🎯 TL;DR (Too Long; Didn’t Read)
In my practice in Hardoi, I see these cases regularly. Based on my clinical experience with hundreds of patients, here’s what actually works.
- Main concept: PPPD (Persistent Postural-Perceptual vertigo-statistics/”>Dizziness) = anxiety + brain’s threat system overdrive—NOT structural ear problem
- Brain connection: Vestibular system directly wired to amygdala (fear center); anxiety triggers false “balance alarms”
- Common misconception: “All in your head”—WRONG; it’s a real functional disorder, not psychiatric (though anxiety is involved)
- Diagnostic test: Standard imaging (MRI, hearing tests) = NORMAL (explains why doctors say “nothing wrong”)
- Diagnostic criteria: 3+ months symptoms, triggered by upright posture/movement/complex visuals (supermarket effect)
- Best treatment combination: SSRI medication + Cognitive Behavioral Therapy (CBT) + vestibular rehabilitation Therapy (VRT) = 70–80% improvement
- Critical mistake: Bed rest + avoidance = WORSE (isolates patient, maintains threat loop; movement + exposure = recovery)
- Last medically reviewed: February 2026
ENGLISH VERSION
Your Anxiety Is Literally Making You Dizzy: The Stress-Vertigo Link (And How to Break It)
Introduction: The Scenario That Changes Lives
Anxiety causing dizziness and stress vertigo is a common scenario encountered by millions. When you find yourself in a crowded supermarket, walking through aisles stacked with products, suddenly, the world feels “off”. You might feel as though you are rocking on a boat, floating, or about to tip over, despite there being no actual movement. Your heart rate accelerates. Panic sets in. You think, “Am I having a stroke? Is this a heart attack?” You grab onto a shelf, feeling desperate.
📋 Table of Contents
- 🎯 TL;DR (Too Long; Didn’t Read)
- Your Anxiety Is Literally Making You Dizzy: The Stress-Vertigo Link (And How to Break It)
- Introduction: The Scenario That Changes Lives
- What Is This Feeling? From “Chakkar” to PPPD
- Dizziness: A Broad Spectrum
- PPPD: The Modern Understanding
- The Diagnostic Criteria for PPPD
- Criterion 1: Duration (3+ Months)
- Criterion 2: Persistence
- Criterion 3: Triggers (Hallmark Features)
- Criterion 4: Inciting Event
- The Science of the Link: How Anxiety Affects Balance
- The Vestibular-Amygdala Connection
- The Threat System Overdrive
- The “Closed-Loop” Strategy: Why Your Efforts Are Failing
- Open-Loop vs. Closed-Loop Balance
- The Paradox: Effort Makes You More Unstable
- The Cerebellum’s Role
- Visual Vertigo: The Challenge of the Modern World
- Visual Dependency: When Eyes Rule the Vestibular System
- Common Triggers of Visual Vertigo
- Breaking the Link: A Multi-Step Approach
- The Frustration of “Normal” Test Results
- Pillar 1: Medication—SSRI/SNRI (“Training Wheels” for the Brain)
- Pillar 2: Cognitive Behavioral Therapy (CBT)—De-Catastrophising the Spin
- Pillar 3: Vestibular Rehabilitation Therapy (VRT)—Desensitization Through Movement
- Neural Pathways of Balance
- The Anatomical Basis for the Anxiety-Vertigo Link
- The Vestibular-Amygdala-Cortical Loop in PPPD
- Practical Advice for the Patient
- Do’s and Don’ts for PPPD Recovery
- Specific Strategies
- Conclusion: Breaking the Vicious Cycle
- Your Anxiety Is Literally Making You Dizzy: Stress-Vertigo Link (और Break करो)
- Introduction: Scenario जो Lives Change करता है
- What Is This Feeling? “Chakkar” से PPPD तक
- Dizziness: Broad Spectrum
- PPPD: Modern Understanding
- PPPD की Diagnostic Criteria
- Criterion 1: Duration (3+ Months)
- Criterion 2: Persistence
- Criterion 3: Triggers (Hallmark)
- Criterion 4: Inciting Event
- The Science of Link: Anxiety कैसे Balance को Affect करता है
- Vestibular-Amygdala Connection
- Threat System Overdrive
- “Closed-Loop” Strategy: Why Efforts Failing
- Open-Loop vs. Closed-Loop
- Paradox: Effort = More Instability
- Visual Vertigo: Modern World की Challenge
- Visual Dependency
- Common Triggers
- Breaking Link: Multi-Step Approach
- Pillar 1: Medication (SSRI/SNRI)
- Pillar 2: Cognitive Behavioral Therapy (CBT)
- Pillar 3: Vestibular Rehabilitation Therapy (VRT)
- Practical Advice
- Do’s and Don’ts
- Specific Strategies
- Conclusion
- Your Anxiety Is Literally Making You Dizzy: Stress-Vertigo Link (और इसे Break करो)
- Introduction: Scenario जो Lives Change करता है
- क्या Is This Feeling? “Chakkar” से PPPD तक
- Dizziness: Broad Spectrum
- PPPD: Modern Understanding
- PPPD की Diagnostic Criteria
- Criterion 1: Duration (3+ Months)
- Criterion 2: Persistence
- Criterion 3: Triggers (Hallmark)
- Criterion 4: Inciting Event
- The Science of Link: Anxiety कैसे Balance को Affect करता है
- Vestibular-Amygdala Connection
- Threat System Overdrive
- “Closed-Loop” Strategy: Why Efforts Failing
- Open-Loop vs. Closed-Loop
- Paradox: Effort = More Instability
- Visual Vertigo: Modern World की Challenge
- Visual Dependency
- Common Triggers
- Breaking Link: Multi-Step Approach
- Pillar 1: Medication (SSRI/SNRI)
- Pillar 2: Cognitive Behavioral Therapy (CBT)
- Pillar 3: Vestibular Rehabilitation Therapy (VRT)
- Practical Advice
- Do’s and Don’ts
- Specific Strategies
- Conclusion
- (Reference Table – Differential Diagnosis & Treatment Approach)
- (Step-by-Step Protocol for Daily Practice)
- Exercise Program Structure
- Week 1–2: Foundation Exercises (Begin Here)
- Exercise 1A: Gaze Stabilization (X1 Viewing) – Sitting
- Exercise 1B: Gaze Stabilization (X1 Viewing) – Standing
- Exercise 2: Postural Stability – Standing on a Firm Surface
- Exercise 3: Visual Tracking (Optokinetic Stimulation)
- Week 3–4: Intermediate Exercises
- Exercise 4: Balance on Unstable Surface (Foam or Pillow)
- Exercise 5: Gait Training with Head Turns
- Exercise 6: Real-World Exposure (Gradual Desensitization)
- Week 5–8: Advanced Exercises
- Exercise 7: Dynamic Balance – Tandem Stance with Movement
- Exercise 8: Visual Desensitization – Complex Environments
- Exercise 9: Vestibular-Proprioceptive Integration – Single-Leg Stance Variations
- Week 9–12: Maintenance & Functional Training
- Exercise 10: Real-World Functional Activities
- Maintenance Protocol (After 12 Weeks)
- (Physical & Psychological Benefits for PPPD)
- Why Yoga Is Vital for PPPD
- Yoga’s Mechanisms for PPPD Recovery
- Recommended Yoga Practice for PPPD
- Complete FAQ Section for Missing Content
- ENGLISH FAQs (20 Questions)
- HINGLISH FAQs (20 Questions)
- HINDI FAQs (20 Questions)
- Dr. Prateek Porwal, ENT & Vertigo Specialist | MBBS, DNB ENT, CAMVD | Prime ENT Center, Hardoi
- PRIME ENT Center
- Why Choose PRIME ENT Center for PPPD & Anxiety-Related Dizziness?
- Book Your Consultation Today
- What to Bring to Your PPPD Consultation
- About Dr. Prateek Porwal
- References
Or perhaps you are driving on a busy motorway. Traffic surrounds you. The feeling comes—not a spinning sensation exactly, but a sense of being “unsteady,” “spaced out,” or “not quite there.” You grip the steering wheel harder. Your foot trembles on the pedal.
For months or years, you may have experienced this. You have seen multiple doctors. You have undergone MRI scans, hearing tests, and vestibular evaluations—all normal. One doctor says, “It’s just stress.” Another says, “It’s all in your head.” You leave feeling confused, frustrated, and invalidated.
But here is the truth: Your anxiety IS literally making you dizzy. And it is not “all in your head”—it is a real, diagnosable medical condition with a distinct neurobiological mechanism.
What Is This Feeling? From “Chakkar” to PPPD
Dizziness: A Broad Spectrum
“Dizziness” is a broad, nonspecific term used to describe sensations ranging from light-headedness to a loss of stable balance. While “vertigo” specifically refers to a false sensation of spinning or self-motion, many people experience a different kind of “dizziness” characterised by a sense of being “spaced out,” “unsteady,” “floating,” or “rocking.”
This distinction is important: A patient with true vertigo experiences spinning. A patient with PPPD experiences unsteadiness, spatial disorientation, or a sense of instability—but often WITHOUT actual spinning.
PPPD: The Modern Understanding
Medical experts now classify anxiety causing dizziness and stress vertigo—or this chronic, stress-linked dizziness—as Persistent Postural-Perceptual Dizziness (PPPD). This condition integrates previous diagnostic labels like:
- Phobic Postural Vertigo (PPV) – dizziness triggered by fear of falling
- Chronic Subjective Dizziness (CSD) – persistent dizziness without visible vestibular dysfunction
- Space and Motion Discomfort (SMD) – disorientation in visually complex environments
PPPD is a chronic functional vestibular disorder. This means:
- It is NOT a structural defect in the inner ear (hence normal imaging)
- It is NOT a primary psychiatric illness (though anxiety is involved)
- It IS a change in how the brain processes balance information—a “software” problem, not a “hardware” defect
The Diagnostic Criteria for PPPD
To be diagnosed with PPPD, a patient typically meets several specific criteria:
Criterion 1: Duration (3+ Months)
Symptoms of dizziness, unsteadiness, or non-spinning vertigo must be present on most days for three months or more. This distinguishes PPPD from acute vertigo (BPPV, vestibular neuritis), which resolves in weeks.
Criterion 2: Persistence
The sensation lasts for hours at a time, though it may wax and wane in intensity. The symptom is chronic and constant, not episodic like BPPV attacks.
Criterion 3: Triggers (Hallmark Features)
Symptoms are exacerbated by THREE categories of triggers:
1. Upright Posture (Standing, Walking)
- Symptoms worse when standing upright compared to sitting or lying down
- Walking provokes more dizziness than standing still
- The worse the situation, the worse the symptoms (crowds, open spaces, escalators)
2. Active or Passive Movement
- Head movements, body rotations
- Passive motion (riding in a car, escalator, elevator)
- Rapid direction changes
- Exposure to motion without ability to control it
3. Complex Visual Stimuli
- Visually busy environments (supermarket aisles, shopping malls with many stacked items)
- Large-field motion: passing traffic, action movies, crowds
- Repetitive patterns: striped clothing, checkered floors, scrolling text
- Fluorescent lighting or flickering screens
- Computer work or mobile phone scrolling
Criterion 4: Inciting Event
PPPD is usually triggered by a medical event that causes acute dizziness, such as:
- Vestibular event: Inner ear infection, BPPV, vestibular neuritis, migraine-related vertigo
- Cardiac event: Syncope (fainting), arrhythmia, blood pressure drop
- Neurological event: TIA, seizure, concussion
- Psychological event: Acute panic attack, severe stress, trauma
After the acute event, most people recover within weeks. However, in some individuals—particularly those with anxiety-prone temperaments—the brain’s threat detection system remains “on,” leading to persistent dizziness even after the ear or heart has healed.
The Science of the Link: How Anxiety Affects Balance
The Vestibular-Amygdala Connection
The reason your anxiety can make you dizzy lies in deep neuro-anatomical connections between your vestibular (balance) system and your threat evaluation system (amygdala).
The anatomical pathway:
- Vestibular nuclei (in the brainstem) = primary processing center for balance signals
- Direct connections to the amygdala (brain’s fear/panic center) = bidirectional
- When balance signals are abnormal → amygdala activates → fear response
- When amygdala is activated (anxiety, panic) → vestibular nuclei become hyperactive → perceived dizziness
Key insight: The vestibular system does not exist in isolation. It is deeply integrated with emotional centers. Balance and fear are neurologically intertwined.
The Threat System Overdrive
When you experience a balance crisis (violent vertigo, fainting, panic attack), your brain’s threat system goes into high alert. This is adaptive: Your brain is trying to protect you. It learns, “Movement is dangerous. Balance is unreliable. Be vigilant.”
In most people, this alert fades as the ear heals or the anxiety resolves. The threat system “stands down.” The brain recalibrates: “Actually, balance is fine now. I can move freely.”
However, in some individuals—particularly those with anxious temperaments, perfectionism, or a history of anxiety—the threat system remains “on.” This leads to:
- Hyper-vigilance: Constant monitoring of body position and movement
- Fear of falling: Even on a flat surface with no actual fall risk
- Catastrophic thinking: “If I feel slightly unsteady, I will definitely fall”
- Avoidance behavior: Avoiding crowds, driving, open spaces—anything that triggers dizziness
- Positive feedback loop: The more you avoid, the more sensitive your threat system becomes. The more sensitive your threat system, the more you avoid.

The “Closed-Loop” Strategy: Why Your Efforts Are Failing
Open-Loop vs. Closed-Loop Balance
Normally, your brain manages balance in an “open-loop” fashion.
In open-loop control, balance happens automatically and unconsciously. You walk without thinking about it. You don’t have to consciously contract your leg muscles or monitor your center of gravity. The cerebellum handles it all in the background.
When you are anxious or have had a balance insult, you switch to a “closed-loop” or “high-demand” strategy.
In closed-loop control, you become consciously aware of balance tasks. You might:
- Stiffen your posture to feel more “stable”
- Walk more rigidly, legs held tight
- Co-contract muscles in your neck and legs (holding them tense for stability)
- Monitor your balance constantly: “Am I upright? Will I fall?”
- Scan the environment for potential hazards
The Paradox: Effort Makes You More Unstable
Ironically, this increased effort makes you more unstable.
By focusing consciously on a task that should be automatic, you create a sensorimotor mismatch between what your brain expects (automatic, fluid movement) and what it feels (rigid, controlled, effortful movement). This mismatch is perceived as a threat.
Result: The very dizziness you are trying to prevent by “stiffening up” is actually created by the stiffening.
This is the core trap of PPPD: The strategies patients use to manage dizziness (avoidance, rigidity, hypervigilance) are exactly the strategies that maintain and worsen the dizziness.
The Cerebellum’s Role
The cerebellum is the brain’s primary balance processor. It expects to operate in the background, adjusting posture and movement automatically. When the conscious cortex takes over and tries to “manage” balance, the cerebellum becomes confused.
The cerebellum’s feedback to the cortex essentially says: “You’re not letting me do my job. Something is wrong. Alert the threat system.”
The threat system (amygdala) amplifies this signal: “Balance IS broken. Be afraid.”
And the cycle deepens.
Visual Vertigo: The Challenge of the Modern World
Visual Dependency: When Eyes Rule the Vestibular System
Many patients with PPPD suffer from visual vertigo or visual dependency. Here’s why:
Because the vestibular signals from the ear are perceived as unreliable (even though they’re actually fine), the brain shifts its preference for balance information from the inner ear to vision.
In healthy people, the vestibular system and vision work together in balance. But in PPPD, the brain essentially says, “I don’t trust the vestibular signals. I’ll rely only on what I see.”
The problem: When the visual field is moving rapidly, complex, or unpredictable, the visual system cannot keep up. The brain perceives, “The whole world is moving, so I must be moving, so I’m losing my balance.”
Common Triggers of Visual Vertigo
- Supermarket aisles: Many stacked items, moving people, repetitive patterns (especially in peripheral vision)
- Shopping malls: Open spaces, moving crowds, high ceilings, bright lights
- Large-field motion: Traffic, passing vehicles, crowds in motion
- Screens: Scrolling on mobile phones, watching action movies, computer work
- Repetitive patterns: Striped clothing, checkered floors, herringbone wood patterns
- Fluorescent lighting: Flicker, high contrast, unnatural color temperature
- Escalators and elevators: Visually disorienting environments with moving floors/walls
In each case, the visual field provides conflicting or overwhelming information about motion, and the brain interprets this as a balance threat.
Breaking the Link: A Multi-Step Approach
The Frustration of “Normal” Test Results
The most frustrating part of PPPD is that standard medical tests come back completely normal:
- MRI brain: Normal
- MRI inner ear: Normal
- Hearing tests: Normal
- Vestibular function tests (caloric, vHIT): Normal or near-normal
- Blood tests: Normal
- EKG (if cardiac workup done): Normal
This leads many patients to feel they are “going crazy” or that their symptoms are “all in their mind.”
Doctors may say things like:
- “Nothing is wrong with you”
- “You just need to relax”
- “It’s anxiety” (dismissively)
- “Have you considered seeing a psychiatrist?”
The truth: The symptoms are physically real and caused by a functional “software” problem in the brain’s vestibular processing, rather than a “hardware” defect in the ear. The brain’s threat detection system is miscalibrated. This is fixable.
Pillar 1: Medication—SSRI/SNRI (“Training Wheels” for the Brain)
Important distinction: Vestibular suppressants (like a vestibular suppressant) should be AVOIDED for PPPD. These medications quiet balance signals, which prevents the brain from recalibrating. (See Article #5: The Medication Trap.)
However, other medications are highly effective for PPPD:
Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) have been shown to significantly reduce symptoms of PPPD. These drugs work by:
- Raising the threshold for the brain’s overreactive balance circuits
- Quieting the “false alarms” sent by the threat system (amygdala)
- Reducing anxiety and hypervigilance
- Allowing the brain to recalibrate its balance expectations
Common medications:
- Paroxetine (Paxil, Seroxat) – 40–; strong evidence for PPPD
- an SSRI medication (Zoloft, Lustral) – 50–; well-tolerated
- an SNRI medication (Effexor, Efexor) – 75– (SNRI); particularly helpful if concurrent depression
- Escitalopram (Lexapro) – 10–; fewer side effects
Timeline: Most patients notice benefit within 2–4 weeks, with maximal benefit at 8–12 weeks.
Why they work: SSRIs increase serotonin availability in the amygdala and vestibular nuclei. Higher serotonin = lower threat perception = fewer false balance alarms.
Pillar 2: Cognitive Behavioral Therapy (CBT)—De-Catastrophising the Spin
CBT is a important tool for addressing the thinking patterns that sustain PPPD.
How catastrophic thinking maintains dizziness:
- You feel a slight sway
- You think catastrophically: “I’m going to fall” or “I’m having a stroke” or “I’ll never be normal again”
- Catastrophic thought activates the amygdala (fear center)
- Amygdala activation increases vestibular sensitivity
- Increased sensitivity causes MORE perceived dizziness
- You feel more dizzy, which confirms your catastrophic thought
- The loop tightens
What CBT does:
- Identifies catastrophic thoughts: “What specifically am I afraid will happen?”
- Challenges distortions: “Is this thought based on evidence? What would I tell a friend in this situation?”
- Develops realistic alternatives: “I felt slightly dizzy. That’s uncomfortable, but it doesn’t mean I’m falling or having a stroke.”
- Reduces avoidance behavior: Gradually exposing yourself to situations that trigger dizziness, in a controlled way, to prove to your brain that the threat is not real
- Builds confidence: Each time you enter a “scary” situation and nothing bad happens, your threat system recalibrates
Typical CBT approach for PPPD:
- Sessions: 8–12 sessions of 45–60 minutes each
- Format: Weekly or bi-weekly
- Homework: Exposure exercises, thought records, behavioral experiments
- Efficacy: 70–80% improvement in symptoms when combined with VRT and medication
Pillar 3: Vestibular Rehabilitation Therapy (VRT)—Desensitization Through Movement
Critical principle: VRT for PPPD is NOT about “fixing” the ear (the ear is fine). It is about teaching the brain to habituate to the signals it has been over-monitoring.
How habituation works:
- Your brain has learned, “Movement = danger. Dizziness = threat.”
- Through repeated, controlled exposure to movement and dizziness, your brain learns, “Movement happened. I didn’t fall. Nothing bad happened. The threat is not real.”
- Over time, the threat system “de-sensitizes.” Dizziness triggers less fear. Less fear = less physical dizziness.
VRT exercises for PPPD:
1. Gaze Stabilization (VOR Exercises)
Goal: Improve eye fixation during head movement, reducing visual dizziness
Exercise: X1 (Times One) Viewing
- Focus on a small target (dot on a wall) at eye level
- Move your head side-to-side slowly while keeping eyes fixed on the target
- Gradually increase head speed
- Repeat 10–15 times
- Progress: Perform while standing instead of sitting
Exercise: X2 Viewing (More Challenging)
- Hold a target (finger, pencil) at arm’s length
- Move your head toward the target while keeping eyes fixed on a distant object
- The relative motion between your hand and distant background increases vestibular demand
- Repeat 10–15 times
2. Visual Desensitization (Optokinetic Stimulation)
Goal: Reduce visual dependency; habituate to moving visual fields
Exercise: Optokinetic Nystagmus (OKN)
- Watch a moving pattern (or video of a scrolling checkerboard pattern)
- Follow the pattern with your eyes for 1–2 minutes
- This stimulates the visual system without requiring head movement
- Progress: Increase pattern speed, or add head movement while watching
Real-world practice:
- Scrolling through a news feed (which triggers visual vertigo in many patients)
- Watching action movies
- Sitting near a window watching traffic
- Initially in short bursts (30 seconds–1 minute), progressing to longer durations
3. Balance Retraining (Postural Stability)
Goal: Strengthen non-visual balance cues; reduce dependence on vision
Exercise: Standing on Foam with Eyes Closed
- Stand on foam or an unstable surface (foam pad, balance board)
- Close your eyes (removing visual input)
- This forces the brain to rely on vestibular and proprioceptive (internal body awareness) cues
- Maintain balance for 30–60 seconds
- Progress: Add arm movements, head turns, or light arm movements while balancing
Exercise: Tandem Standing (Heel-to-Toe)
- Stand with one foot directly in front of the other (heel of front foot touching toes of back foot)
- Maintain balance for 30 seconds
- Progress: Close your eyes, add arm movements, turn your head
Exercise: Single-Leg Stance
- Stand on one leg
- Maintain balance for 30 seconds
- Progress: Close your eyes, add arm movements, perform on an unstable surface
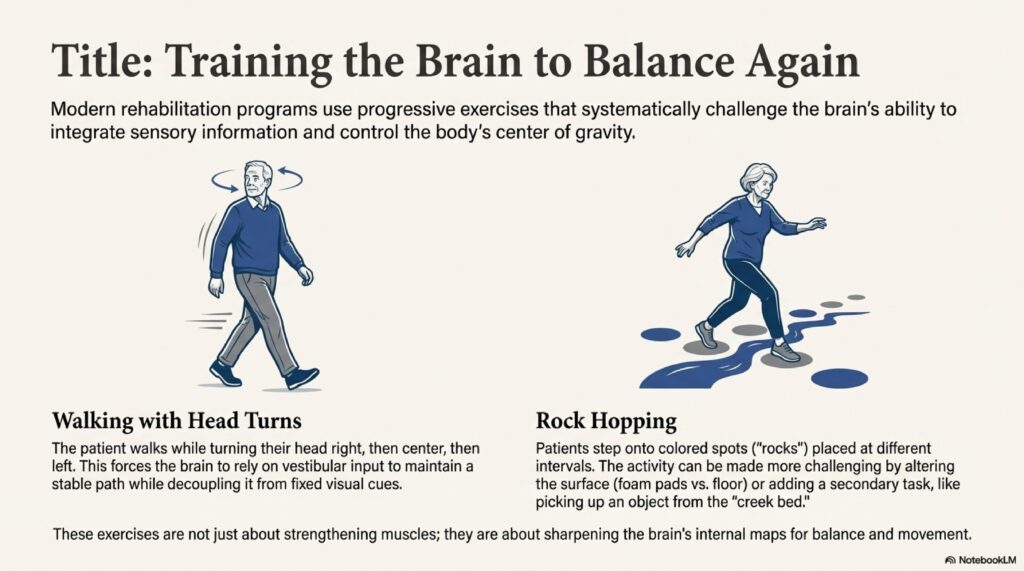
4. Gait Training with Head Turns
Goal: Integrate head-eye-body coordination; habituate to combined movements
Exercise: Marching with Head Turns
- Walk slowly, turning your head side-to-side while walking
- Continue for 1–2 minutes
- Progress: Walk faster, turn head faster, walk in different patterns (figure-8, around obstacles)
Exercise: Walking in Complex Environments
- Walk in a grocery store aisle (teh classic PPPD trigger)
- Walk around obstacles
- Walk in crowds (if safe)
- These real-world exposures are the most effective habituation
Timeline: Exercises should be performed 2–3 times per day, every day. Improvement usually takes 4–12 weeks, with continued benefits up to 6 months.
Neural Pathways of Balance
The Anatomical Basis for the Anxiety-Vertigo Link
Understanding the neurobiology of balance helps explain why anxiety and dizziness are so intertwined.
The Vestibulo-Ocular Reflex (VOR): Gaze Stability
The VOR is a three-neuron arc—one of the fastest reflex pathways in the nervous system:
- Vestibular nerve (from inner ear semicircular canals) detects head rotation
- Synapses directly on vestibular nuclei in the brainstem
- Synapses on extraocular motor nuclei (controlling eye muscles)
- Result: Within milliseconds, the eyes move opposite to the head, stabilizing gaze
Clinical test: During the HINTS exam (Article #1), an abnormal head impulse test suggests vestibular dysfunction or central cause.
In PPPD: The VOR is structurally and functionally normal. However, the brain’s INTERPRETATION of VOR signals is altered by threat processing.
Vestibulospinal Pathways: Postural Control
Two major descending pathways from the vestibular nuclei maintain posture:
1. Lateral Vestibulospinal Tract (LVST)
- Projects through the entire spinal cord
- Excites extensor muscles (legs, back)
- Maintains antigravity tone; prevents collapse
2. Medial Vestibulospinal Tract (MVST)
- Targets the cervical spinal cord (neck region)
- Controls head and neck position relative to body
In PPPD: These pathways are intact. However, conscious anxiety-driven “stiffening” hijacks these automatic pathways, creating the closed-loop rigidity described earlier.
Central Integration: The Vestibular Cortex
Beyond the brainstem, vestibular information ascends to the cortex:
- Vestibular nuclei → Thalamus → Parieto-Insular Vestibular Cortex (PIVC)
- PIVC = responsible for perception of self-motion and spatial orientation
- Connections to: Prefrontal cortex (decision-making), amygdala (emotion), insula (interoception—internal body awareness)
Key insight: The PIVC is connected to the amygdala. This is why anxiety literally alters vestibular perception.
The Vestibular-Amygdala-Cortical Loop in PPPD
Normal Balance:
Inner Ear → Vestibular Nuclei → Cerebellum → Automatic Postural Control
(Unconscious, automatic, fluid)
PPPD Loop:
Inner Ear (normal signals)
↓
Vestibular Nuclei (normal function)
↓
PIVC (Vestibular Cortex)
↓
Threat Evaluation (Amygdala) ← Hyper-responsive due to prior balance threat
↓
Increased Fear/Anxiety
↓
Prefrontal Cortex (conscious worry, catastrophic thinking)
↓
Hypervigilance to Balance Signals
↓
Closed-Loop Stiffening (loss of automatic control)
↓
Sensorimotor Mismatch
↓
PERCEIVED DIZZINESS (no structural problem)
↓
Fear Reinforced
↓
Loop TightensBreaking the loop requires:
- Medication (SSRI/SNRI) = Lower amygdala responsiveness
- CBT = Reframe threat evaluation; reduce catastrophic thinking
- VRT = Habituate the vestibular system; prove to the brain that dizziness is not dangerous
Practical Advice for the Patient
Do’s and Don’ts for PPPD Recovery
DON’T Do:
❌ Take “dizziness pills” (vestibular suppressants) long-term – They prevent the brain’s recalibration. (See Article #5.)
❌ Rest in bed – Immobility worsens PPPD by increasing deconditioning and anxiety.
❌ Avoid situations that trigger dizziness – Avoidance reinforces the threat system. The more you avoid, the worse PPPD becomes.
❌ Focus on the dizziness – Hypervigilance maintains the symptom. Distraction is therapeutic.
❌ Catastrophize about the meaning of dizziness – “I’m going to fall” or “This will never go away” perpetuates fear.
DO:
✅ Take SSRI/SNRI medication – Effectively reduces threat system overactivity.
✅ Engage in daily movement – Walking, gentle exercise, everyday activities. Movement activates the vestibular system and signals safety.
✅ Gradually expose yourself to triggers – Supermarket visits, driving, crowds. Each exposure without a negative outcome recalibrates your threat system.
✅ Practice CBT techniques – Challenge catastrophic thoughts. Use thought records. Practice exposure exercises.
✅ Perform VRT exercises – 2–3 times daily. Gaze stabilization, balance training, visual desensitization.
✅ Stay active and social – Isolation worsens PPPD. Engagement with others and activities accelerates recovery.
Specific Strategies
1. Limit Sedatives and Suppressants
If you must use a vestibular suppressant (e.g., for an acute vertigo attack), use it for NO MORE than 48–72 hours. Then begin tapering, even if dizziness persists. The brain needs to recalibrate without chemical suppression.
2. Keep a Vertigo/Dizziness Diary
Document:
- Date and time of dizziness episodes
- Trigger (supermarket? car ride? stressful situation?)
- Intensity (1–10 scale)
- Duration (seconds? minutes? hours?)
- Associated symptoms (anxiety? panic? fear of falling?)
- What helped? (distraction? movement? support from others?)
This diary helps:
- Confirm the PPPD diagnosis (pattern of triggers)
- Track improvement over weeks/months
- Identify personal triggers (important for CBT)
3. Relaxation Techniques: Yoga, Tai Chi, Breathing
Why these help:
- Lower the baseline activation of your threat system (amygdala)
- Improve proprioceptive awareness (body sense)
- Provide daily practice with balance and movement in a controlled setting
- Reduce anxiety independent of vestibular rehabilitation
Specific practices:
Yoga (45–60 minutes, 3–5×/week):
- Recommended styles: Hatha, Vinyasa, or gentle flow (avoid hot yoga or inversion-heavy classes initially)
- Key poses for vestibular health: Tree pose (balance), child’s pose (calming), cat-cow stretch (spinal mobility), warrior poses (proprioceptive challenge)
- Breathing practice (Pranayama): Diaphragmatic breathing activates the parasympathetic nervous system, reducing threat response
Tai Chi (20–30 minutes, 4–5×/week):
- Slow, controlled movements with constant balance challenges
- Meditative quality reduces anxiety
- Improves proprioception (body awareness)
- Gentle vestibular stimulation without overload
Simple Breathing Exercise (Daily, 5–10 minutes):
- Sit comfortably
- Inhale slowly through nose for 4 counts
- Hold for 4 counts
- Exhale slowly through mouth for 6 counts
- Pause for 2 counts
- Repeat 10–15 times
- This activates the parasympathetic (calming) nervous system
4. Gradual Exposure: The “Exposure Hierarchy”
Create a list of situations that trigger your dizziness, ranked by intensity (1–10 scale):
Example Hierarchy:
- Level 1 (Mild): Sitting in a quiet room scrolling on a phone
- Level 2: Standing while using a phone
- Level 3: Walking in a small grocery store aisle
- Level 4: Walking in a busy grocery store
- Level 5: Sitting in a moving car
- Level 6: Driving on a quiet road
- Level 7: Driving on a busy highway
- Level 8: Sitting in a crowded restaurant
- Level 9: Standing in a crowded shopping mall
- Level 10 (Severe): Walking through a mall during busy hours
Exposure protocol:
- Start with Level 1–2 situations
- Spend 15–30 minutes in that situation (or until anxiety peaks and begins to decrease)
- Do NOT leave until your anxiety is at least 50% reduced – This teaches your brain that the situation is safe
- Repeat the exposure 2–3 times
- Once comfortable at a level, progress to the next level
- Typical timeline: 1 level per week
Why this works: Each successful exposure tells your brain, “I was afraid something bad would happen. Nothing bad happened. The threat is not real.” Over time, the threat system re-calibrates.
Conclusion: Breaking the Vicious Cycle
The link between stress and dizziness is a physical reality, not a lack of willpower. If you feel subjectively unsteady, experience visual vertigo in supermarkets or while driving, or have persistent dizziness despite normal imaging, you are likely suffering from PPPD—a functional maladaptation of your vestibular-anxiety system.
PPPD is NOT:
- A defect in your inner ear (imaging is normal)
- A psychological illness (though anxiety is involved)
- “All in your head” (it’s a real neurobiological problem)
- Incurable (it responds well to treatment)
PPPD IS:
- A miscalibration of your brain’s threat detection system
- Treatable through a combination of medication, therapy, and rehabilitation
- Reversible with proper management
- Completely recoverable for most patients
The path to recovery:
- Medication (SSRI/SNRI) quiets the threat system
- CBT reframes catastrophic thinking and reduces avoidance
- VRT habituates the vestibular system to movement and perceived dizziness
- Active engagement (movement, social activity, exposure) accelerates recovery
By combining these three pillars, you break the vicious cycle. Within 8–12 weeks, most patients report 70–80% improvement. By 6 months, full functional recovery is often achieved.
You are not “going crazy.” Your anxiety is literally activating your vestibular system in a way that makes you feel dizzy. And that dizzy feeling can be resolved by addressing the anxiety, retraining your brain, and gradually proving to yourself that movement—and life—are safe.
HINGLISH VERSION
Your Anxiety Is Literally Making You Dizzy: Stress-Vertigo Link (और Break करो)
Introduction: Scenario जो Lives Change करता है
Scenario = millions को encounter होता है। Crowded supermarket, aisles walk कर रहे हो products से। Suddenly, world “off” feel होता है। Boat पर rock करने जैसा feel, या floating, या tip over होने जैसा—लेकिन कोई actual movement नहीं है। Heart rate accelerate, panic set। Think करते हो “stroke? Heart attack?” Shelf को grab, desperate feel।
या busy motorway पर drive कर रहे हो। Traffic surround। Feeling आता है—spinning sensation नहीं exactly, लेकिन “unsteady,” “spaced out,” या “not quite there” feel। Steering wheel को tight grip।
Months या years के लिए experience किया हो सकता है। Multiple doctors देखे। MRI, hearing tests, vestibular evaluation—सब normal। Doctor कहता है “just stress” या “all in your head”। Leave करते हो confused, frustrated, invalidated।
But truth यह है: Your anxiety IS literally making you dizzy। And it’s NOT “all in your head”—it’s real, diagnosable medical condition।
What Is This Feeling? “Chakkar” से PPPD तक
Dizziness: Broad Spectrum
“Dizziness” = broad term (light-headedness से stable balance loss तक)। “Vertigo” = specifically spinning sensation। Lekin many people different kind “dizziness” experience करते हैं—”spaced out,” “unsteady,” “floating,” “rocking”।
Distinction important है: True vertigo = spinning। PPPD = unsteadiness, spatial disorientation, instability—लेकिन often WITHOUT spinning।
PPPD: Modern Understanding
PPPD (Persistent Postural-Perceptual Dizziness) = chronic, stress-linked dizziness। Previous labels integrate करता है:
- Phobic Postural Vertigo (PPV) – fear of falling से dizziness
- Chronic Subjective Dizziness (CSD) – persistent dizziness बिना visible vestibular dysfunction
- Space and Motion Discomfort (SMD) – visually complex environments में disorientation
PPPD = chronic functional vestibular disorder। इसका मतलब:
- NOT inner ear में structural defect (hence normal imaging)
- NOT primary psychiatric illness (लेकिन anxiety involve)
- IS change कैसे brain balance information process करता है—”software” problem, NOT “hardware”
PPPD की Diagnostic Criteria
Criterion 1: Duration (3+ Months)
Symptoms = 3 months या उससे ज्यादा सबसे days में present। Acute vertigo (BPPV, neuritis) से अलग, जो weeks में resolve।
Criterion 2: Persistence
Sensation = hours तक लasti है, लेकिन intensity में wax-wane हो सकता है। Chronic, constant—NOT episodic like BPPV attacks।
Criterion 3: Triggers (Hallmark)
Symptoms = तीन categories से triggered:
1. Upright Posture (Standing, Walking)
- Standing = worse than sitting/lying down
- Walking = more than standing still
- Crowds, open spaces, escalators = worse
2. Active or Passive Movement
- Head movements, body rotations
- Riding in car, escalator, elevator
- Motion without control
- Rapid direction changes
3. Complex Visual Stimuli
- Supermarket aisles (many stacked items)
- Malls (crowds, high ceilings, bright lights)
- Traffic, action movies
- Repetitive patterns (stripes, checkered floors)
- Fluorescent lights, scrolling screens
Criterion 4: Inciting Event
Usually कोई triggering event = acute dizziness:
- Vestibular: Ear infection, BPPV, neuritis, migraine vertigo
- Cardiac: Syncope, arrhythmia, BP drop
- Neurological: TIA, seizure, concussion
- Psychological: Panic attack, severe stress, trauma
Most = weeks में recover। Lekin some individuals (especially anxiety-prone) → threat system “on” रहता है → persistent dizziness।
The Science of Link: Anxiety कैसे Balance को Affect करता है
Vestibular-Amygdala Connection
Anatomical pathway:
- Vestibular nuclei (brainstem में) = balance signals का primary processing center
- Direct connections amygdala को (brain’s fear/panic center) = bidirectional
- Abnormal balance signals → amygdala activate → fear response
- Anxiety/panic → vestibular nuclei hyperactive → perceived dizziness
Key insight: Vestibular system isolated नहीं है। Emotional centers से deeply integrated। Balance + fear = neurologically intertwined।
Threat System Overdrive
Balance crisis experience (violent vertigo, fainting, panic) → brain’s threat system = high alert। Adaptive है—protection। Brain learns: “Movement dangerous। Balance unreliable। Vigilant रहो।”
Most people में = alert fades जब ear heal या anxiety resolve। Threat system “stands down”। Brain recalibrate: “Actually, balance fine है।”
Lekin कुछ individuals में (anxious temperament, perfectionism) → threat system “on” रहता है। Result:
- Hyper-vigilance: Constant body position monitoring
- Fear of falling: Even safe surface पर
- Catastrophic thinking: “Slight unsteady = definitely fall”
- Avoidance: Crowds, driving, open spaces avoid
- Positive feedback loop: More avoid = more sensitive threat system। More sensitive = more avoid।
“Closed-Loop” Strategy: Why Efforts Failing
Open-Loop vs. Closed-Loop
Normally: Brain = “open-loop” balance। Automatic, unconscious। Walking without thinking।
Anxiety या balance insult के बाद: Shift to “closed-loop” या “high-demand”। Consciously aware। Stiffening, rigid posture, leg tension। Constantly monitor balance। Scan hazards।
Paradox: Effort = More Instability
Ironically: Increased effort = more unstable।
Consciously managing = sensorimotor mismatch between expected (automatic, fluid) + felt (rigid, controlled)। Mismatch = threat।
Result: Dizziness try prevent करने की कोशिश में stiffening = dizziness create। CORE TRAP।
Visual Vertigo: Modern World की Challenge
Visual Dependency
Vestibular signals perceived unreliable → brain = vision prefer। Result = balance info mostly vision से।
Problem: Visual field fast, complex, unpredictable → visual system can’t keep। Brain: “World moving = I’m moving = balance lose।”
Common Triggers
- Supermarket aisles: Many items, moving people, patterns
- Shopping malls: Open spaces, crowds, lights
- Large-field motion: Traffic, movies, crowds
- Screens: Scrolling, action movies, computer
- Repetitive patterns: Stripes, checkered floors
- Fluorescent lights: Flicker, contrast
- Escalators/elevators: Disorienting motion
Breaking Link: Multi-Step Approach
Pillar 1: Medication (SSRI/SNRI)
NOT vestibular suppressants (जो recovery prevent)। Rather:
SSRIs/SNRIs:
- Paroxetine (Paxil) – 40–
- an SSRI medication (Zoloft) – 50–
- an SNRI medication (Effexor) – 75–
- Escitalopram (Lexapro) – 10–
How: Amygdala’s threat perception lower करते हैं। Brain = fewer false balance alarms।
Timeline: 2–4 weeks benefit, 8–12 weeks max benefit।
Pillar 2: Cognitive Behavioral Therapy (CBT)
How catastrophic thinking = dizziness maintain:
- Slight sway feel
- Think: “Fall जाऊँगा” या “stroke”
- Amygdala activate
- Dizziness perceive more
- More dizziness = thought confirm
- Loop tighten
CBT does:
- Catastrophic thoughts identify
- Distortions challenge करो
- Realistic alternatives develop
- Avoidance reduce (graduated exposure)
- Confidence build
Efficacy: 70–80% improvement with VRT + medication।
Pillar 3: Vestibular Rehabilitation Therapy (VRT)
NOT ear “fix” करना (already fine)। Rather habituate brain to over-monitored signals।
Exercises:
Gaze Stabilization (X1 Viewing):
- Target focus करो
- Head side-to-side move (keep eyes fixed)
- Speed increase gradually
Visual Desensitization (Optokinetic):
- Moving pattern watch
- Follow with eyes
- Reduce visual dependency
Balance Training (Foam, Eyes Closed):
- Unstable surface पर stand
- Eyes close (vision remove)
- Force brain vestibular + proprioceptive use
Gait with Head Turns:
- Walk slow, head side-to-side turn
- Speed increase, pattern change
Duration: 2–3×/day, 4–12 weeks improvement।
Practical Advice
Do’s and Don’ts
DON’T:
❌ Long-term suppressants (prevent recalibration)
❌ Bed rest (worsens deconditioning)
❌ Avoid triggers (reinforces threat)
❌ Focus dizziness पर (hypervigilance)
❌ Catastrophize (perpetuates fear)
DO:
✅ SSRI/SNRI take
✅ Daily movement
✅ Gradually expose triggers
✅ CBT practice
✅ VRT perform (2–3×/day)
✅ Stay active, social
Specific Strategies
1. But Dizziness Diary:
- Date, time, trigger, intensity (1–10), duration
- Associated anxiety? Panic?
- What helped?
2. Relaxation Techniques:
Yoga (3–5×/week, 45–60 min):
- Tree pose, child’s pose, warrior poses
- Breathing (Pranayama)
Tai Chi (4–5×/week, 20–30 min):
- Slow movements + balance challenges
- Meditative, proprioceptive improvement
Breathing (Daily, 5–10 min):
- Inhale 4 counts
- Hold 4 counts
- Exhale 6 counts
- Activates parasympathetic (calming)
3. Exposure Hierarchy:
Create list (1–10 scale):
- Level 1: Phone using seated
- Level 5: Drive quiet road
- Level 10: Mall crowded hours walk
Protocol:
- Start Level 1–2
- 15–30 min spend
- Anxiety peak, reduce होने तक रहो
- 2–3× repeat
- Next level progress
Why: Each success = “threat not real”। Brain recalibrate।
Conclusion
Stress-dizziness link = physical reality, NOT willpower lack। PPPD = functional maladaptation। NOT ear defect, NOT psychiatric illness, NOT “all head में।” Treatable है।
Recovery path:
- Medication = Threat system quiet
- CBT = Reframe thinking, reduce avoidance
- VRT = Habituate vestibular, prove safety
Timeline: 8–12 weeks में 70–80% improvement। 6 months में full recovery।
You’re not crazy। Anxiety = vestibular activate real way। Dizziness = resolved by addressing anxiety + retraining brain + gradually proving movement + life safe।
HINDI VERSION
Your Anxiety Is Literally Making You Dizzy: Stress-Vertigo Link (और इसे Break करो)
Introduction: Scenario जो Lives Change करता है
Scenario = millions को encounter होता है। Crowded supermarket, aisles walk कर रहे हो products से। Suddenly, world “off” feel होता है। Boat पर rock करने जैसा feel, या floating, या tip over होने जैसा—लेकिन कोई actual movement नहीं है। Heart rate accelerate, panic set। Think करते हो “stroke? Heart attack?” Shelf को grab, desperate feel।
या busy motorway पर drive कर रहे हो। Traffic surround। Feeling आता है—spinning sensation नहीं exactly, लेकिन “unsteady,” “spaced out,” या “not quite there” feel। Steering wheel को tight grip।
Months या years के लिए experience किया हो सकता है। Multiple doctors देखे। MRI, hearing tests, vestibular evaluation—सब normal। Doctor कहता है “just stress” या “all in your head”। Leave करते हो confused, frustrated, invalidated।
But truth यह है: Your anxiety IS literally making you dizzy। And it’s NOT “all in your head”—it’s real, diagnosable medical condition।
क्या Is This Feeling? “Chakkar” से PPPD तक
Dizziness: Broad Spectrum
“Dizziness” = broad term (light-headedness से stable balance loss तक)। “Vertigo” = specifically spinning sensation। Lekin many people different kind “dizziness” experience करते हैं—”spaced out,” “unsteady,” “floating,” “rocking”।
Distinction critical है: True vertigo = spinning। PPPD = unsteadiness, spatial disorientation, instability—लेकिन often WITHOUT spinning।
PPPD: Modern Understanding
PPPD (Persistent Postural-Perceptual Dizziness) = chronic, stress-linked dizziness। Previous labels integrate करता है:
- Phobic Postural Vertigo (PPV) – fear of falling से dizziness
- Chronic Subjective Dizziness (CSD) – persistent dizziness बिना visible vestibular dysfunction
- Space and Motion Discomfort (SMD) – visually complex environments में disorientation
PPPD = chronic functional vestibular disorder। इसका मतलब:
- NOT inner ear में structural defect (hence normal imaging)
- NOT primary psychiatric illness (लेकिन anxiety involve है)
- IS change कैसे brain balance information को process करता है—”software” problem, NOT “hardware”।
PPPD की Diagnostic Criteria
Criterion 1: Duration (3+ Months)
Symptoms = 3 months या उससे ज्यादा सबसे दिन present। Acute vertigo (BPPV, neuritis) से अलग, जो weeks में resolve।
Criterion 2: Persistence
Sensation = hours तक last है, लेकिन intensity में wax-wane हो सकता है। Chronic, constant—NOT episodic like BPPV attacks।
Criterion 3: Triggers (Hallmark)
Symptoms = तीन categories से triggered:
1. Upright Posture (Standing, Walking)
- Standing = worse than sitting/lying down
- Walking = more than standing still
- Crowds, open spaces, escalators = worse
2. Active or Passive Movement
- Head movements, body rotations
- Riding in car, escalator, elevator
- Motion without control
- Rapid direction changes
3. Complex Visual Stimuli
- Supermarket aisles (many stacked items)
- Malls (crowds, high ceilings, bright lights)
- Traffic, action movies
- Repetitive patterns (stripes, checkered floors)
- Fluorescent lights, scrolling screens
Criterion 4: Inciting Event
Usually कोई triggering event = acute dizziness:
- Vestibular: Ear infection, BPPV, neuritis, migraine vertigo
- Cardiac: Syncope, arrhythmia, BP drop
- Neurological: TIA, seizure, concussion
- Psychological: Panic attack, severe stress, trauma
Most = weeks में recover। Lekin some individuals (especially anxiety-prone) → threat system “on” रहता है → persistent dizziness।
The Science of Link: Anxiety कैसे Balance को Affect करता है
Vestibular-Amygdala Connection
Anatomical pathway:
- Vestibular nuclei (brainstem में) = balance signals का primary processing center
- Direct connections amygdala को (brain’s fear/panic center) = bidirectional
- Abnormal balance signals → amygdala activate → fear response
- Anxiety/panic → vestibular nuclei hyperactive → perceived dizziness
Key insight: Vestibular system isolated नहीं है। Emotional centers से deeply integrated। Balance + fear = neurologically intertwined।
Threat System Overdrive
Balance crisis experience (violent vertigo, fainting, panic) → brain की threat system = high alert। Adaptive है—protection। Brain सीखता है: “Movement dangerous। Balance unreliable। Vigilant रहो।”
Most people में = alert fades जब ear heal या anxiety resolve। Threat system “stands down”। Brain recalibrate: “Actually, balance ठीक है।”
Lekin कुछ individuals में (anxious temperament, perfectionism) → threat system “on” रहता है। Result:
- Hyper-vigilance: Constant body position monitoring
- Fear of falling: Even safe surface पर
- Catastrophic thinking: “Slight unsteady = definitely fall”
- Avoidance: Crowds, driving, open spaces avoid करना
- Positive feedback loop: More avoid = more sensitive threat system। More sensitive = more avoid।
“Closed-Loop” Strategy: Why Efforts Failing
Open-Loop vs. Closed-Loop
Normally: Brain = “open-loop” balance। Automatic, unconscious। Walking without thinking।
Anxiety या balance insult के बाद: Shift to “closed-loop” या “high-demand”। Consciously aware। Stiffening, rigid posture, leg tension। Constantly monitor balance। Scan hazards।
Paradox: Effort = More Instability
Ironically: Increased effort = more unstable।
Consciously managing = sensorimotor mismatch between expected (automatic, fluid) + felt (rigid, controlled)। Mismatch = threat।
Result: Dizziness try prevent करने की कोशिश में stiffening = dizziness create। CORE TRAP।
Visual Vertigo: Modern World की Challenge
Visual Dependency
Vestibular signals perceived unreliable → brain = vision prefer करता है। Result = balance info mostly vision से।
Problem: Visual field fast, complex, unpredictable → visual system can’t keep। Brain: “World moving = I’m moving = balance lose।”
Common Triggers
- Supermarket aisles: Many items, moving people, patterns
- Shopping malls: Open spaces, crowds, lights
- Large-field motion: Traffic, movies, crowds
- Screens: Scrolling, action movies, computer
- Repetitive patterns: Stripes, checkered floors
- Fluorescent lights: Flicker, contrast
- Escalators/elevators: Disorienting motion
Breaking Link: Multi-Step Approach
Pillar 1: Medication (SSRI/SNRI)
NOT vestibular suppressants (जो recovery prevent)। Rather:
SSRIs/SNRIs:
- Paroxetine (Paxil) – 40–
- an SSRI medication (Zoloft) – 50–
- an SNRI medication (Effexor) – 75–
- Escitalopram (Lexapro) – 10–
How: Amygdala की threat perception को lower करते हैं। Brain = fewer false balance alarms।
Timeline: 2–4 weeks benefit, 8–12 weeks max benefit।
Pillar 2: Cognitive Behavioral Therapy (CBT)
How catastrophic thinking = dizziness maintain:
- Slight sway feel
- Think: “Fall जाऊँगा” या “stroke”
- Amygdala activate
- Dizziness perceive more
- More dizziness = thought confirm
- Loop tighten
CBT does:
- Catastrophic thoughts को identify
- Distortions को challenge करो
- Realistic alternatives develop
- Avoidance को reduce (graduated exposure)
- Confidence build
Efficacy: 70–80% improvement with VRT + medication।
Pillar 3: Vestibular Rehabilitation Therapy (VRT)
NOT ear को “fix” करना (already fine है)। Rather habituate brain को over-monitored signals के साथ।
Exercises:
Gaze Stabilization (X1 Viewing):
- Target को focus करो
- Head को side-to-side move (keep eyes fixed)
- Speed को gradually increase करो
Visual Desensitization (Optokinetic):
- Moving pattern को watch करो
- Follow करो eyes से
- Reduce करो visual dependency
Balance Training (Foam, Eyes Closed):
- Unstable surface पर stand करो
- Eyes को close करो (vision remove)
- Force करो brain को vestibular + proprioceptive use के लिए
Gait with Head Turns:
- Walk करो slow, head को side-to-side turn करो
- Speed को increase करो, pattern change करो
Duration: 2–3×/day, 4–12 weeks improvement।
Practical Advice
Do’s and Don’ts
DON’T:
❌ Long-term suppressants (prevent recalibration)
❌ Bed rest (worsens deconditioning)
❌ Avoid करना triggers (reinforces threat)
❌ Focus करना dizziness पर (hypervigilance)
❌ Catastrophize करना (perpetuates fear)
DO:
✅ SSRI/SNRI लो
✅ Daily movement करो
✅ Gradually expose करो triggers को
✅ CBT practice करो
✅ VRT perform करो (2–3×/day)
✅ Stay करो active, social
Specific Strategies
1. Dizziness Diary:
- Date, time, trigger, intensity (1–10), duration
- Associated anxiety? Panic?
- क्या help किया?
2. Relaxation Techniques:
Yoga (3–5×/week, 45–60 min):
- Tree pose, child’s pose, warrior poses
- Breathing (Pranayama)
Tai Chi (4–5×/week, 20–30 min):
- Slow movements + balance challenges
- Meditative, proprioceptive improvement
Breathing (Daily, 5–10 min):
- Inhale 4 counts
- Hold 4 counts
- Exhale 6 counts
- Activates parasympathetic (calming)
3. Exposure Hierarchy:
Create करो list (1–10 scale):
- Level 1: Phone using seated
- Level 5: Drive quiet road
- Level 10: Mall crowded hours walk
Protocol:
- Start करो Level 1–2 से
- 15–30 min spend करो
- Anxiety peak, reduce होने तक रहो
- 2–3× repeat करो
- Next level पर progress करो
Why: Each success = “threat not real”। Brain recalibrate करता है।
Conclusion
Stress-dizziness link = physical reality, NOT willpower lack। PPPD = functional maladaptation। NOT ear defect, NOT psychiatric illness, NOT “all head में।” Treatable है।
Recovery path:
- Medication = Threat system quiet
- CBT = Reframe thinking, reduce avoidance
- VRT = Habituate vestibular, prove safety
Timeline: 8–12 weeks में 70–80% improvement। 6 months में full recovery।
You’re not crazy। Anxiety = vestibular को literally activate करता है real way में। Dizziness = resolved हो सकता है anxiety को address करके + brain को retrain करके + gradually prove करके movement + life safe है।
PPPD vs. OTHER VESTIBULAR CONDITIONS
(Reference Table – Differential Diagnosis & Treatment Approach)
| Condition | PPPD | BPPV | Vestibular Neuritis | vestibular migraine | Menière’s Disease |
|---|---|---|---|---|---|
| Primary Cause | Functional (threat system overdrive) | Mechanical (crystal displacement) | Viral/inflammatory (vestibular nerve) | Migraine mechanism | Inner ear fluid pressure |
| Structural Abnormality | None (normal imaging) | Crystal in semicircular canal | Nerve inflammation | None | Endolymphatic hydrops |
| Duration of Symptoms | 3+ months, persistent | Minutes–hours, episodic | Days–weeks, constant | 4–72 hours, episodic | Minutes–hours, episodic |
| Type of Vertigo | Unsteadiness, floating, spatial disorientation | Violent spinning | Moderate spinning | Mild–moderate spinning | Severe spinning + tinnitus |
| Nystagmus | Usually none | Characteristic (HSN, ARN, BBN pattern) | Usually present | Sometimes present | May be present |
| Primary Trigger | Upright posture, movement, visual complexity, anxiety | Specific head positions | Viral prodrome | Migraine triggers | Pressure changes, loud sounds, salt |
| Hearing Loss | No | No | Sometimes | Sometimes | YES (hallmark feature) |
| Tinnitus | No | No | No | Sometimes | YES (hallmark feature) |
| Brain Imaging (MRI) | Normal | Normal (unless imaging canal crystals) | Normal or labyrinth enhancement | Normal or brain lesions | Normal (inner ear imaging needed) |
| Vestibular Testing (Caloric, vHIT) | Normal or mild asymmetry | Normal (repositioning test positive) | Abnormal (asymmetry 20–25%+) | Variable | Variable |
| Dix-Hallpike Test | Negative | POSITIVE (diagnostic) | Negative | Negative | Negative |
| HINTS Exam | Normal (peripheral) | Not applicable (BPPV not tested) | Normal (peripheral) | Normal (peripheral) | Normal (peripheral) |
| Typical Patient Age | 20–60 (especially 40–50) | >50 years | 40–50 years | 20–45 years | 40–60 years |
| Anxiety Component | Central feature | Absent (but fear of falling common) | Minimal | Variable | Absent |
| First-Line Treatment | SSRI/SNRI + CBT + VRT | Epley/Semont maneuver | Observation + VRT | Preventative migraine meds | Diuretics + dietary salt restriction |
| Response to Vestibular Suppressants | Poor (blocks recovery) | Not indicated | Unhelpful | Unhelpful | Temporarily helpful during attacks |
| Time to Recovery | 8–12 weeks with treatment | Minutes–hours (Epley cure) | 4–12 weeks | Variable; preventatives help | Variable; chronic |
| Diagnostic Confidence | High (criteria clear) | Very high (Dix-Hallpike) | High (clinical + imaging) | Moderate (clinical diagnosis) | High (hearing loss + vertigo) |
| Prognosis | Excellent (70–80% full recovery) | Excellent (80–90% after maneuver) | Good (80–90% recovery) | Excellent with preventatives | Variable; chronic management |
HOME EXERCISE PROGRAMS (VRT)
(Step-by-Step Protocol for Daily Practice)
Exercise Program Structure
Frequency: 2–3 times per day
Duration: 10–20 minutes per session
Timeline: 4–12 weeks (or until 80%+ symptom improvement)
Progression: Each week, increase repetitions or difficulty
Week 1–2: Foundation Exercises (Begin Here)
Exercise 1A: Gaze Stabilization (X1 Viewing) – Sitting
Purpose: Stabilize eyes during head movement; improve VOR
Setup:
- Sit comfortably
- Hold your thumb or a small object at arm’s length in front of your eyes
- Keep your eyes focused on the object
Execution:
- Move your head slowly side-to-side (left-right rotation)
- Keep your eyes fixed on the object
- Perform 15 repetitions
- Rest 30 seconds
- Repeat 3 sets
Progression: Increase head speed over days
Exercise 1B: Gaze Stabilization (X1 Viewing) – Standing
Setup & Execution: Same as 1A, but standing
Progression from Sitting: Gravity challenge increases; improves balance proprioception
Exercise 2: Postural Stability – Standing on a Firm Surface
Purpose: Improve balance proprioception; reduce reliance on vision
Setup:
- Stand with feet shoulder-width apart
- Keep eyes open, looking ahead
Execution (Progress Through These):
- Week 1: Stand normally, 30 seconds
- Week 2: Feet together, 30 seconds
- Week 3: Tandem stance (heel-to-toe), 30 seconds
- Week 4: Single-leg stance, 30 seconds per leg
Repetitions: 3 sets per variation
Exercise 3: Visual Tracking (Optokinetic Stimulation)
Purpose: Habituate to moving visual field; reduce visual dependency
Setup:
- Watch a moving pattern video (search “optokinetic nystagmus stimulation” on YouTube)
- OR: Watch a scrolling checkerboard or moving dots on screen
Execution:
- Watch the moving pattern for 1–2 minutes
- Follow the pattern with your eyes
- Perform
Progression: Increase speed or pattern complexity over weeks
Week 3–4: Intermediate Exercises
Exercise 4: Balance on Unstable Surface (Foam or Pillow)
Purpose: Force proprioceptive reliance; remove visual dominance
Setup:
- Stand on a foam pad, balance board, or thick pillow
- Eyes open initially
Execution:
- Maintain balance for 30–60 seconds
- Rest 30 seconds
- Repeat 3 sets
Progression:
- Week 3: Eyes open
- Week 4: Eyes closed (removes vision; increases vestibular demand)
- Week 5: Add arm movements while balancing
Exercise 5: Gait Training with Head Turns
Purpose: Integrate head-eye-body coordination; habituate to movement
Setup:
- Clear space for walking (at least 10 feet)
Execution:
- Walk slowly forward
- Turn your head side-to-side while walking
- Walk for 1–2 minutes
- Rest
Repetitions: 3 sessions, 1–2 minutes each
Progression:
- Week 3: Slow walking, slow head turns
- Week 4: Faster walking, faster head turns
- Week 5: Walk in figure-8 pattern while turning head
Exercise 6: Real-World Exposure (Gradual Desensitization)
Purpose: Habituate to triggers in real environments; break avoidance cycle
Setup: Choose a trigger environment (supermarket aisle, shopping mall, etc.)
Execution:
- Spend 15–30 minutes in the environment
- Do NOT leave until anxiety reduces by at least 50%
- This teaches the brain: “I was scared. Nothing bad happened. This is safe.”
Progression:
- Week 1–2: Less busy times (early morning supermarket)
- Week 3–4: Busier times
- Week 5+: More complex environments (malls, driving, crowds)
Week 5–8: Advanced Exercises
Exercise 7: Dynamic Balance – Tandem Stance with Movement
Purpose: Challenge balance system under dynamic conditions
Setup:
- Stand in tandem (heel-to-toe) position
Execution:
- Maintain tandem stance, eyes open, 30 seconds
- Perform arm movements (reaching, crossing) while in tandem
- Perform head turns while in tandem
- Progress to eyes closed
Repetitions: 3 sets, 30 seconds each
Exercise 8: Visual Desensitization – Complex Environments
Purpose: Reduce visual dependency in visually complex settings
Execution:
- Gradually increase time in visually busy environments
- Examples: Scrolling through news feeds, watching action movies, sitting near windows watching traffic
- Duration: Start 30 seconds, progress to 5–10 minutes
Progression: Week 5: 30–60 sec | Week 6: 2–5 min | Week 7–8: 10+ min
Exercise 9: Vestibular-Proprioceptive Integration – Single-Leg Stance Variations
Purpose: Integrate vestibular and proprioceptive systems; advanced balance challenge
Setup:
- Stand on one leg
Execution (Progress Through):
- Week 5: Single-leg, eyes open, 30 seconds
- Week 6: Single-leg, eyes open + arm movements
- Week 7: Single-leg, eyes closed, 30 seconds
- Week 8: Single-leg, eyes closed, on foam pad
Repetitions: 3 sets per variation
Week 9–12: Maintenance & Functional Training
Exercise 10: Real-World Functional Activities
Purpose: Return to normal activities with confidence
Activities:
- Driving: Begin with quiet roads (10 min), progress to busier routes
- Stair climbing: Walk up and down stairs while turning head
- Crowd navigation: Walk through mall or crowded areas (grocery store during busy hours)
- Recreational activities: Return to sports, exercise, hobbies
- Computer/phone use: Gradually increase screen time
Duration: 10–20 minutes daily, as part of normal routine
Maintenance Protocol (After 12 Weeks)
Once symptoms resolve to 80%+ improvement, CONTINUE:
- Daily maintenance: 10–15 minutes of exercises, 5–7 days per week
- Real-world exposure: Continue gradual exposure to triggers
- Relaxation techniques: Daily yoga or breathing (5–10 min)
- Cognitive strategies: Continue CBT techniques; challenge catastrophic thoughts
THE IMPORTANCE OF YOGA
(Physical & Psychological Benefits for PPPD)
Why Yoga Is Vital for PPPD
PPPD involves both physical (vestibular-proprioceptive) and psychological (anxiety, threat system) components. Yoga addresses both simultaneously.
Yoga’s Mechanisms for PPPD Recovery
1. Anxiety Management & Threat System Deactivation
How:
- Yoga activates the parasympathetic nervous system (rest-and-digest), opposing sympathetic activation (fight-or-flight)
- Mindful breathing lowers cortisol (stress hormone) and amygdala reactivity
- Reduces hyper-vigilance to body sensations
Specific practices:
- Pranayama (breathing exercises): Activates parasympathetic; reduces baseline anxiety
- Meditation: Calms amygdala; reduces threat perception
- Savasana (relaxation pose): Complete parasympathetic activation
2. Proprioceptive Awareness & Proprioceptive Retraining
How:
- Yoga requires intense concentration on body position and movement
- Forces proprioceptive system “online” – brain must pay attention to body in space
- Over time, proprioceptive confidence increases, reducing visual dependency
Specific poses:
- Tree pose: Balance challenge; ankle proprioceptors engaged
- Warrior poses (I, II, III): Proprioceptive challenge; stance stability
- Child’s pose: Grounding; vestibular-proprioceptive integration
3. Vestibular System Stimulation
How:
- Head movements, changes in orientation, balance challenges stimulate semicircular canals
- Provides safe, controlled vestibular input
- Promotes central compensation without fear (unlike clinical VRT, which some find anxiety-provoking)
Specific practices:
- Head rolls: Vestibular stimulation; smooth, controlled
- Inverted poses (if comfortable): Anterior canal stimulation
- Balance poses: Active proprioceptive + vestibular engagement
4. Motor Cortex & Cerebellar Health
How:
- Yoga requires complex motor coordination
- Maintains motor cortex plasticity
- Improves cerebellar function (balance, coordination)
- Particularly important in older adults (age-related proprioceptive decline)
Recommended Yoga Practice for PPPD
Style: Hatha, Vinyasa, or Gentle Flow
Frequency: 3–5 times per week
Duration: 45–60 minutes per session
Modifications: Avoid extreme inversion or rapid head movements initially
Sample Beginner Class Structure (45 minutes)
- Centering & Breathing (5 min)
- Seated meditation
- Pranayama (4-count inhale, 4-count hold, 6-count exhale)
- Warm-up (5 min)
- Neck rolls (controlled, slow)
- Shoulder rolls
- Cat-cow stretch
- Standing Poses (20 min)
- Mountain pose (grounding)
- Tree pose (balance)
- Warrior I, II, III (proprioceptive challenge)
- Triangle pose (stretch, proprioceptive awareness)
- Balance Challenges (5 min)
- Single-leg variations
- Eyes-closed modifications
- Relaxation (10 min)
- Child’s pose
- Corpse pose (Savasana)
- Final breathing
ARTICLES #6 & #7: detailed FAQs
>
Complete FAQ Section for Missing Content
📋 ARTICLE #6: ANXIETY IS LITERALLY MAKING YOU DIZZY – COMPLETE FAQS (60 QUESTIONS)
ENGLISH FAQs (20 Questions)
1. What is PPPD (Persistent Postural-Perceptual Dizziness)?
PPPD is a functional disorder where the brain’s balance filters become hypersensitive due to anxiety or prior balance trauma. Unlike BPPV (true spinning), PPPD involves a “software” problem in the brain—the balance system is physically normal but the brain misinterprets normal motion as a threat. Typical presentation: chronic unsteadiness, floating sensation, or spatial disorientation (NOT spinning). Diagnostic criteria: 3+ months symptoms, triggered by upright posture/movement/visual complexity. PPPD responds excellently to SSRI medication (paroxetine 40–), CBT (8–12 weeks), and VRT exercises (2–3×/day). Recovery rate: 70–80% improvement with combined treatment.
2. How are anxiety and dizziness connected neurologically?
The vestibular system (inner ear balance centers) connects directly to the amygdala (brain’s fear/threat center). When severe vertigo or panic occurs, the threat system activates—an adaptive response. In most people, this alert fades as the ear heals. In anxiety-prone individuals, the threat system REMAINS “ON,” creating a feedback loop: Anxiety → triggers vestibular sensitivity → perceived dizziness → more anxiety. This is NOT psychological weakness; it’s a real neurobiological connection between the vestibular-amygdala axis. The connection can be recalibrated with proper treatment.
3. What are the four diagnostic criteria for PPPD?
(1) Duration: Symptoms present 3+ months on most days (distinguishes PPPD from acute vertigo). (2) Persistence: Sensations last hours at a time, though intensity may fluctuate. (3) Triggers: Symptoms triggered by (a) upright posture (standing/walking worse than lying down), (b) active/passive movement, or (c) complex visual stimuli (supermarket aisles, traffic, moving patterns, fluorescent lights). (4) Inciting Event: Usually triggered by medical event (inner ear infection, BPPV, vestibular neuritis, cardiac syncope, TIA, or acute psychological distress). Normal imaging (MRI, hearing tests) confirms functional (NOT structural) disorder.
4. Why does PPPD cause “visual vertigo” and visual dependency?
In PPPD, vestibular signals are perceived as unreliable (even though structurally normal), so the brain shifts balance preference to VISION. This creates “visual dependency”—dizziness triggered by complex visual environments. Triggers: supermarket aisles (stacked items), shopping malls (crowds + high ceilings + lights), traffic, action movies, scrolling phones, fluorescent lights, repetitive patterns (stripes, checkered floors). The visual system cannot process this conflicting information fast enough, and the brain perceives motion conflict, triggering dizziness. Visual desensitization therapy (gradual, repeated exposure to moving scenes) significantly improves this over 4–8 weeks.
5. What is the “closed-loop” strategy and why does it worsen PPPD?
Normally, balance is AUTOMATIC (open-loop)—you walk without thinking about it. In PPPD, patients consciously MONITOR balance (closed-loop), stiffening posture and co-contracting muscles to feel “stable.” This paradoxically creates a SENSORIMOTOR MISMATCH between expected (automatic, fluid movement) and felt (rigid, controlled movement). The brain interprets this mismatch as a threat, INCREASING dizziness. The more patients try to “control” balance through stiffening, the WORSE symptoms become. Treatment involves relearning automatic balance through gradual exposure and reducing hypervigilance—allowing the cerebellum to regain automatic control.
6. What medications are most effective for treating PPPD?
SSRIs/SNRIs are first-line: Paroxetine (40–, strongest evidence for PPPD), an SSRI medication (50–), an SNRI medication (75–), escitalopram (10–). These raise the brain’s threshold for threat detection by increasing serotonin availability in the amygdala and vestibular nuclei. Timeline: Benefits appear 2–4 weeks, maximal benefit 8–12 weeks. AVOID: Vestibular suppressants (a vestibular suppressant, scopolamine, a vestibular suppressant) for PPPD—they block central compensation and worsen long-term outcomes. SSRI dosing should be individualized; side effects typically include initial nausea (usually resolves) and sexual dysfunction (discuss alternatives with doctor). Medication alone is insufficient; must combine with CBT and VRT.
7. How does Cognitive Behavioral Therapy (CBT) help PPPD patients?
CBT addresses catastrophic thinking patterns that maintain PPPD. Mechanism: (1) Identify catastrophic thoughts (“I’m going to fall,” “I’ll never be normal”); (2) Challenge accuracy using evidence; (3) Develop realistic alternatives (“I felt unsteady, but nothing happened”); (4) Graduated exposure—gradually entering “scary” situations to prove threat is not real. Each successful exposure teaches the brain: “I was afraid X would happen. X didn’t happen. The threat is not real.” Over 8–12 weeks, repeated exposures recalibrate the threat system. CBT also reduces avoidance behavior—the #1 maintainer of PPPD. Efficacy: 70–80% improvement when combined with VRT + medication.
8. What is Vestibular Rehabilitation Therapy (VRT) for PPPD and how does it differ from VRT for BPPV?
VRT for PPPD is NOT about “fixing” the ear (already normal). Instead, it teaches the BRAIN to HABITUATE to dizziness-provoking signals. Exercises: (1) Gaze stabilization (X1 viewing): Head moving, eyes fixed on target; (2) Visual desensitization: Watch moving patterns to reduce visual dependency; (3) Balance training on unstable surfaces: Force brain to use non-visual cues; (4) Gait training with head turns: Integrate movement while head moving; (5) Real-world exposure: Supermarkets, malls, driving—controlled exposure to actual triggers. Performed 2–3×/day, VRT achieves 60–80% improvement over 8–12 weeks. Unlike BPPV (specific cure—Epley maneuver), PPPD recovery requires sustained practice and neural recalibration.
9. Why is bed rest and avoidance harmful in PPPD recovery?
Bed rest and avoidance (staying home, avoiding crowds) ALLOW the threat system to become MORE sensitive. Neurobiological mechanism: Each time patient avoids a trigger, the brain REINFORCES the threat perception (“Crowds are dangerous—must avoid”). This creates a vicious cycle: More avoidance → More sensitivity → More avoidance. In severe cases, leads to agoraphobia (inability to leave home). Recovery REQUIRES the OPPOSITE: Gradual, repeated exposure to feared situations to reprogram the brain. Each successful exposure (nothing bad happened) weakens the threat association. Avoidance is the #1 ENEMY of PPPD recovery—yet most patients’ first instinct is to avoid.
10. What is the typical timeline for PPPD recovery with combined treatment?
With combined treatment (SSRI + CBT + VRT): 8–12 weeks = 70–80% symptomatic improvement; 6 months = full functional recovery. Untreated PPPD: Can persist for years, often progressing to agoraphobia. Timeline depends on: (1) Treatment adherence (skipping sessions delays recovery), (2) Severity at diagnosis (mild cases recover faster), (3) Individual neuroplasticity (varies person-to-person). Some patients notice benefits within 2–4 weeks of starting SSRI + VRT; others require 3–4 months. Consistency is KEY—daily exercises more important than intense occasional sessions. Post-recovery: Daily 10–15 min maintenance exercises prevent relapse.
11. What is the role of yoga in PPPD recovery and how often should it be practiced?
Yoga addresses both physical (vestibular-proprioceptive) AND psychological (anxiety, threat system) components. Mechanisms: (1) Anxiety reduction: Activates parasympathetic nervous system, lowers cortisol, reduces amygdala reactivity; (2) Proprioceptive training: Improves body awareness, confidence, reduces hypervigilance; (3) Vestibular stimulation: Balance poses (tree, warrior) gently stimulate vestibular system without triggering fear; (4) Motor cortex health: Maintains plasticity, particularly important in aging; (5) Mindfulness: Reduces catastrophic thinking. Recommended: 3–5 times weekly (45–60 minutes). Particularly helpful for patients anxious about clinical VRT. Specific poses: Tree pose (balance), warrior poses (proprioceptive challenge), child’s pose (calming), pranayama (breathing—activates parasympathetic). Yoga + medication + VRT = detailed approach.
12. Can PPPD be can provide long-term relief for, or will it recur?
PPPD is a REVERSIBLE, FUNCTIONAL disorder—NOT a progressive disease. With proper treatment, 80–100% recovery is achievable and sustainable. “Cure” means the brain has RECALIBRATED, not that the condition can significantly less likely to recur. However: Risk of mild symptom recurrence if severely stressed (especially if treatment discontinued). Full relapse is uncommon because the brain retains learned adaptations (like riding a bike—once learned, recovery is faster). Prevention of relapse: Continue daily maintenance exercises (10–15 min), manage stress, maintain social engagement, continue medication 6–12 months as recommended. Most recovered patients remain symptom-free long-term with basic maintenance.
13. What is the difference between PPPD and panic disorder, and how are they treated differently?
PPPD: Vestibular dysfunction; primary problem = balance system dysregulation; triggers = postural/visual (standing, supermarkets); treats as vestibular condition. Panic Disorder: Psychiatric condition; primary problem = anxiety dysregulation; triggers = situational (crowds, enclosed spaces); treats as psychiatric condition. Overlap: PPPD patients often develop panic attacks TRIGGERED by dizziness (fear of falling); panic patients may experience vestibular symptoms (dizziness during panic). Treatment differs: PPPD = VRT + vestibular-specific medication (SSRIs for vestibular stabilization) + CBT for catastrophic thinking about balance; Panic = psychiatric therapy + SSRIs for panic + CBT for anxiety. Many patients have BOTH requiring coordinated care (ENT + psychiatry). Untreated PPPD can evolve into panic disorder if threat system remains hyperactive.
14. Why do some people develop PPPD after BPPV while others recover fully?
BPPV can trigger PPPD in susceptible individuals (anxious temperament, perfectionism, prior anxiety/trauma history). Theory: Severe BPPV triggers intense fear, activating threat system. In most people, threat alert FADES as inner ear heals (benign situation—just faulty crystals, easily fixed). In anxiety-prone individuals, threat system remains “ON,” leading to persistent dizziness even after ear heals—PPPD. Protective factors: Early reassurance (“This is BPPV, 90% cured with one maneuver”), successful Epley maneuver, positive reinforcement (“You fixed it—ear works now”). Risk factors: Catastrophizing (“This will never go away”), prolonged avoidance, reassurance-seeking. This explains why some BPPV patients recover fully after one Epley, others develop chronic dizziness. Personality and early psychological management are important.
15. What typically triggers PPPD flare-ups during recovery and how long do they last?
Common triggers: (1) High stress or major life changes; (2) Sleep deprivation; (3) Caffeine or alcohol excess; (4) Skipping VRT exercises; (5) Returning to avoidance behaviors; (6) Relapse in catastrophic thinking; (7) New sensory challenges (flying, highway driving); (8) Medication changes. Duration: Flare-ups are TEMPORARY—typically 24–72 hours if properly managed. Importantly: Flare-ups do NOT indicate treatment failure or disease recurrence. Rather, they indicate the brain needs REINFORCEMENT of coping strategies. Management: Increase VRT frequency, renew CBT techniques, manage stress actively, maintain exercise, avoid medication escalation (which delays recovery). Most flare-ups resolve within days with proper response.
16. How do you differentiate PPPD from BPPV from vestibular migraine based on symptom presentation?
PPPD: 3+ months chronic, triggered by upright posture/movement/visual complexity, normal imaging, associated with anxiety/prior balance event, no true spinning. BPPV: Episodic (minutes–hours, NOT hours continuously), triggered by specific head positions (Dix-Hallpike positive in 90–95%), normal between attacks, violent spinning, often resolved after one Epley maneuver. Migraine: 4–72 hour episodes, associated with headache/photophobia/phonophobia/nausea, triggers include diet (chocolate, aged cheese), stress, hormones, sleep changes, often unilateral. Definitive diagnosis requires specialist evaluation: HINTS exam (rules out central), Dix-Hallpike test (BPPV), audiometry (Menière’s vs others), MRI (rules out pathology). Many patients have MULTIPLE conditions requiring different treatments.
17. What is the “72-hour rule” for vestibular suppressants and does it apply to SSRIs in PPPD?
72-hour rule: Applies to VESTIBULAR SUPPRESSANTS (a vestibular suppressant, benzodiazepines, scopolamine), NOT SSRIs. Suppressants should be used MAXIMUM 1–3 days because they chemically “block” the vestibular system, preventing the BRAIN from adapting (central compensation). Longer use = brain stops trying to compensate = when medication stops = vestibular system WEAKER (not stronger). Paradoxical outcome: Longer medication use = WORSE long-term outcomes. Some patients become CHRONICALLY dependent—medication-induced chronic motion sickness (tragic). SSRIs are DIFFERENT: Can be used LONG-TERM (6–12 months minimum) during PPPD treatment because they don’t suppress recovery—they lower the threat threshold, ALLOWING recovery to occur. SSRI mechanism is rehabilitative, not suppressive. Always consult doctor before stopping any medication.
18. Can PPPD patients travel safely by airplane or car, and how should they prepare?
YES, with preparation. Pre-travel protocol (7–10 days before): (1) VRT exercises: Daily X1 viewing + head movements; (2) Visual desensitization: Watch moving scenes from windows, progressively increase duration (start 15 sec, work up to 5+ min); (3) Anxiety management: Relaxation techniques, SSRI if prescribed (don’t start day before—already at steady state); (4) Confidence building: Short car trips before long journeys. During travel: Sit in front seat, fixate on horizon (NOT dashboard or close objects), avoid phone scrolling, use neck pillow for head support, maintain slow, controlled head movements. Pharmacology: Scopolamine patch (24–48 hours of protection) if needed, but gradual habituation safer long-term than medication-dependent approach. Most PPPD patients fly/drive successfully post-treatment.
19. What should family members and close contacts know about supporting a PPPD patient?
Key support strategies: (1) Validate symptoms—they are REAL. Not “in the patient’s head” (this is a real neurobiological condition). (2) Encourage exposure, not avoidance. “Let’s go to the mall” is therapeutic; “Stay home” is harmful. (3) Support medication/therapy compliance. Attend appointments if possible, remind about daily exercises. (4) Avoid catastrophizing language. Don’t say “You’ll never get better” (untrue—80–100% recovery possible). (5) Practice patience. Recovery takes 2–6 months, not days. (6) Learn about PPPD. Understanding the condition helps provide appropriate support. (7) Encourage exercise + social engagement. Isolation worsens outcomes; activity accelerates recovery. (8) Be consistent. Family who reinforce recovery strategies improve outcomes dramatically. Family involvement significantly improves recovery rates—isolation predicts poor outcomes.
20. What are the red flags that require immediate specialist referral in PPPD?
Seek urgent ENT/neurology evaluation if: (1) Symptoms WORSEN despite 3+ months of proper medication + VRT (suggests alternative diagnosis or treatment adjustment needed); (2) New onset vertigo with ABNORMAL HINTS exam (suggests central cause—stroke—requires urgent MRI); (3) Severe disability affecting work/relationships after 3 months treatment (may need increased medication dose or psychiatric referral); (4) Associated neurological symptoms (weakness, speech changes, vision loss, facial drooping) (suggests central pathology); (5) Hearing loss developing WITH dizziness (suggests inner ear pathology—Menière’s vs other); (6) Severe psychiatric comorbidity (depression, suicidality) requiring mental health hospitalization. Note: Most PPPD responds excellently to first-line treatment (SSRI + CBT + VRT). Red flags indicate either alternative diagnosis or need for treatment intensification. Early specialist involvement (ENT + psychiatry) optimizes outcomes.
HINGLISH FAQs (20 Questions)
1. PPPD kya है?
PPPD = Persistent Postural-Perceptual Dizziness = brain के balance filters hypersensitive हो जाते हैं anxiety या prior balance trauma से। यह NOT true spinning (BPPV) है; यह “software” problem है brain का। Unsteadiness, floating, spatial disorientation feel होता है—NOT spinning। Normal imaging लेकिन chronic dizziness। SSRI medication (paroxetine 40–) + CBT (8–12 weeks) + VRT (2–3×/day exercises) = 70–80% improvement।
2. Anxiety aur dizziness का neurological connection?
Vestibular system (inner ear) = directly connected = amygdala को (fear center)। Severe vertigo होने पर = threat system activate होता है। Most people में fade होता है; anxiety-prone individuals में “on” रहता है = feedback loop = Anxiety → dizziness → more anxiety। Biological connection है, psychological नहीं।
3. PPPD की four diagnostic criteria?
(1) Duration: 3+ महीने daily symptoms। (2) Persistence: Sensations hours लम्बे। (3) Triggers: Upright posture (standing/walking), movement, complex visuals (supermarket, traffic, lights)। (4) Inciting event: Prior ear infection, BPPV, vestibular neuritis, panic, या trauma।
4. Visual vertigo कैसे develop होता है?
Brain vestibular signals को unreliable think करता है, तो vision prefer करता है। “Visual dependency” बन जाता है। Supermarket aisles, malls, traffic, phone scrolling, movies, lights = triggers। Visual system overwhelmed होता है। Visual desensitization therapy = 4–8 weeks में improve।
5. “Closed-loop” strategy क्या है?
Normally = automatic balance। PPPD में = conscious monitoring, stiffening = sensorimotor mismatch बनता है = brain को threat लगता है = WORSE dizziness। Stiffening = vicious cycle। Treatment = relearn automatic balance through exposure।
6. PPPD के लिए कौन medicines काम करती हैं?
SSRIs/SNRIs = paroxetine (40–), an SSRI medication (50–), an SNRI medication (75–)। Benefits = 2–4 weeks, max = 8–12 weeks। Vestibular suppressants AVOID करो। SSRI + CBT + VRT = combination essential।
7. CBT PPPD में कैसे मदद करता है?
Catastrophic thinking patterns = address होती हैं। Challenge करते हो false thoughts, graduated exposure करते हो feared situations को = prove करते हो threat नहीं है। 8–12 weeks में brain recalibrate होता है।
8. VRT (Vestibular Rehabilitation) PPPD में कैसे काम करता है?
NOT ear fix करना (already normal)। Brain को habituate करना है। Exercises = X1 viewing, visual desensitization, balance training, gait training, real-world exposure। 2–3×/day = 60–80% improvement।
9. Bed rest aur avoidance PPPD में harmful क्यों?
Rest + avoidance = threat system MORE sensitive बनाता है। Each avoidance = brain को reinforce करता है (“dangerous, avoid”)। Cycle worse होता जाता है। Recovery = OPPOSITE = gradual exposure। Avoidance = #1 enemy।
10. PPPD recovery कितना time लेता है?
Treatment के साथ = 8–12 weeks में 70–80% improvement; 6 महीने = full recovery। Untreated = साल लग सकते हैं। Consistency = KEY। Daily maintenance post-recovery = relapse prevent।
11. Yoga PPPD में क्या role खेलता है?
Anxiety reduction (parasympathetic activation), proprioceptive training, vestibular stimulation, motor health, mindfulness। 3–5×/week (45–60 min) = recommended। Anxiety-prone patients के लिए helpful।
12. PPPD can provide long-term relief for हो सकता है?
YES, functional reversible condition है। 80–100% recovery possible है। Cure = brain recalibrated। Relapse rare है if maintenance continue करते हो।
13. PPPD aur panic disorder में difference?
PPPD = vestibular dysfunction; panic = psychiatric। Triggers different। Treatment different। Coordinated care (ENT + psychiatry) = needed।
14. BPPV के बाद कुछ लोग PPPD develop क्यों करते हैं?
Susceptible individuals में = brain threat system hyperactive हो जाता है। Most में fade होता है; anxiety-prone में persist होता है।
15. PPPD flare-ups का trigger क्या?
Stress, sleep loss, caffeine, skipped exercises, avoidance, catastrophic thinking, new challenges (flying, highway)। Temporary होते हैं, reinforce करना पड़ता है।
16. PPPD vs BPPV vs migraine को कैसे differentiate करो?
PPPD = chronic 3+ months, postural/visual triggers, anxiety। BPPV = episodic, position-triggered। Migraine = 4–72 hours, headache/triggers। Specialist consultation = needed।
17. “72-hour rule” क्या है PPPD में?
Suppressants = max 1–3 days (longer use = blocks recovery)। SSRIs = long-term ok।
18. PPPD patient plane या car में travel कर सकता है?
YES, with preparation। Pre-travel VRT, visual desensitization, anxiety management। During = front seat, horizon fixate, head support।
19. Family members PPPD patient को कैसे support करें?
Validate, encourage exposure, support compliance, avoid catastrophizing, patience, learn, encourage activity, consistent support।
20. Red flags हैं specialist referral के लिए?
Worsening despite treatment, abnormal HINTS, severe disability, neurological symptoms, hearing loss + dizziness, psychiatric crisis।
HINDI FAQs (20 Questions)
1. पीपीपीडी (PPPD) क्या होता है?
पीपीपीडी = एक कार्यात्मक विकार = मस्तिष्क के balance filters चिंता या पूर्व balance trauma से hypersensitive हो जाते हैं। यह true spinning (BPPV) नहीं है; यह brain की “software” समस्या है। Inner ear physically सामान्य है, लेकिन मस्तिष्क सामान्य गति पर over-react करता है। लक्षण: unsteadiness, floating, spatial disorientation। Treatment: SSRI (paroxetine 40–) + CBT + VRT = 70–80% सुधार।
2. चिंता और चक्कर का तंत्रिका विज्ञान संबंध?
Vestibular system (inner ear) = सीधे amygdala (fear center) से जुड़ा है। गंभीर vertigo = threat system activate। अधिकांश में fade होता है; anxiety-prone individuals में “on” रहता है = feedback loop। Biological connection है, psychological नहीं।
📞 PRIME ENT CENTER CONTACT INFORMATION
Dr. Prateek Porwal, ENT & Vertigo Specialist | MBBS, DNB ENT, CAMVD | Prime ENT Center, Hardoi
PRIME ENT Center
Clinic Location:
Nagheta Road, Near Income Tax Office
Jindpeer Chauraha, Hardoi
Uttar Pradesh 241001, India
Contact Details:
- Phone: +91 73930 62200
- Email: primeenthdi@gmail.com
- Website: https://primeentcenter.in
Consultation Timings:
- Monday to Saturday: 11:00 AM–04:00 PM | 06:00 PM–08:00 PM
- Sunday: Closed
- Emergency Services: Available through main contact number
Why Choose PRIME ENT Center for PPPD & Anxiety-Related Dizziness?
✓ detailed PPPD Assessment – Diagnosis based on diagnostic criteria + differential exclusion of structural causes
✓ Medication Management Expertise – Safe SSRI/SNRI initiation, monitoring, dosage optimization
✓ Coordinated Multidisciplinary Care – Direct referrals to CBT therapists and VRT specialists
✓ Evidence-Based VRT – In-coordination with qualified physical therapists; home exercise protocol guidance
✓ Vestibular-Specific Evaluation – HINTS exam, caloric testing, vestibular function assessment to confirm peripheral vs. central
✓ 3-Language Patient Education – English, Hindi, Hinglish counseling; patient handouts; anxiety-dizziness education
✓ complete Approach – Addresses medical, physical, and psychological dimensions of PPPD
✓ Ongoing Monitoring – Regular follow-ups during SSRI tapering, VRT progression, recovery phases
Book Your Consultation Today
For PPPD evaluation, anxiety-dizziness assessment, or multidisciplinary care coordination:
📱 Call: +91 73930 62200
💬 WhatsApp: +91 73930 62200
📧 Email: primeenthdi@gmail.com
🌐 Website: https://primeentcenter.in
What to Bring to Your PPPD Consultation
- Symptom diary: Document triggers, duration, associated anxiety (2+ weeks ideal)
- Previous imaging: Any MRI, CT, or hearing test results (confirm normal findings)
- Medication list: Current and past medications, including anxiety or vestibular medications
- Mental health history: Prior anxiety, panic, trauma, depression (not mandatory but helpful)
- Questions about: SSRI vs. other treatments, CBT availability, VRT options, timelines
- Insurance information: For mental health referral coordination
About Dr. Prateek Porwal
Dr. Prateek Porwal is a board-certified ENT specialist with advanced expertise in vestibular disorders, functional dizziness, and the neurobiological links between anxiety and balance. With over 13+ years of clinical experience and specialized training in neuro-otology, Dr. Porwal integrates medical, psychological, and rehabilitative approaches to PPPD, achieving high rates of patient recovery and satisfaction.
His philosophy: PPPD is real, treatable, and recovery is achievable through a compassionate, evidence-based approach that addresses the whole patient—not just the symptoms.
Medical Disclaimer: This article is for educational purposes only. It does not constitute medical advice or prescribing guidance. All medications mentioned should only be taken under the direct supervision of a qualified physician. Specific doses, durations, and drug choices depend on your individual clinical condition and must be determined by your treating doctor. If you experience severe symptoms, please seek immediate medical attention.
Break the anxiety-dizziness cycle. Reclaim your life. PRIME ENT Center is here to help.
References
- Staab JP, et al. Diagnostic criteria for persistent postural-perceptual dizziness (PPPD). Journal of Vestibular Research. 2017;27(4):191–208.
- Edelman S, Mahoney AEJ, Cremer PD. Cognitive behavior therapy for chronic subjective dizziness. American Journal of Otolaryngology. 2012;33(4):395–401.
