurrence और medication फिर resume करते हैं, trap deepening। Patient education critical है।
4. BPPV को medication से treat हो सकता है?
Answer: Nahi। BPPV = mechanical problem (calcium crystals wrong place)। No medication crystals को correct location पर move नहीं कर सकती। Suppressants = nausea slightly कम लेकिन BPPV cure नहीं करता और crystals को naturally reposition नहीं करता। Only effective treatment = physical maneuver: Epley या Semont, 80–90% cure rate single session में। BPPV wala patient = Dix-Hallpike testing + immediate Epley refer होना चाहिए, NOT suppressants। अगर patient suppressants पर है BPPV के लिए बिना Dix-Hallpike या Epley के = treatment approach change करनी चाहिए।
5. Kyun benzodiazepines elderly के लिए इतने dangerous हैं?
Answer: Benzodiazepines significantly increase करते हैं fall risk, cognitive decline, mortality elderly patients में (65+)। Mechanism multifaceted: (1) Sedation + cognitive impairment = balance + reaction time reduce; (2) Elderly = natural decline vestibular, visual, proprioceptive में; benzodiazepines पर = “perfect storm”; (3) 50–80% fall risk increase elderly में, falls = leading cause death age group में; (4) Long-term = dementia-like cognitive decline + depression। Elderly + vestibular disorders के लिए benzodiazepines avoid करनी चाहिए अगर possible हो। अगर absolutely necessary severe acute के लिए = 48 hours से ज्यादा नहीं। Non-pharmacological (VRT, mobilization) = far safer + effective।
6. Kya meclizine long-term use के लिए safe है?
Answer: Nahi। Meclizine को अक्सर “safer” prescribe किया जाता है benzodiazepines के मुकाबले, lekin NOT appropriate long-term के लिए। Long-term meclizine = persistent sedation + brain fog; dry mouth, blurred vision, constipation; tolerance (higher doses needed); delayed central compensation (brain’s natural healing blocked)। Clinical studies = patients on meclizine 1–2 weeks से ज्यादा prolonged dizziness दिखते हैं compared early VRT बिना medication के। Meclizine appropriate = 24–48 hours acute attack, फिर taper। अगर patient weeks–months मeclizine पर है = discontinued होनी चाहिए + VRT initiate।
7. Anticholinergic toxicity क्या है aur kyun dangerous?
Answer: Anticholinergic drugs (scopolamine, atropine, some antihistamines) = acetylcholine block करती हैं brain + body में, distinctive syndrome = “anticholinergic toxicity”। Symptoms = confusion, delirium, agitation, hallucinations, urinary retention, dry mouth, blurred vision, constipation, increased heart rate। Elderly = extremely vulnerable। Anticholinergic burden = multiple anticholinergic meds accumulation = associated dementia risk + falls। Scopolamine patches = very effective motion sickness लेकिन problematic chronic use क्योंकि continuous anticholinergic effects 72 hours per patch। Scopolamine = only travel motion sickness (brief duration), never chronic vertigo।
8. Rebound dizziness aur disease worsening में क्या difference?
Answer: Rebound dizziness (good sign): Occurs 24 hours within discontinuation; temporary (24–72 hours); worsens फिर improves; functional; no new neuro symptoms। Brain waking up।
Disease worsening (bad sign): Progressive days–weeks; persists 72 hours beyond; new symptoms (weakness, speech, vision loss); progressively less functional। Requires urgent imaging।
Key: अगर dizziness worsens immediately after stopping medication लेकिन improves 72 hours में = rebound। अगर days बाद progressively worsens = may disease, requires evaluation।
9. Kya benzodiazepine taper घर पे safely हो सकता है बिना medical supervision?
Answer: Nahi। Benzodiazepine tapering = medical supervision required। कारण: (1) Abrupt discontinuation = seizures possible; (2) Slow tapering (10% per week) = medical guidance + dose adjustment; (3) Withdrawal anxiety + physical symptoms = monitoring; (4) Comorbid depression/anxiety = worsen, medication adjustment या psychiatric support need। Benzodiazepines = never “cold turkey”। Supervised taper 8–16 weeks necessary। Supervision = phone follow-ups possible lekin initial assessment + taper plan = in-person। Some patients = psychiatric support या CBT benefit withdrawal दौरान।
10. Kya करना चाहिए अगर months–years vertigo medications पर हो?
Answer: (1) Vestibular evaluation schedule करो: Dix-Hallpike (अगर positional), HINTS (अगर constant)। Confirm diagnosis। (2) VRT referral request करो: PT specializing vestibular। Immediately start, even on medication। (3) Medication taper discuss करो doctor से: Use protocol। Benzodiazepines = 10% per week 8–16 weeks। Antihistamines/anticholinergics = faster (1–2 weeks)। (4) Early mobilization शुरू करो: Even on medication, gentle walking, head movements। (5) Rebound expect करो: Medication stop के बाद dizziness may worsen temporarily (24–72 hours)। Normal। (6) Monitor symptoms: New neuro symptoms (weakness, speech, vision) = urgent care। (7) Long-term plan: VRT 8–12 weeks minimum। Most patients = 80–90% improvement supervised taper + VRT।
HINDI FAQs (20 Questions)
1. Kyun vertigo medications actually recovery को prevent करती हैं?
Answer: Vertigo medications = vestibular system को suppress करती हैं (essence में “quiet” करती हैं inner ear + brainstem signals)। Lekin true recovery = “central compensation” process, जहाँ brain दूसरे senses पर rely सीखता है (vision, proprioception) compensate करने के लिए। Suppressants = natural healing process को block करती हैं क्योंकि वो brain के signals को हटा देती हैं जो brain को adapt करने चाहिए। Short-term (24–72 hours) = suppressants अच्छा लगता है (nausea कम)। Long-term (weeks–months) = dizziness PROLONG होती है क्योंकि central compensation नहीं हो पाता।
2. 72-hour rule absolute है या longer use हो सकता है?
Answer: 72-hour rule = guideline, absolute नहीं। Most cases में suppressants को discontinue होनी चाहिए 72 hours में क्योंकि beyond = recovery को delay करता है more than help। Rare exceptions: (1) Severe Menière’s persistent vomiting—1–2 weeks medication अगर fluids keep नहीं रख सकता; (2) Hospitalized acute vestibular neuritis—acute phase के दौरान medication; (3) Uncontrolled migraine severe vertigo—migraine-specific meds (NOT suppressants) may needed। Key = अगर patient suppressants पर है 72 hours से बिना diagnosis या concurrent VRT के = likely TRAP में है।
3. Kyun patients को medication stop करने से severe dizziness होता है?
Answer: यह “rebound dizziness” कहलाती है = sign कि brain recovering है, NOT disease recurrence। Suppressants active जब brain chemically quiet होता है। Stop करने पर brain suddenly “awake” होता है। Re-emergence of vestibular signals + brain recalibration = temporary severe dizziness, usually 24–72 hours। Temporary, self-limited। Many patients misunderstand करते हैं rebound को disease recurrence के रूप में और medication फिर से resume करते हैं, trap को deepen करते। Patient education critical है।
4. BPPV को medication से treat हो सकता है?
Answer: Nahi। BPPV = mechanical problem (calcium crystals wrong place में)। No medication crystals को correct location पर move नहीं कर सकती। Suppressants = nausea को slightly कम करते हैं लेकिन BPPV को cure नहीं करता और crystals को naturally reposition नहीं करता। Only effective treatment = physical maneuver: Epley या Semont, 80–90% cure rate single session में। BPPV wala patient को = Dix-Hallpike testing + immediate Epley के लिए refer होना चाहिए, NOT suppressants। अगर patient suppressants पर है BPPV के लिए बिना Dix-Hallpike या Epley के = treatment approach को change करनी चाहिए।
5. Kyun benzodiazepines elderly के लिए इतने dangerous हैं?
Answer: Benzodiazepines significantly increase करते हैं fall risk, cognitive decline, mortality elderly patients में (65+)। Mechanism multifaceted: (1) Sedation + cognitive impairment = balance + reaction time को reduce करता है; (2) Elderly = natural decline vestibular, visual, proprioceptive में; benzodiazepines के साथ = “perfect storm”; (3) 50–80% fall risk increase elderly में, falls = leading cause death age group में; (4) Long-term = dementia-like cognitive decline + depression। Elderly + vestibular disorders के लिए benzodiazepines को avoid करनी चाहिए अगर possible हो। अगर absolutely necessary severe acute के लिए = 48 hours से ज्यादा नहीं। Non-pharmacological (VRT, mobilization) = far safer + effective।
6. Kya meclizine long-term use के लिए safe है?
Answer: Nahi। Meclizine को अक्सर “safer” prescribe किया जाता है benzodiazepines के मुकाबले, लेकिन NOT appropriate long-term के लिए। Long-term meclizine = persistent sedation + brain fog; dry mouth, blurred vision, constipation; tolerance (higher doses needed); delayed central compensation (brain की natural healing block)। Clinical studies = patients on meclizine 1–2 weeks से ज्यादा prolonged dizziness दिखाते हैं compared early VRT बिना medication के। Meclizine appropriate = 24–48 hours acute attack, फिर taper। अगर patient weeks–months meclizine पर है = discontinued होनी चाहिए + VRT initiate।
7. Anticholinergic toxicity क्या है aur kyun dangerous?
Answer: Anticholinergic drugs (scopolamine, atropine, some antihistamines) = acetylcholine को block करती हैं brain + body में, distinctive syndrome = “anticholinergic toxicity”। Symptoms = confusion, delirium, agitation, hallucinations, urinary retention, dry mouth, blurred vision, constipation, increased heart rate। Elderly = extremely vulnerable। Anticholinergic burden = multiple anticholinergic meds accumulation = associated dementia risk + falls। Scopolamine patches = very effective motion sickness के लिए लेकिन problematic chronic use क्योंकि continuous anticholinergic effects 72 hours per patch देता है। Scopolamine = केवल travel motion sickness (brief duration), never chronic vertigo।
8. Rebound dizziness aur disease worsening में क्या difference?
Answer: Rebound dizziness (good sign): Occurs 24 hours के अंदर discontinuation के; temporary (24–72 hours); worsens फिर improves; functional; no new neuro symptoms। Brain waking up।
Disease worsening (bad sign): Progressive days–weeks; persists 72 hours से ज्यादा; new symptoms (weakness, speech, vision loss); progressively less functional। Requires urgent imaging।
Key: अगर dizziness worsens immediately after stopping medication लेकिन improves 72 hours में = rebound। अगर days बाद progressively worsens = may be disease, requires evaluation।
9. Kya benzodiazepine taper घर पे safely हो सकता है बिना medical supervision?
Answer: Nahi। Benzodiazepine tapering = medical supervision required। कारण: (1) Abrupt discontinuation = seizures possible; (2) Slow tapering (10% per week) = medical guidance + dose adjustment; (3) Withdrawal anxiety + physical symptoms = monitoring; (4) Comorbid depression/anxiety = worsen, medication adjustment या psychiatric support need। Benzodiazepines = never “cold turkey”। Supervised taper 8–16 weeks necessary। Supervision = phone follow-ups possible लेकिन initial assessment + taper plan = in-person। Some patients = psychiatric support या CBT से benefit withdrawal के दौरान।
10. Kya करना चाहिए अगर months–years vertigo medications पर हो?
Answer: (1) Vestibular evaluation schedule करो: Dix-Hallpike (अगर positional), HINTS (अगर constant)। Confirm diagnosis। (2) VRT referral request करो: PT specializing in vestibular। Immediately start, even on medication। (3) Medication taper discuss करो doctor से: Use protocol। Benzodiazepines = 10% per week 8–16 weeks। Antihistamines/anticholinergics = faster (1–2 weeks)। (4) Early mobilization शुरू करो: Even on medication, gentle walking, head movements। (5) Rebound expect करो: Medication stop के बाद dizziness may worsen temporarily (24–72 hours)। Normal। (6) Monitor symptoms: New neuro symptoms (weakness, speech, vision) = urgent care। (7) Long-term plan: VRT 8–12 weeks minimum। Most patients = 80–90% improvement supervised taper + VRT।
📞 PRIME ENT CENTER CONTACT INFORMATION
Dr. Prateek Porwal, MBBS, DNB, CAMVD (Yenepoya)
Senior ENT Specialist | Vestibular Disorders & Neuro-Otology
University Certified Neurotologist (India)
11 Years of Clinical Experience
PRIME ENT Center
Clinic Location:
Nagheta Road, Near Income Tax Office
Jindpeer Chauraha, Hardoi
Uttar Pradesh 241001, India
Contact Details:
- Phone: +91 73930 62200
- Email: primeenthdi@gmail.com
- Website: https://primeentcenter.in
Consultation Timings:
- Monday to Saturday: 11:00 AM–04:00 PM | 06:00 PM–08:00 PM
- Sunday: Closed
- Emergency Services: Available through main contact number
Why Choose PRIME ENT Center for Medication Safety & Vertigo Management?
✓ Evidence-Based Medication Tapering – Safe discontinuation protocols for antihistamines, benzodiazepines, anticholinergics
✓ Vestibular Rehabilitation Coordination – Direct referral to specialized PT for VRT during medication transitions
✓ Comprehensive Diagnostic Evaluation – Dix-Hallpike, HINTS exam, vestibular testing to confirm accurate diagnosis before medication decisions
✓ Medication Safety Expertise – Awareness of drug interactions, elderly-specific contraindications, addiction risks
✓ Patient Education – Detailed explanations of medication traps, rebound effects, safe alternatives
✓ 3-Language Care – English, Hindi, Hinglish patient counseling and taper protocol guidance
✓ Telehealth Monitoring – Remote follow-ups during medication taper phases
✓ Crisis Prevention – Early identification of patients stuck in medication cycles, rapid intervention
Book Your Consultation Today
For medication review, safe tapering guidance, or comprehensive vestibular evaluation:
📱 Call: +91 73930 62200
💬 WhatsApp: +91 73930 62200
📧 Email: primeenthdi@gmail.com
🌐 Website: https://primeentcenter.in
What to Bring to Your Medication Review Appointment
- Complete medication list: All current medications, dosages, duration of use (especially “dizziness pills”)
- Medical records: Previous diagnoses, prior imaging results, past vestibular evaluations
- Symptom diary or timeline: When symptoms started, how medication affected them over time
- Questions about tapering: Concerns about rebound, withdrawal, how to stop safely
- Insurance information: For VRT referral coordination
About Dr. Prateek Porwal
Dr. Prateek Porwal is a highly experienced, board-certified ENT specialist with advanced training in vestibular disorders, medication safety, and evidence-based vertigo management. With over 11 years of dedicated clinical practice, Dr. Porwal has helped hundreds of patients escape the medication trap through safe tapering, accurate diagnosis, and early VRT initiation.
Key Qualifications:
- MBBS – Bachelor of Medicine, Bachelor of Surgery
- DNB – Diplomate of National Board, ENT
- CAMVD (Yenepoya), University Certified Neurotologist (India) – Specialized certification in vestibular neurology and medication effects on inner ear
Dr. Porwal understands the complexity of long-term medication use in vertigo management and provides compassionate, evidence-based alternatives that prioritize patient safety and true recovery.
Stop taking pills that prevent recovery. Get evaluated. Get the right diagnosis. Taper safely.
Further Resources on Vestibular Health & Medication Safety Recover truly.
American Vestibular Society – Vestibular Disorder Information
Vestibular Disorders Association (VEDA) – Patient Education & Support
PubMed Central – Peer-reviewed Research on Vestibular Medications
American Academy of Neurology – Vertigo & Dizziness Guidelines
National Institutes of Health – Vestibular Science Research
