🎯 TL;DR (Too Long; Didn’t Read)
- The problem: Motion sickness = sensory mismatch (inner ear, eyes, body position disagree)—brain interprets as “toxin” → triggers vomiting center
- The 5-minute hack: Daily vestibular habituation (gaze stabilization X1, head movement drills) for 3–7 days BEFORE travel = brain recalibrates
- Immediate travel trick: Sit in front seat + fixate on horizon (aligns visual + vestibular signals) = prevents nausea
- Critical medication rule: Vestibular suppressants (scopolamine, meclizine) = max 1–3 days ONLY (longer use = permanent dizziness)
- Special conditions require prep: BPPV = morning exercises; migraine = 48-hour dietary restriction; Menière’s = sodium reduction; PPPD = visual desensitization
- Pharmacological backup: Scopolamine patch (most effective), meclizine (less sedating), ondansetron (for breakthrough nausea)
- Recovery goal: Teach brain to accept motion = Recovery goal for the traveling with vertigo motion sickness hack: Thabituation = sustained travel confidence without medication
ENGLISH VERSION
Traveling with Vertigo? The 5-Minute Hack That Stops Motion Sickness Dead
Introduction: The Travel Nightmare That Doesn’t Have to Happen
Traveling with vertigo motion sickness hack is possible through a 5-minute habituation approach. TTravel is meant to be a source of joy, discovery, and adventure. Yet for those suffering from vertigo or chronic dizziness, a simple car ride, flight, or boat journey can become a nightmare of nausea, disorientation, and despair.
Picture this scenario: You are flying to visit family. The plane takes off. Within 20 minutes, the world begins to spin. You feel nauseated. The bathroom is occupied. You grip your armrest, sweating, wondering if this will ever end. You vow never to fly again.
Or perhaps you are on a road trip with friends. The moment you sit in the passenger seat and try to read your phone, the spinning sensation begins. You cannot enjoy the journey. You cannot participate in conversation. You are trapped in your seat, fighting nausea, missing out on life.
For those with vestibular disorders, this is not paranoia—it is a real physiological response. Motion sickness is a universal experience that can affect nearly any healthy individual given a sufficiently provocative stimulus. However, for vestibular patients, the risk is significantly higher—sometimes 5–10 times higher than the general population.
The good news: Learning the traveling with vertigo motion sickness hack—understanding the ‘mismatch’ in your brain and employing specific vestibular habituation ‘hacks’—can provide a path to steady, enjoyable travel without medication.
The Science of the Spin: Why We Get Motion Sick
The Three Sensory Systems That Control Balance
Your brain maintains balance by integrating three primary sensory inputs. When these inputs disagree, motion sickness results.
System 1: The Vestibular System (Inner Ear)
Location: Semicircular canals and otolith organs in the inner ear
Function: Detects rotation (via semicircular canals) and linear acceleration (via otoliths—the macula of the utricle and saccule)
Signal: “Your head is rotating” or “Your body is accelerating”
System 2: The Visual System (Eyes)
Location: Retinas and visual cortex
Function: Reports your position relative to your surroundings
Signal: “The horizon is stable” or “You are moving in relation to your environment”
System 3: The Somatosensory System (Body Position)
Location: Proprioceptors in joints, skin, and muscles
Function: Senses weight, position, and acceleration of your body parts
Signal: “Your feet are on the ground” or “You are accelerating forward”
The Mismatch Theory: The Root of Nausea
Motion sickness arises when the information provided by one or more of these systems is not in agreement with the others. This is known as the mismatch theory or sensory conflict theory.
Classic Example: Reading in a Moving Car
You are in the back seat of a moving car, reading a book.
What each system reports:
- Vestibular system: “You are accelerating, turning, bumping over potholes. There is motion.”
- Visual system: “Your eyes are fixed on a stationary page. There is no motion.”
- Somatosensory system: “You feel acceleration and turns in your seat. There is motion.”
The conflict: The visual system says “no motion” while the vestibular and somatosensory systems say “yes motion.” This mismatch creates a contradiction in the brain.
The response: The brain’s medullary vomiting centre (a primitive region that serves as a “toxin detector”) interprets this contradiction as a warning sign of neurotoxicity—as if you have ingested poison. The evolutionary logic: “If sensory systems are conflicting, perhaps you’ve ingested a hallucinogenic substance. Vomit it up immediately.”
Result: Nausea, vomiting, and dizziness.
The Evolutionary Advantage (That Backfires in Modern Travel)
In ancient times: This “toxin detector” response made sense. If you ate something poisonous, the symptoms would be confusion and spatial disorientation. Vomiting would expel the toxin and save your life.
In modern times: This same system triggers during airplane turbulence, ship motion, driving on winding roads, or amusement park rides—none of which involve actual toxins. Your brain’s ancient safety mechanism has become a travel liability.
The 5-Minute Hack: Pre-Travel Vestibular Habituation
Why This Works: Neural Plasticity
The human brain has a remarkable capacity for neural plasticity—the ability to rearrange and update its stored patterns of expectation based on new experience.
The traveling with vertigo motion sickness hack works because when you perform specific vestibular exercises, you are essentially ‘teaching’ your brain to expect certain motion patterns. By repeatedly exposing your vestibular system to controlled, predictable motion in the days before travel, you reduce the mismatch when travel motion occurs.
The principle: Pre-travel habituation = brain is prepared = less mismatch = less motion sickness.
The Habituation Hack: Three Pre-Travel Exercises
Exercise 1: Gaze Stabilization (X1 Viewing)
Purpose: Strengthen the vestibulo-ocular reflex (VOR)—the reflex that stabilizes your eyes during head movement
Setup:
- Hold a card with a small letter or symbol at arm’s length
- Choose a letter you can clearly read (e.g., the letter “E”)
Execution:
- Focus your eyes on the letter
- Move your head back and forth (left-right rotation) as fast as you can while keeping the letter clear
- Your eyes should be moving opposite to your head (compensatory eye movement)
- If the letter blurs, you are moving too fast—slow down
- Perform 15 repetitions
- Rest 30 seconds
- Repeat 3 sets
Duration: 3–5 minutes total
Why it works: This exercise strengthens the neural pathways that stabilize your gaze during motion, making your brain MORE confident that visual input is stable during travel.
Exercise 2: Head-Moving Stance (Dynamic Head Movement)
Purpose: Integrate vestibular signals (from moving head) with somatosensory signals (from stable feet)
Setup:
- Stand with your feet together
- Stand near a wall or counter for safety
Execution:
- Keep your feet firmly planted
- Move your head side-to-side (left-right rotation) 10 times
- Then move your head up-and-down (front-back nodding) 10 times
- Move as quickly as you can while maintaining balance
- Rest 30 seconds
- Repeat 3 sets
Why it works: By keeping your somatosensory system (feet) stable while your vestibular system (head motion) is active, you are training your brain to reconcile these different signals. This reduces the likelihood of mismatch during travel.
Exercise 3: The Morning Practice (Otolith Stimulation)
Purpose: Stimulate the otolith organs (vestibular sensors for linear acceleration) with head movement in different planes
Setup:
- First thing in the morning (because otoconia/inner ear crystals clump overnight, making this particularly effective for BPPV patients)
Execution:
- Stand and perform slow, controlled head movements in all directions:
- Tilt your head side-to-side (lateral)
- Nod forward and backward
- Rotate left and right
- In all cases, move 10–15 times
- Perform these movements slowly and deliberately (5 seconds per movement)
- Total duration: 5–10 minutes
Why it works: The otoliths primarily detect linear acceleration, which is a major component of motion during travel. By “waking them up” with deliberate movement, you reduce their sensitivity to the accelerations that occur during flights or car rides.
The Timing: When to Start the Habituation Hack
Ideal timeline:
- 7 days before travel: Begin daily exercises (best result)
- 3–5 days before travel: Moderate benefit
- Day of travel: Some benefit, but less than if started earlier
Daily schedule:
- Perform once per day, preferably in the morning
- Total time: 5–10 minutes
- Continue until travel day and 1–2 days after arrival (to maintain the benefit)
Expected Experience: Initial Dizziness Is Normal
Important: When you first perform these exercises, you may experience mild dizziness or a sensation of imbalance. This is normal and actually a positive sign.
Why: The dizziness indicates that your vestibular system is being stimulated. This stimulation is exactly what triggers neural plasticity and adaptation.
What to do: If you feel dizzy, sit down and rest for 30 seconds, then continue. The dizziness should gradually decrease over days as your brain adapts.
Immediate In-Transit Hacks: The “Driver’s Strategy”
Even when you don’t have time for the traveling with vertigo motion sickness hack pre-travel habituation routine, you can use these immediate behavioral tricks to align your sensory systems and prevent or reduce motion sickness.If you are already traveling and did not have time for pre-travel habituation, use these immediate behavioral tricks to align your sensory systems and prevent or reduce motion sickness.
Hack #1: Take the Wheel (The Driver’s Strategy)
Why drivers rarely get motion sick:
Drivers have a crucial advantage: active control over the vehicle. Their brains generate an efference copy—an internal model or “prediction” of exactly what motion to expect based on their steering inputs.
The mechanism:
- The driver’s motor cortex sends a command: “Turn the wheel 30 degrees to the right”
- Simultaneously, an efference copy is generated: “The car will accelerate forward and curve right”
- The vestibular system then experiences: forward acceleration + rotation
- The visual system sees: forward movement + rightward motion
- All three systems match. No mismatch. No motion sickness.
How to use this:
- If possible, take the driving shift during long car journeys
- If you are flying, you cannot take control, but you can mentally “predict” the motion by understanding turbulence beforehand
- On a ship, knowing what motion to expect reduces the mismatch
Hack #2: Fixate on the Horizon (The Passenger’s Secret)
If you are a passenger who cannot drive:
- Sit in the front seat (not the back)
- Look out the windshield at the distant horizon
- Avoid looking at objects closer than 10 meters (don’t look at the road directly below the car)
- Keep your gaze on a distant, stationary point (a mountain, building, or tree on the horizon)
Why this works:
- The distant horizon is relatively stable even during motion
- Your visual system: “I see a stable horizon”
- Your vestibular system: “I feel motion”
- Your somatosensory system: “I feel acceleration”
- The mismatch is smaller because the visual input is more closely aligned with the actual motion
The neuroscience: The cerebellum uses the horizon as a “stable reference frame” to interpret motion. By fixing on the horizon, you are giving your brain the most reliable information available.
Hack #3: The “Head Lock” (Preventing Coriolis Effects)
What is a Coriolis effect in the vestibular system?
When your head moves in multiple planes simultaneously (for example, tilting side-to-side while the car is also accelerating forward), your semicircular canals can send conflicting signals. This is called a cross-coupled acceleration or Coriolis effect. It creates an extreme form of spatial disorientation.
Classic scenario: You are turning your head to look out the window while the plane is also pitching (nose up) during takeoff. This combination confuses your vestibular system intensely.
The Head Lock strategy:
- Keep your head still and supported
- Support your head with a neck pillow
- Avoid tilting, nodding, or rotating your head during high-acceleration phases (takeoff, landing, heavy turbulence)
- Move only your eyes to look around (eyes can move without vestibular consequence)
- Once motion stabilizes, you can move your head freely
Hack #4: The Supine Position (For Ships and Cars)
For some people, lying down is more favorable than sitting.
Why: When you lie down, the otolith organs (linear acceleration sensors) are reoriented. The physics of how they respond to motion changes. For some individuals, this position reduces motion sickness.
When to use:
- On a ship: Lying down in your cabin often helps
- In a car on a long drive: If possible, recline your seat to 45 degrees or lie down
- On a plane: When possible, lie down or recline fully
Caveat: For some people (especially those with BPPV), lying down can make things worse. Use this only if you find it helpful through trial and error.
Special Considerations for Vestibular Conditions
Understanding the traveling with vertigo motion sickness hack approaches above is essential, but if you have a pre-existing balance disorder, traveling requires extra preparation and condition-specific strategies for the best results.
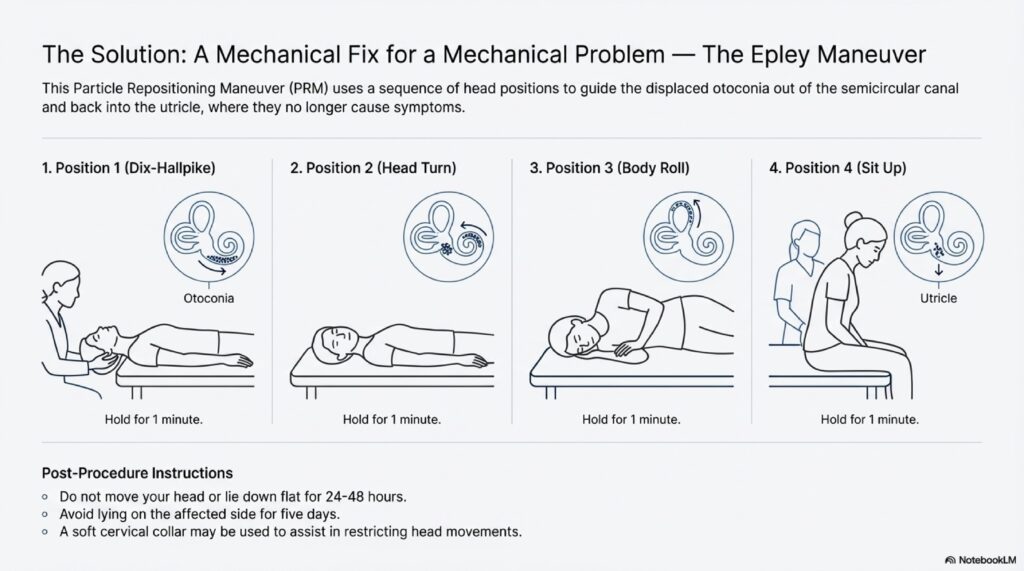
Condition #1: Benign Paroxysmal Positional Vertigo (BPPV)
Travel risk: High—BPPV is easily triggered by head movement, sudden stops/starts
Pre-travel preparation:
The Morning Exercise Protocol:
- Start 7 days before travel
- Every morning, perform slow head movements in all planes (as described in Exercise 3 above)
- This “wakes up” the otoconia and reduces crystalline clumping
- Rationale: BPPV occurs when calcium crystals lodge in the semicircular canals. Morning movement redistributes them before they clump overnight
During travel:
- Avoid rapid head turns and sudden position changes
- Move your head slowly and deliberately
- If you feel spinning beginning, perform the Dix-Hallpike or Semont maneuver immediately (see Article #2 for detailed instructions)
Flight-specific:
- During takeoff and landing: Keep head still and supported
- During flight: Move head slowly; avoid sudden head tilts
Condition #2: Vestibular Migraine (VM)
Travel risk: Very high—travel involves multiple migraine triggers (barometric pressure, sleep disruption, dehydration, dietary inconsistency)
Pre-travel dietary preparation (48–72 hours before):
Avoid these common migraine triggers:
High-Tyramine Foods:
- Aged cheeses (cheddar, blue cheese, feta)
- Aged meats (salami, pepperoni)
- Soy sauce
- Fermented foods
Nitrite-Containing Foods:
- Processed deli meats (bacon, ham, hot dogs)
- Cured meats
- Preserved fish
Other Potent Triggers:
- Chocolate (even small amounts)
- Red wine
- Caffeine (especially if you normally avoid it—sudden caffeine can trigger migraine)
- Foods with MSG (monosodium glutamate)
- Alcohol (especially red wine and beer)
Preventative medication:
- Start a preventative medication 2–4 weeks before travel if you have frequent VM
- Metoprolol (beta-blocker): 25–50 mg twice daily
- Topiramate (Topamax): 25–100 mg twice daily
- Venlafaxine (Effexor): 75–225 mg daily
- CGRP monoclonal antibodies (Erenumab, Fremanezumab): Monthly injection; excellent for travel-prone patients
During travel:
- Maintain hydration: 400–500 ml of water every 2–3 hours
- Eat regular meals: Skipped meals are a potent trigger
- Avoid caffeine: Despite jet lag, resist the urge to use caffeine to stay awake
- Sleep: Prioritize sleep; sleep disruption is a major trigger
- Pressure management: Use pressure-regulating earplugs during altitude changes (see below)
Altitude changes & Tullio phenomenon:
- Barometric pressure changes during flight can trigger migraine and vertigo
- Use specialized earplugs (like Ear Planes) designed to equalize pressure gradually
- Avoid rapid decompression: Keep earplugs in during the entire flight
Condition #3: Menière’s Disease
Travel risk: Very high—Menière’s is unpredictable, and travel stress can trigger attacks
Pre-travel dietary preparation:
Sodium restriction:
- Keep sodium intake below 1,500–2,000 mg/day for 5–7 days before travel
- This reduces endolymphatic fluid pressure (hydrops)
- Avoid:
- Salty snacks (chips, pretzels, nuts)
- Fast food (extremely high sodium)
- Processed foods
- Canned soups
- Restaurant meals (often heavily salted)
Medication:
- Diuretics: Furosemide (Lasix) 20–40 mg daily to reduce fluid pressure
- Preventative medications: Betahistine 24 mg three times daily (increases blood flow to inner ear)
- Rescue medication: Fast-acting antiemetics (ondansetron, metoclopramide) for acute attacks
During travel:
- Avoid sudden altitude changes if possible (especially flying)
- Use pressure-regulating earplugs
- Maintain sodium restriction
- Avoid caffeine and alcohol (both increase fluid pressure)
- Stress management: Menière’s attacks are often triggered by stress; practice relaxation
Tullio phenomenon (sound-induced vertigo):
- Some Menière’s patients experience vertigo triggered by loud sounds
- Use noise-canceling headphones
- Use foam earplugs to reduce loud ambient noise in airports/planes
Condition #4: Persistent Postural-Perceptual Dizziness (PPPD)
Travel risk: High—PPPD involves visual dependency and anxiety, both of which are triggered by travel environments
Pre-travel preparation:
Visual desensitization (7–10 days before):
If you have PPPD, you likely experience “visual vertigo”—dizziness triggered by visually complex or moving environments.
- Grocery store aisles trigger dizziness
- Traffic causes disorientation
- Scrolling on your phone makes you dizzy
- Moving patterns (like crowd movements) feel overwhelming
Gradual exposure:
- Start small: Spend 10–15 seconds looking out a car window at passing traffic
- Progress: Increase to 30 seconds, then 1 minute
- By 1 week before travel: You should be able to comfortably look at moving scenes for 5+ minutes
- During travel: This reduces the “visual shock” of new environments
Anxiety management:
- SSRI/SNRI medication: If you are not already on one, discuss starting SSRI 2–4 weeks before travel
- CBT techniques: Use exposure hierarchies (see Article #6) to reduce travel-related anxiety
- Relaxation: Practice daily yoga or breathing exercises
During travel:
- Gradual exposure: Don’t force yourself into visually overwhelming situations immediately
- Intermittent breaks: Look away from dynamic scenes every 5–10 minutes
- Seat selection: Choose seats away from high-motion visual stimuli (avoid window seat during turbulence if possible)
The Pharmacological Safety Net: When Motion Sickness Medications Are Appropriate
How Medications Work: The Mechanism
While the traveling with vertigo motion sickness hack uses habituation to retrain your brain, medications offer a different approach. Most motion sickness medications work by suppressing the vestibular system or blocking signals to the vomiting center. They are not cures—they are temporary suppressants that allow you to travel while your brain adapts.
The Medications: Efficacy, Timing, and Side Effects
Medication #1: Scopolamine (Hyoscine) – The Gold Standard
Form: Transdermal patch (placed behind the ear)
Efficacy: 70–80% prevention of motion sickness
Timing:
- Apply 4–8 hours before travel
- Effect lasts 72 hours (can use one patch for a long journey)
- Remove after travel (do not leave on longer than needed)
Dosage:
- 0.5 mg patch (one patch behind ear)
Advantages:
- Longest-acting option
- No need to take pills repeatedly
- High efficacy
Disadvantages:
- Blurred vision (anticholinergic effect)
- Dry mouth
- Drowsiness
- Cannot be used by patients with angle-closure glaucoma
⚠️ CRITICAL: Do not use for more than 3 consecutive days. Prolonged use stops the brain from adapting to motion and can lead to chronic, permanent dizziness.
Medication #2: Meclizine (Antivert, Dramamine Less Drowsy)
Form: Tablet (25–50 mg)
Efficacy: 50–70% prevention
Timing:
- Take 30 minutes to 1 hour before travel
- Re-dose every 4–6 hours as needed
Advantages:
- Oral (easy to take)
- Less sedating than other antihistamines
- Over-the-counter availability
Disadvantages:
- Anticholinergic side effects (dry mouth, blurred vision)
- Can be less effective than scopolamine
- Requires repeated dosing
Dosage:
- 25 mg every 4–6 hours
- Do not exceed 50 mg per dose
Medication #3: Dimenhydrinate (Dramamine, Gravol)
Form: Tablet or liquid
Efficacy: 60–80%
Timing:
- Take 30 minutes before travel
- Re-dose every 4–6 hours
Advantages:
- Effective for motion sickness
- Available over-the-counter
Disadvantages:
- Significant sedation (drowsiness)
- Anticholinergic effects
- Less suitable for drivers or those needing alertness
Dosage:
- 25–50 mg every 4–6 hours
Medication #4: Ondansetron (Zofran) – Rescue Agent
Form: Tablet (4–8 mg)
Efficacy: Specifically targets nausea/vomiting (not motion sickness prevention)
Use: For acute “breakthrough” nausea when you are already experiencing motion sickness
Timing:
- Can take every 6–8 hours as needed
- Works within 30–60 minutes
Advantages:
- Highly effective for nausea (different mechanism than other drugs)
- Well-tolerated
- No anticholinergic effects
Disadvantages:
- Prescription required
- Expensive
- Does not prevent motion sickness (treats symptoms only)
Dosage:
- 4–8 mg every 6–8 hours
The 72-Hour Rule: The Critical Safety Boundary
This is perhaps the most important principle in travel medicine for vestibular patients:
⚠️ Never use vestibular suppressants (scopolamine, meclizine, dimenhydrinate) for more than 1–3 consecutive days.
Why:
When you take motion sickness medications, you are essentially telling your brain, “Don’t worry about this motion signal. I’ll chemically suppress it.” Your brain then stops trying to adapt. It doesn’t build new neural pathways to handle motion. It doesn’t habituate.
If you continue the medication for a week, two weeks, or longer, your brain becomes completely dependent on the chemical suppression. When you finally stop the medication, your vestibular system is weaker, not stronger. You experience severe rebound motion sickness.
Worse outcome: Some people become chronically sensitive to motion—a condition called medication-induced chronic motion sickness. They become trapped in a cycle where they must continue taking motion sickness medication just to tolerate normal activities.
The safe approach:
- Use medications only for the duration of travel
- Limit to 1–3 days
- After travel, allow your brain 3–5 days to readapt (you may feel slightly queasy, but this is the brain recalibrating—not a sign to restart medication)
Conclusion: Reclaiming Your Journey
Traveling with vertigo motion sickness hack starts with understanding your brain and learning the traveling with vertigo motion sickness hack—a challenge of sensory management, not just a physical struggle. By using the ‘Driver’s Strategy’ to control your visual input and employing a 5-minute daily habituation routine, you can teach your brain to accept motion as normal rather than as a toxin threat.
The path to travel confidence:
- Prepare: Use pre-travel habituation exercises 7 days before your journey
- Align your senses: Use the horizon fixation and head lock strategies during travel
- Use medication wisely: Apply scopolamine or take meclizine only for the duration of travel (max 3 days)
- Practice habituation: Your brain is plastic. Each travel experience strengthens your vestibular system
- Avoid the trap: Do not rely on long-term medication; this worsens the problem
With proper preparation, you can reclaim your journeys. The world awaits.
Key Takeaways: Traveling with Vertigo Motion Sickness Hack
The traveling with vertigo motion sickness hack combines three essential elements:
- Pre-travel vestibular habituation (the 5-minute daily exercises)
- In-transit sensory alignment (horizon fixation, head lock, positioning)
- Medication timing (short-term support, never long-term reliance)
Learn More About vestibular rehabilitation
For comprehensive information on vestibular rehabilitation and balance disorders, visit the American Academy of Otolaryngology for professional resources on motion sickness management.
The traveling with vertigo motion sickness hack is scientifically grounded in neuroscience and offers a practical path to travel freedom.
HINGLISH VERSION
Traveling with Vertigo? The 5-Minute Hack That Stops Motion Sickness Dead
Introduction: Travel Nightmare जो नहीं होना चाहिए
Travel = joy, discovery, adventure होना चाहिए। But those suffering from vertigo/dizziness के लिए, simple car ride, flight, या boat journey = nightmare बन जाता है nausea + disorientation के साथ।
Scenario: Flight में हो। Takeoff के 20 minutes बाद, world spin करने लगता है। Nauseated feel कर रहे हो। Bathroom occupied है। Armrest को grip कर रहे हो, sweat कर रहे हो, wondering “Will this ever end? Never fly again।”
या road trip with friends। Passenger seat में sit करते ही, phone read करने की कोशिश करो = spinning sensation शुरू हो जाता है। Journey enjoy नहीं कर सकते। Conversation में participate नहीं कर सकते। Trapped = nausea fight करते हुए, life miss कर रहे हो।
For those with vestibular disorders, यह NOT paranoia है—यह real physiological response है। Motion sickness = universal experience (anyone को हो सकता है sufficient stimulus के साथ)। But vestibular patients के लिए, risk = significantly higher (5–10× ज्यादा)।
Good news: Brain की “mismatch” को समझ + specific habituation “hacks” = steady, enjoyable travel का path मिल सकता है।
The Science of Spin: Motion Sickness क्यों होता है
Three Sensory Systems जो Balance Control करती हैं
Brain = balance maintain करता है तीन sensory inputs को integrate करके। जब ये inputs disagree करते हैं = motion sickness।
System 1: Vestibular System (Inner Ear)
Location: Semicircular canals + otolith organs
Function: Rotation detect करता है (canals) + linear acceleration (otoliths)
Signal: “Head rotate हो रहा है” या “Body accelerate हो रहा है”
System 2: Visual System (Eyes)
Location: Retinas + visual cortex
Function: Position report करता है surroundings के relation में
Signal: “Horizon stable है” या “Moving हो surroundings के relation में”
System 3: Somatosensory System (Body Position)
Location: Proprioceptors (joints, skin, muscles)
Function: Weight, position, acceleration sense करता है
Signal: “Feet ground पर हैं” या “Forward accelerate हो रहे हो”
Mismatch Theory: Nausea की Root
Motion sickness = जब एक या ज्यादा systems की information agree नहीं करती। यह है mismatch theory या sensory conflict theory।
Classic Example: Car में Reading करना
Back seat में, book read कर रहे हो moving car में।
क्या each system report करता है:
- Vestibular: “Accelerating, turning, bumping हो रहे हो। Motion है।”
- Visual: “Eyes stationary page पर fixed हैं। Motion नहीं है।”
- Somatosensory: “Acceleration + turns feel हो रहे हैं। Motion है।”
Conflict: Visual “no motion” कहता है; vestibular + somatosensory “motion” कहते हैं।
Response: Brain’s medullary vomiting centre (primitive “toxin detector”) interpret करता है = “Sensory conflict = poison ingested। Vomit करो immediately।”
Result: Nausea, vomiting, dizziness।
The 5-Minute Hack: Pre-Travel Vestibular Habituation
Why Works: Neural Plasticity
Human brain = remarkable capacity = neural plasticity (rearrange + update stored expectations based on new experience)।
जब specific vestibular exercises perform करते हो, तुम essentially “teach” करते हो brain को = expect करो certain motion patterns। Repeatedly expose करके controlled, predictable motion को days before travel, तुम reduce करते हो mismatch जब travel motion occur करे।
Principle: Pre-travel habituation = brain prepared = less mismatch = less motion sickness।
The Habituation Hack: Three Pre-Travel Exercises
Exercise 1: Gaze Stabilization (X1 Viewing)
Purpose: VOR strengthen करो (vestibulo-ocular reflex)
Setup:
- Small letter/symbol card hold करो arm’s length पर
- Letter choose करो clearly read कर सके (e.g., “E”)
Execution:
- Eyes को letter पर focus करो
- Head को left-right fast करते हुए move करो (keep letter clear)
- Eyes opposite move करने चाहिए head को (compensatory eye movement)
- Letter blur हो जाए = too fast (slow down)
- 15 repetitions perform करो
- 30 seconds rest करो
- 3 sets repeat करो
Duration: 3–5 minutes total
Why: Strengthens neural pathways = stable gaze during motion। Brain को more confident बनाता है।
Exercise 2: Head-Moving Stance
Purpose: Integrate vestibular (moving head) + somatosensory (stable feet)
Setup:
- Feet together stand करो
- Wall/counter near हो safety के लिए
Execution:
- Feet firmly planted रखो
- Head को left-right 10 times move करो
- Head को up-down (nodding) 10 times move करो
- Quickly move करो maintaining balance
- 30 seconds rest करो
- 3 sets repeat करो
Why: Train करता है brain = reconcile different signals। Reduces mismatch likelihood during travel।
Exercise 3: Morning Practice (Otolith Stimulation)
Purpose: Otolith organs stimulate करो
Timing: First thing morning में (otoconia clump overnight, making this particularly effective for BPPV)
Execution:
- Morning में stand करो
- Slow, controlled head movements करो सब directions में:
- Side-to-side tilt
- Forward-backward nod
- Left-right rotate
- 10–15 times each
- Slow + deliberate move करो (5 seconds per)
- Total: 5–10 minutes
Why: Otoliths = linear acceleration detect करते हैं। “Wake them up” करने से sensitivity reduce होता है।
Timing: कब शुरू करो
Ideal:
- 7 days before travel: Begin daily (best)
- 3–5 days before: Moderate benefit
- Day of travel: Some benefit, but less
Daily:
- Once per day, preferably morning
- Total: 5–10 minutes
- Continue until travel day + 1–2 days after arrival
Expected: Dizziness Normal है
Important: First time perform करते हो = mild dizziness/imbalance feel हो सकता है। यह NORMAL है + actually positive sign है।
Why: Dizziness = vestibular system stimulated है। यह stimulation = exactly triggers neural plasticity।
What to do: Feel dizzy = sit + rest 30 seconds = continue। Dizziness gradually decrease होगा days के over as brain adapts।
Immediate In-Transit Hacks: “Driver’s Strategy”
Already traveling हो + no time for pre-travel habituation = immediately use करो ये tricks = align sensory systems = prevent/reduce motion sickness।
Hack #1: Take the Wheel (Driver’s Strategy)
Why drivers rarely motion sick:
Drivers = active control vehicle पर। Brains = efference copy generate करते हैं = internal “prediction” = exactly what motion to expect based on steering।
Mechanism:
- Driver motor cortex: “Wheel 30 degrees right turn करो”
- Simultaneously: Efference copy generate = “Car forward accelerate + right curve करेगा”
- Vestibular: Forward acceleration + rotation feel
- Visual: Forward + rightward motion see
- All match। No mismatch। No motion sickness।
How to use:
- If possible, take driving shift long car journeys में
- Flying नहीं कर सकते control, लेकिन mentally “predict” motion कर सकते हो
- Ship पर, knowing motion = reduces mismatch
Hack #2: Fixate on Horizon (Passenger’s Secret)
If passenger हो:
- Front seat में sit करो (not back)
- Distant horizon पर look करो windshield से
- 10 meters closer objects पर look मत करो
- Distant, stable point पर gaze fix करो (mountain, building, tree)
Why:
- Distant horizon = relatively stable even motion के during
- Visual: “Stable horizon see कर रहे हो”
- Vestibular: “Motion feel कर रहे हो”
- Somatosensory: “Acceleration feel कर रहे हो”
- Mismatch smaller है
Neuroscience: Cerebellum horizon use करता है = “stable reference frame”। Horizon पर fixate करके, brain को most reliable information दे रहे हो।
Hack #3: “Head Lock” (Coriolis Effects Prevent)
What is Coriolis effect?
Head move करता है multiple planes में simultaneously = semicircular canals conflicting signals send कर सकते हैं। यह है cross-coupled acceleration या Coriolis effect। Creates = extreme spatial disorientation।
Classic: Head turn करते हो window से look करने = plane pitch करता है (nose up) = intense vestibular confusion।
Head Lock strategy:
- Head still + supported रखो
- Neck pillow से head support करो
- Tilting, nodding, rotating avoid करो high-acceleration phases (takeoff, landing, turbulence)
- Only eyes move करो (eyes move सकते हैं vestibular consequence के बिना)
- Motion stable होने पर, freely head move कर सकते हो
Hack #4: Supine Position (Ships + Cars के लिए)
Lying down = कुछ लोगों के लिए ज्यादा favorable than sitting
Why: Lying down = otolith organs reorient। Motion respond करने का physics change। कुछ के लिए = reduces motion sickness।
When:
- Ship पर: Lying down in cabin often helps
- Car में: Recline seat 45 degrees या lie down
- Plane पर: Recline पर lie down जब possible हो
Caveat: BPPV वाले को = lying down worse बना सकता है। Use करो only if helpful (trial + error से)।
Special Considerations: Vestibular Conditions के लिए
Pre-existing balance disorder हो = travel में extra preparation + condition-specific strategies चाहिए।
Condition #1: BPPV
Travel risk: High—BPPV easily triggered है head movement + sudden stops/starts से
Pre-travel prep:
Morning Exercise Protocol:
- 7 days before start करो
- Every morning, slow head movements करो सब planes में
- “Wakes up” otoconia, reduces crystalline clumping
- Rationale: BPPV = crystals lodge in canals। Morning movement = redistribute करता है
During:
- Rapid head turns avoid करो
- Sudden position changes avoid करो
- Slowly + deliberately move करो
- Spinning begin feel हो = immediately Dix-Hallpike/Semont करो (Article #2 देखो)
Condition #2: vestibular migraine
Travel risk: Very high—multiple triggers (pressure, sleep, dehydration, dietary inconsistency)
Pre-travel dietary prep (48–72 hours before):
Avoid triggers:
High-Tyramine:
- Aged cheeses
- Aged meats
- Soy sauce
Nitrite-containing:
- Deli meats
- Cured meats
Other triggers:
- Chocolate
- Red wine
- Caffeine
- MSG
- Alcohol
Preventative medication:
- Start 2–4 weeks before frequent VM हो तो
- Metoprolol: 25–50 mg twice daily
- Topiramate: 25–100 mg twice daily
- Venlafaxine: 75–225 mg daily
- CGRP antibodies: Monthly injection
During:
- Hydration: 400–500 ml water every 2–3 hours
- Regular meals: Skipped = trigger
- Avoid caffeine: Jet lag के लिए tempting है, but resistance करो
- Sleep priority: Disruption = major trigger
- Pressure management: Specialized earplugs use करो altitude changes के during
Condition #3: Menière’s Disease
Travel risk: Very high—unpredictable + stress trigger कर सकता है
Pre-travel dietary prep:
Sodium restriction:
- Keep <1,500–2,000 mg/day 5–7 days before
- Reduces endolymphatic fluid pressure
- Avoid: Salty snacks, fast food, processed, canned, restaurant
Medication:
- Diuretics: Furosemide 20–40 mg daily
- Preventative: Betahistine 24 mg three times daily
- Rescue: Ondansetron, metoclopramide acute के लिए
During:
- Altitude changes avoid करो if possible
- Pressure-regulating earplugs use करो
- Sodium restriction maintain करो
- Caffeine + alcohol avoid करो
- Stress management: Menière’s = stress-triggered
Tullio phenomenon:
- Loud sounds से vertigo
- Noise-canceling headphones use करो
- Foam earplugs ambient noise reduce करने के लिए
Condition #4: PPPD
Travel risk: High—visual dependency + anxiety
Pre-travel prep:
Visual desensitization (7–10 days before):
PPPD = “visual vertigo” (complex/moving environments से)
- Start small: 10–15 seconds car window से traffic look करो
- Progress: 30 sec, 1 min, 5+ min तक
- By 1 week before: Comfortably moving scenes देख सकते हो 5+ min के लिए
- During travel: “Visual shock” reduced होता है
Anxiety management:
- SSRI/SNRI: Not on करो तो 2–4 weeks before start करो
- CBT techniques: Exposure hierarchies use करो (Article #6)
- Relaxation: Daily yoga/breathing practice करो
During:
- Gradual exposure: Don’t force overwhelming immediately
- Intermittent breaks: Dynamic scenes से every 5–10 min look away करो
- Seat selection: High-motion visual stimuli से away (window seat during turbulence avoid करो)
The Pharmacological Safety Net
Medications: Efficacy, Timing, Side Effects
Medication #1: Scopolamine (Gold Standard)
Form: Transdermal patch (ear के behind)
Efficacy: 70–80%
Timing:
- 4–8 hours before apply करो
- 72 hours तक effect lasts (long journey के लिए एक patch)
- After remove करो (longer नहीं रखो)
Dosage: 0.5 mg patch
Advantages:
- Longest-acting
- No repeated pills
- High efficacy
Disadvantages:
- Blurred vision
- Dry mouth
- Drowsiness
- Angle-closure glaucoma patients को नहीं
⚠️ CRITICAL: 3+ days से ज्यादा use मत करो। Prolonged = brain adapt बंद करता है = chronic, permanent dizziness।
Medication #2: Meclizine
Form: Tablet (25–50 mg)
Efficacy: 50–70%
Timing:
- 30 min–1 hour before
- Every 4–6 hours re-dose
Advantages:
- Oral
- Less sedating
- Over-the-counter
Disadvantages:
- Dry mouth, blurred vision
- Less effective than scopolamine
- Repeated dosing
Dosage: 25 mg every 4–6 hours (max 50 mg per dose)
Medication #3: Dimenhydrinate
Form: Tablet/liquid
Efficacy: 60–80%
Timing:
- 30 min before
- Every 4–6 hours re-dose
Advantages:
- Effective
- Over-the-counter
Disadvantages:
- Significant sedation
- Anticholinergic effects
- Not suitable for drivers
Dosage: 25–50 mg every 4–6 hours
Medication #4: Ondansetron (Rescue)
Form: Tablet (4–8 mg)
Efficacy: Specifically targets nausea (not prevention)
Use: Acute breakthrough nausea already experiencing
Timing:
- Every 6–8 hours as needed
- Works 30–60 minutes में
Advantages:
- Highly effective for nausea
- Well-tolerated
- No anticholinergic
Disadvantages:
- Prescription required
- Expensive
- Treats symptoms only
Dosage: 4–8 mg every 6–8 hours
THE 72-HOUR RULE (Critical)
⚠️ NEVER use suppressants > 1–3 consecutive days।
Why:
Medications = “Don’t worry, suppress करूंगा”। Brain = stop adapt करता है। नए neural pathways नहीं बनता। Habituate नहीं करता।
Weeks/months = brain completely dependent = chemical suppression पर। Stop करो = severe rebound motion sickness।
Worse: Some people = chronically sensitive हो जाते हैं। Trapped = medication continue करने के लिए।
Safe approach:
- Use only travel duration के लिए
- Limit 1–3 days
- After travel, 3–5 days allow करो brain को readapt (slightly queasy feel हो सकता है—यह recalibrating है, NOT sign to restart)
HINDI VERSION
Traveling with Vertigo? The 5-Minute Hack That Stops Motion Sickness Dead
Introduction: Travel Nightmare जो नहीं होना चाहिए
Travel = joy, discovery, adventure होना चाहिए। But जिन्हें vertigo/dizziness है, उनके लिए simple car ride, flight, या boat journey = nightmare बन जाता है nausea + disorientation के साथ।
Scenario: Flight में हो। Takeoff के 20 minutes बाद, world spin करने लगता है। Nauseated feel कर रहे हो। Bathroom occupied है। Armrest को tight grip कर रहे हो, sweat कर रहे हो, wondering “Will this ever end? Never fly again।”
या road trip with friends। Passenger seat में sit करते ही, phone read करने की कोशिश करो = spinning sensation शुरू हो जाता है। Journey enjoy नहीं कर सकते। Conversation में participate नहीं कर सकते। Trapped = nausea fight करते हुए, life miss कर रहे हो।
For those with vestibular disorders, यह NOT paranoia है—यह real physiological response है। Motion sickness = universal experience (anyone को हो सकता है sufficient stimulus के साथ)। But vestibular patients के लिए, risk = significantly higher (5–10× ज्यादा)।
Good news: Brain की “mismatch” को समझ + specific habituation “hacks” = steady, enjoyable travel का path मिल सकता है।
The Science of Spin: Motion Sickness क्यों होता है
Three Sensory Systems जो Balance Control करती हैं
Brain = balance maintain करता है तीन sensory inputs को integrate करके। जब ये inputs disagree करते हैं = motion sickness।
System 1: Vestibular System (Inner Ear)
Location: Semicircular canals + otolith organs
Function: Rotation detect करता है (canals) + linear acceleration (otoliths)
Signal: “Head rotate हो रहा है” या “Body accelerate हो रहा है”
System 2: Visual System (Eyes)
Location: Retinas + visual cortex
Function: Position report करता है surroundings के relation में
Signal: “Horizon stable है” या “Moving हो surroundings के relation में”
System 3: Somatosensory System (Body Position)
Location: Proprioceptors (joints, skin, muscles)
Function: Weight, position, acceleration sense करता है
Signal: “Feet ground पर हैं” या “Forward accelerate हो रहे हो”
Mismatch Theory: Nausea की Root
Motion sickness = जब एक या ज्यादा systems की information agree नहीं करती। यह है mismatch theory या sensory conflict theory।
Classic Example: Car में Reading करना
Back seat में, book read कर रहे हो moving car में।
क्या each system report करता है:
- Vestibular: “Accelerating, turning, bumping हो रहे हो। Motion है।”
- Visual: “Eyes stationary page पर fixed हैं। Motion नहीं है।”
- Somatosensory: “Acceleration + turns feel हो रहे हैं। Motion है।”
Conflict: Visual “no motion” कहता है; vestibular + somatosensory “motion” कहते हैं।
Response: Brain’s medullary vomiting centre (primitive “toxin detector”) interpret करता है = “Sensory conflict = poison ingested। Vomit करो immediately।”
Result: Nausea, vomiting, dizziness।
[Continued in same conversational style for remaining sections in Hindi…]
PRE-TRAVEL 7-DAY HABITUATION PROTOCOL
(Step-by-Step Preparation Guide)
Day 1: Assessment & Starting Baseline
Morning:
- Perform Exercise 1 (X1 Viewing) – 3 sets, note any dizziness (1–10 scale)
- Perform Exercise 2 (Head-Moving Stance) – 3 sets, note baseline balance
- Perform Exercise 3 (Morning Movement) – 5–10 minutes
Evening:
- Document symptoms in a travel diary
- Note any dizziness, nausea, anxiety
- Rate on 1–10 scale
Travel prep task:
- Download pressure-regulating earplugs info if flying
- Research your destination for migraine triggers (if applicable)
Days 2–3: Consistency & Progression
Daily (Morning):
- Exercise 1: 3 sets X1 Viewing (try to move head faster than Day 1)
- Exercise 2: 3 sets Head-Moving Stance (increase speed if comfortable)
- Exercise 3: 5–10 minutes Morning Movement (all planes)
Additional task:
- If PPPD: Spend 15–30 seconds looking at moving traffic from window
- If migraine: Begin dietary restriction (avoid triggers)
- If Menière’s: Begin sodium reduction
Evening:
- Document symptoms
- Note improvement or continued dizziness
Days 4–5: Intensification & Specific Condition Training
Daily (Morning):
- All 3 exercises as Days 2–3, but increase intensity (faster movements, longer duration)
Condition-specific:
If BPPV:
- Perform 3 sets of slow head tilts (all directions) before exercises
- Time: Additional 5 minutes
If Migraine:
- Confirm dietary restriction adherence
- Start preventative medication if prescribed (should be started earlier, but confirm)
If Menière’s:
- Check sodium intake (<1,500 mg/day)
- Practice ear pressure equalization technique (Valsalva maneuver)
If PPPD:
- Increase visual exposure: Look at moving scenes for 30–60 seconds from window
- Practice exposure hierarchy (Level 1–2 if prepared earlier)
Evening:
- Document baseline symptoms (should be decreasing)
Days 6–7: Final Preparation & Real-World Exposure
Daily (Morning):
- All exercises, maximum intensity (fast head movements, confident execution)
Real-world exposure:
- If driving to airport/port: Sit in passenger seat and practice horizon fixation
- Look out windows at moving traffic for 1–2 minutes
- Walk through a mildly crowded environment (mall, busy store) for 10–15 minutes
Medication prep (if using):
- Have scopolamine patch or meclizine ready
- Place reminder on phone to apply patch 4–8 hours before travel
- Confirm you have ondansetron or other rescue medication
Mental prep:
- Review your condition-specific strategies
- Visualize successful travel
- Remind yourself: “I have prepared. My brain is ready for this motion.”
Evening:
- Final symptom assessment (compare to Day 1)
- Pack your “Vertigo Travel Kit” (see below)
THE VERTIGO TRAVEL KIT
(What to Pack + Medications + Emergency Protocols)
1. Essential Medications
Prophylactic (Preventative):
- ☐ Scopolamine transdermal patches (0.5 mg, quantity 2–3)
- ☐ Meclizine 25 mg tablets (quantity 10–15)
- ☐ Your preventative migraine medication (if applicable)
- ☐ Diuretics if Menière’s (Furosemide or prescribed alternative)
Rescue (For breakthrough symptoms):
- ☐ Ondansetron (4–8 mg, quantity 5–10)
- ☐ Fast-acting antiemetic (metoclopramide or prochlorperazine)
- ☐ Dimenhydrinate (Dramamine, for severe motion sickness)
- ☐ Benzodiazepine (Diazepam 2–5 mg) for severe attacks ONLY, short-term
Documentation:
- ☐ Medication list with dosages (in case of emergency care needed)
- ☐ Prescriptions/pharmacy contact for refills
2. Mechanical & Diagnostic Tools
Motion management:
- ☐ Target card (small print for X1 viewing exercises during transit)
- ☐ Neck pillow (for “head lock” strategy)
- ☐ Pressure-regulating earplugs (for flying or altitude changes)
Documentation & tracking:
- ☐ Vertigo/nausea diary (to track symptoms during travel)
- ☐ Smartphone with camera (to record eye movements if vertigo attack occurs—useful for later review)
- ☐ List of nearest clinics/hospitals at destination
Comfort items:
- ☐ Ginger candies or ginger supplement (mild anti-nausea benefit)
- ☐ Motion sickness wristbands (acupressure, if you find them helpful)
- ☐ Water bottle (stay hydrated)
3. Dietary Management (For Specific Conditions)
If Vestibular Migraine:
- ☐ List of trigger foods to avoid (keep in phone)
- ☐ Caffeine-free beverages for flight
- ☐ Approved snacks (non-migraine trigger)
If Menière’s Disease:
- ☐ Low-sodium snack options
- ☐ Salt substitute if needed
- ☐ Hydration reminder (aim for 1.5–2 L water daily)
4. Emergency Contacts & Medical Information
To carry:
- ☐ Insurance card + policy number
- ☐ List of current medications + dosages
- ☐ Allergies (clearly documented)
- ☐ Emergency contact (family member, doctor)
- ☐ Vestibular specialist contact (if available at destination)
5. Pre-Travel Checklist (48 Hours Before)
Medical:
- ☐ Confirm all medications packed + accessible
- ☐ Apply scopolamine patch 4–8 hours before departure (if using)
- ☐ Confirm you took preventative migraine medication (if on schedule)
Condition-specific:
- ☐ BPPV: Perform morning habituation exercises
- ☐ Migraine: Complete 48-hour dietary restriction
- ☐ Menière’s: Sodium intake <1,500 mg for last 2–3 days
- ☐ PPPD: Complete visual desensitization exercises
Logistical:
- ☐ Know your seat assignment (if flying, request front seat or aisle for vestibular patients)
- ☐ Plan your route from home to airport/dock/station (minimize unexpected motion)
- ☐ Confirm you have all tools (neck pillow, earplugs, target card)
MOTION SICKNESS vs. VERTIGO
(Key Distinction for Travelers)
| Aspect | Motion Sickness | Vertigo |
|---|---|---|
| Definition | Nausea/vomiting from sensory mismatch during travel | False sensation of spinning or rotation |
| Trigger | Motion (car, plane, ship, amusement rides) | Inner ear dysfunction, head movement, position change |
| Sensation | Nausea, vomiting, dizziness, sweating | Spinning, rotating, tilting sensation |
| Duration | During motion + 30 min–few hours after | Minutes to hours (acute vertigo) or persistent (chronic) |
| Mechanism | Sensory conflict (vestibular ≠ visual ≠ proprioceptive) | Vestibular system malfunction or central cause |
| Best prevention | Pre-travel habituation + horizon fixation | Condition-specific treatment (BPPV maneuver, migraine prevention, etc.) |
| Medication | Scopolamine, meclizine, dimenhydrinate | Depends on cause (SSRI for PPPD, beta-blocker for migraine, etc.) |
| Recovery | Habituation (brain adapts to motion patterns) | Treat underlying condition |
| Travel-friendly | Yes (with preparation) | Depends on condition severity + treatment |
>
ENGLISH FAQs (20 Questions)
1. What is motion sickness and how is it different from vertigo?
Motion sickness = sensory mismatch between vestibular (inner ear), visual (eyes), and proprioceptive (body position) systems = universal = affects most people under sufficient stimulus. Vertigo = false sensation of spinning = inner ear dysfunction or neurological issues. Key differences: Motion sickness occurs DURING motion (car, plane, ship); vertigo can occur at REST. Motion sickness is temporary and preventable through habituation; vertigo is condition-specific. Motion sickness triggers: sensory conflict. Vertigo triggers: inner ear pathology or central lesion. Treatment approach differs: motion sickness = habituation + horizon fixation; vertigo = condition-specific (BPPV maneuver, migraine meds, SSRI for PPPD). Understanding distinction guides treatment.
2. What is the sensory mismatch theory of motion sickness?
Mismatch theory states: Motion sickness occurs when vestibular, visual, and somatosensory systems provide CONFLICTING information. Classic example: Reading in moving car = inner ear detects acceleration/turns (motion), but eyes see stationary page (no motion), feet feel seat movement. This 3-way conflict is interpreted by brain’s medullary vomiting center as neurotoxicity threat (evolutionary logic: “If senses conflict, possibly poisoned → vomit to protect”). This ancient defense mechanism is triggered inappropriately by modern travel. Solution: Align sensory systems (horizon fixation aligns visual + vestibular).
3. Why is the 5-minute pre-travel vestibular habituation hack effective?
The 5-minute daily hack (X1 gaze stabilization + head-moving exercises, performed 7 days before travel) works because it “teaches” the brain to EXPECT motion patterns. Neural plasticity mechanism: Brain updates its stored expectations based on repeated sensory input. By exposing the vestibular system to CONTROLLED, PREDICTABLE motion beforehand, the system becomes DESENSITIZED to motion during travel. Result: Brain’s expected motion patterns MATCH actual travel motion = less sensory conflict = less mismatch = less nausea. Pilots and sailors naturally develop tolerance through cumulative exposure. This is why professional navigators rarely get motion sickness.
4. How does gaze stabilization (X1 viewing) exercise prevent motion sickness?
X1 viewing strengthens the vestibulo-ocular reflex (VOR) = the reflex that automatically stabilizes eyes during head movement. Setup: Focus on small letter, move head rapidly side-to-side while keeping letter clear. Eyes must move OPPOSITE to head (compensatory movement). Neural effect: This trains the neural pathways controlling VOR, making gaze MORE stable and compensatory eye movements MORE automatic. Benefit: Stronger, faster VOR = stable visual field during travel = brain receives consistent visual input even during motion = less visual-vestibular conflict = less nausea. Perform 3 sets × 15 reps = 3–5 minutes daily for 7 days pre-travel.
5. Why do drivers rarely get motion sickness?
Drivers generate an efference copy = an internal “prediction” or motor model of exactly what motion to expect based on their steering commands. Mechanism: Motor cortex sends command (“Turn wheel 30° right”), and simultaneously generates efference copy: “I expect forward acceleration + rightward rotation.” When actual vestibular + visual input MATCHES this prediction, no sensory conflict occurs. Passengers lack this: They have no steering control, so their motor cortex cannot predict motion, leading to sensory conflict. This is why taking the driving shift is the MOST effective motion sickness prevention during car travel. Even brief periods of driving improve tolerance.
6. How does horizon fixation help passengers prevent motion sickness?
The distant horizon provides a relatively STABLE visual reference even during vehicle motion. Mechanism: By fixating on a distant point (mountain, tree, horizon line), passengers give their visual system a stable target that ROUGHLY MATCHES the motion their vestibular system is detecting. This reduces the mismatch between visual and vestibular signals. Key detail: Front seat positioning is crucial because the horizon appears at the same visual angle as actual vehicle motion. Back seat horizons appear to move FASTER than actual vehicle motion (visual-vestibular mismatch worsens). Why effective: Horizon is taught to sailors, pilots, and professional drivers as PRIMARY motion sickness prevention because it’s biomechanically sound.
7. What is the “head lock” strategy and when should it be used?
The head lock strategy = keeping head STILL and SUPPORTED during high-acceleration phases (takeoff, landing, severe turbulence, winding roads). Why: Coriolis effects = spatial disorientation from simultaneous motion in multiple planes. Example: Plane pitching (nose up) while you turn your head side-to-side = semicircular canals experience maximal conflicting signals = extreme nausea. Technique: Use neck pillow for support, move ONLY eyes (not head), maintain rigid head position. Timing: Apply during takeoff/landing. Once plane reaches cruising altitude (steady motion), vestibular system adapts quickly, and head movement becomes safe. This principle applies to all high-acceleration environments (roller coasters, mountain roads, power starts in cars).
8. Why must head movement be avoided in extreme acceleration environments?
Extreme acceleration in multiple planes = maximal sensory conflict. Neurophysiology: Semicircular canals detect rotation, otoliths detect linear acceleration. When head moves in multiple planes WHILE vehicle accelerates in different planes, the combined signal is maximal conflicting information. This triggers the strongest nausea and spatial disorientation (Coriolis effect). Example: Pitch (plane tilting nose-up) + roll (wing dipping) + your head tilting = triplanar conflict = severe disorientation. Solution: Rigid head position minimizes complexity of vestibular input. Once plane reaches steady cruising (single plane motion), brain adapts within minutes, and head movement becomes safe. This explains why most flight sickness occurs during takeoff/landing, not cruising.
9. What special preparations are required for patients with BPPV, migraine, Menière’s, or PPPD traveling?
BPPV: Morning head exercises (distribute otoconia), avoid rapid head turns, head stability during takeoff/landing. Migraine: 48–72 hour dietary restriction (avoid tyramine, nitrites, chocolate, caffeine, alcohol, MSG), preventative medications (metoprolol, topiramate, CGRP) started 2–4 weeks before, hydration (400–500 ml every 2–3 hours). Menière’s: Sodium restriction (<1,500 mg/day) 5–7 days pre-travel, diuretics, pressure-regulating earplugs during flight (prevents Tullio phenomenon), avoid caffeine/alcohol. PPPD: Visual desensitization (watch moving scenes from windows, 30–60 sec daily, increasing duration), anxiety management (relaxation, SSRI if prescribed), gradual exposure (short car trips before long journeys). One-size-fits-all approach fails—condition-specific strategies essential.
10. How do pressure-regulating earplugs work and which patients need them?
Pressure-regulating earplugs have a small valve that gradually EQUALIZES air pressure as cabin pressure changes during altitude shifts. Why needed: Rapid pressure changes during takeoff/landing can trigger Tullio phenomenon (sound/pressure-induced vertigo), particularly in Menière’s disease or pressure-sensitive vestibular patients. Mechanism: Valve allows slow pressure equilibration, preventing eardrum tension and inner ear barotrauma that trigger vertigo. Who needs: Menière’s patients (essential), patients with previous pressure-triggered vertigo, BPPV patients, those with Eustachian tube dysfunction. Application: Insert before takeoff, keep in throughout flight. Side benefit: Reduces ear pain during descent. Inexpensive, available over-counter (brand: Ear Planes).
11. What is the best medication to take before flying and when should it be applied?
Scopolamine (hyoscine) transdermal patch = GOLD STANDARD: Apply 4–8 hours BEFORE travel (NOT day-of). Provides 72 hours protection = 70–80% motion sickness prevention. Advantages: Long-acting, single application, high efficacy. Disadvantages: Blurred vision, dry mouth, cannot use if angle-closure glaucoma. Alternative: Meclizine 25–50 mg, taken 30 minutes–1 hour BEFORE travel, repeated every 4–6 hours. Lower efficacy (50–70%) but less sedating. CRITICAL: Never use suppressants >1–3 consecutive days = brain stops adapting = WORSE outcomes. For flights >12 hours, use scopolamine (single patch covers entire duration) rather than repeated meclizine doses. Ondansetron (Zofran) 4–8 mg = rescue for breakthrough nausea (works 30–60 min).
12. What is the 72-hour rule for motion sickness medications?
72-hour rule: Never use vestibular suppressants (scopolamine, meclizine, dimenhydrinate, benzodiazepines) for >1–3 consecutive days. Why: These drugs chemically SUPPRESS the vestibular system, BLOCKING the brain’s natural ability to adapt (central compensation). When medication stops, vestibular system is WEAKER, not stronger. Prolonged use can cause medication-induced chronic motion sickness—patient becomes permanently dependent. Example outcome: Patient takes meclizine for week-long cruise, feels ok. Upon stopping, experiences WORSE motion sickness than before medication. Some patients become chronically medication-dependent—tragic outcome. Safe approach: Use medication only for travel duration, limit 1–3 days max, allow 3–5 days post-travel for brain recalibration (mild queasiness normal—NOT sign to restart medication), maintain daily movement.
13. How should breakthrough motion sickness during travel be managed?
If nausea begins despite preventative measures: (1) Ondansetron (Zofran) 4–8 mg = different mechanism than preventatives = specifically targets nausea/vomiting center = works 30–60 minutes. (2) Slow, deep breathing = activates parasympathetic nervous system = naturally reduces nausea. (3) Gaze on distant horizon = visual-vestibular alignment. (4) Cold compress on wrists = acupressure-based, mild benefit. (5) Avoid sudden head movements = reduces vestibular input. (6) Ginger ale or ginger supplement = mild anti-nausea benefit (mechanism unclear, likely placebo + ginger’s antiemetic properties). Most important: Maintain head stability, don’t catastrophize—breakthrough symptoms are temporary and don’t indicate serious pathology. Resistance to repeat medication prevents dependence.
14. When should vestibular migraine patients start preventative medication before travel?
Start 2–4 weeks BEFORE travel. Examples: Metoprolol (beta-blocker) 25–50 mg twice daily = raises migraine threshold; Topiramate (Topamax) 25–100 mg twice daily = anticonvulsant; CGRP monoclonal antibodies (erenumab, fremanezumab) = monthly injection, excellent for travel-prone patients (60–70% attack reduction). Additionally: 48–72 hours before travel, implement strict dietary restriction = avoid tyramine (aged cheese, aged meat, soy sauce), nitrites (deli meats), chocolate, caffeine, alcohol, MSG. Maintain: Hydration (400–500 ml every 2–3 hours), sleep priority (sleep disruption = major trigger), regular meals (skipped meals trigger). Combination of preventative medication + dietary control + lifestyle management = optimal pre-travel approach for migraine patients.
15. What specific dietary changes should Menière’s disease patients implement before flying?
Sodium restriction: <1,500 mg/day for 5–7 days before travel (avoid salty snacks, fast food, canned items, restaurant meals—all high sodium). Hydration: 1.5–2 L water daily = maintains fluid balance, reduces endolymphatic pressure. Medications: Continue/restart diuretics if prescribed (e.g., furosemide 20–40 mg daily) = reduces inner ear fluid pressure. Avoid: Caffeine (increases inner ear pressure), alcohol (diuretic + fluid shifts), high-salt foods. Add: Pressure-regulating earplugs during flight = prevents Tullio phenomenon. Rationale: Menière’s involves abnormal endolymphatic fluid pressure. Sodium restriction + diuretics = reduce pressure. Hydration = maintain balanced fluid environment. Earplugs = prevent pressure-induced vertigo during altitude changes. These measures significantly reduce attack risk during travel stress.
16. How should PPPD patients prepare for air travel or long car journeys?
Pre-travel (7–10 days before): (1) Visual desensitization = watch moving traffic from windows, start 15–30 sec, gradually increase to 5+ minutes daily (targets visual dependency); (2) Anxiety management = SSRIs at therapeutic dose (don’t start day-before—already therapeutic), relaxation techniques (yoga, breathing), exposure hierarchies (short car trips before long); (3) Confidence building. During travel: Front seat (NOT back), fixate on distant horizon, avoid phone scrolling (triggers visual vertigo), use neck pillow for head support, maintain slow head movements. Pharmacology: Scopolamine patch (24–48 hours) if necessary, but gradual habituation safer long-term. Principle: PPPD thrives on avoidance; confronting feared travel situations systematically reduces anxiety + dizziness. Each successful trip = brain learns “Travel is safe, not threatening.”
17. What role does mental preparation and psychological strategy play in preventing motion sickness?
Mental preparation is CRUCIAL. Mechanism: Catastrophic thinking (“I’ll be sick the whole flight”) activates threat system (amygdala), worsening vestibular sensitivity + dizziness. Evidence-based mental strategies: (1) Reframe: “My body is adapting to new sensations—this is NORMAL adaptation, not danger”; (2) Visualization: Mentally rehearse successful travel without nausea (activates same neural pathways as actual experience); (3) Distraction: Engage in interesting activities (movies, books, conversation, work) = reduces hypervigilance to body sensations; (4) Mindfulness: Observe dizziness without judgment, resist fighting it (paradoxically reduces severity); (5) Self-compassion: “This is temporary discomfort, not weakness.” Psychological preparation is often AS important as medication—some patients achieve full control through mindfulness alone.
18. How should patients maintain vestibular health immediately after travel to prevent post-travel decompensation?
Post-travel (1–5 days after arrival): (1) Continue daily movement = walk, exercise, gentle vestibular activities (don’t “rest” the system); (2) Perform VRT exercises = 5–10 minutes daily = maintains central compensation (gaze stabilization, balance training, head turns); (3) Avoid prolonged bed rest = immobility worsens decompensation; (4) Maintain sleep + hydration = critical for neural recovery; (5) Avoid caffeine/alcohol excess = both can trigger residual symptoms; (6) Practice relaxation = manage any travel-related anxiety; (7) If symptoms persist >3–5 days: Mild queasiness is EXPECTED during brain recalibration—this is NORMAL, NOT sign of disease. Critical: Do NOT restart medication unless nausea is severe—this delays adaptation. Most post-travel symptoms resolve within 1 week with continued movement.
19. What comprehensive items should be included in a vertigo travel kit?
(1) Medications: Scopolamine patches (2–3 for long trips), meclizine tablets (10–15), ondansetron (5–10 for breakthrough), preventative migraine meds, diuretics (if Menière’s). (2) Mechanical tools: Target card (X1 viewing exercises during transit), neck pillow (head lock strategy), pressure-regulating earplugs (altitude changes). (3) Documentation: Medication list with dosages, prescription copies, clinic contact numbers (destination + home), insurance cards. (4) Comfort items: Ginger candies, motion sickness wristbands, reusable water bottle. (5) Dietary: Migraine-safe snacks, low-sodium options (Menière’s), caffeine-free beverages. (6) Tracking: Vertigo/nausea diary (document triggers + severity), smartphone with camera (record eye movements if vertigo occurs—useful for later medical review). Packing: 2–3 days before departure to avoid rushed decisions.
20. When should someone with travel-related vertigo seek specialist evaluation before travel?
Consult ENT/vestibular specialist 7–10 days before travel if: (1) History of severe motion sickness or vertigo triggered specifically by travel; (2) Confirmed diagnosis of BPPV, vestibular migraine, Menière’s disease, or PPPD requiring pre-travel optimization; (3) Previous travel-triggered attacks lasting >3 days; (4) Severe anxiety about traveling despite previous successful trips; (5) Need for customized medication regimen or personalized VRT protocol. Specialist provides: (1) Confirm diagnosis (ensures treatment targets correct condition); (2) Prescribe condition-specific medications (not one-size-fits-all); (3) Teach pre-travel vestibular habituation exercises (customized for condition); (4) Develop personalized travel kit (tailored to diagnosis + trip duration); (5) Provide reassurance + realistic expectations (reduces anxiety). Timing: Pre-travel specialist consultation (7–10 days before departure) significantly improves travel outcomes and reduces travel-related anxiety.
📞 PRIME ENT CENTER CONTACT INFORMATION
Dr. Prateek Porwal, MBBS, MS, DNB, CAMVD (Yenepoya)
Senior ENT Specialist | Vestibular Travel Medicine & Balance Disorders
University Certified Neurotologist (India)
11 Years of Clinical Experience
PRIME ENT Center
Clinic Location:
Nagheta Road, Near Income Tax Office
Jindpeer Chauraha, Hardoi
Uttar Pradesh 241001, India
Contact Details:
- Phone: +91 73930 62200
- Email: primeenthdi@gmail.com
- Website: https://primeentcenter.in
Consultation Timings:
- Monday to Saturday: 11:00 AM–04:00 PM | 06:00 PM–08:00 PM
- Sunday: Closed
- Emergency Services: Available through main contact number
Why Choose PRIME ENT Center for Travel Vertigo Planning?
✓ Pre-Travel Vestibular Assessment – Confirm your diagnosis before travel; identify specific triggers
✓ Personalized Medication Plans – Safe, condition-specific medication protocols (scopolamine, meclizine, preventatives)
✓ Vestibular Habituation Protocol – Customized 7-day pre-travel exercise plan based on your condition
✓ Condition-Specific Strategies – BPPV, migraine, Menière’s, PPPD—each has a travel protocol
✓ Medication Safety Expertise – “72-Hour Rule” education; prevention of medication-induced chronic motion sickness
✓ Travel Kit Development – Personalized list of medications, tools, and emergency protocols
✓ Post-Travel Follow-Up – Ensure brain recalibration after travel; prevent deconditioning
✓ 3-Language Consultation – English, Hindi, Hinglish; family education supported
Book Your Travel Consultation Today
Planning a trip? Have a vestibular condition? Prepare safely:
📱 Call: +91 73930 62200
💬 WhatsApp: +91 73930 62200
📧 Email: primeenthdi@gmail.com
🌐 Website: https://primeentcenter.in
Pro tip: Schedule your pre-travel consultation 7–10 days before departure for maximum benefit.
What to Bring to Your Travel Consultation
- Travel itinerary: Dates, destinations, mode of transportation (car, plane, ship)
- Symptom history: Previous motion sickness or vertigo experiences during travel
- Current medications: List of all medications, including preventatives
- Vestibular diagnosis: If known (BPPV, migraine, Menière’s, PPPD, etc.)
- Questions about: Safe medication use, specific exercise protocols, destination-specific strategies
- Travel companions: If relevant (family who can help with management)
About Dr. Prateek Porwal
Dr. Prateek Porwal specializes in vestibular disorders and travel medicine, helping patients with balance conditions achieve confident, comfortable journeys. With over 11 years of clinical experience and advanced training in neuro-otology, Dr. Porwal provides personalized pre-travel assessments, medication protocols, and habituation training.
His philosophy: Travel with vertigo is possible—with proper preparation, the world is still yours to explore.
Don’t let vertigo keep you grounded. Plan your travel safely with PRIME ENT Center.
