The cervical vertigo misdiagnosis neck x-ray trap is one of the most common diagnostic errors in clinical medicine—affecting thousands of patients annually. This comprehensive guide exposes how imaging findings mislead practitioners and patients, preventing proper treatment.
- Main trap: Cervical spondylosis (bone spurs, disc space narrowing) on X-rays is INCIDENTAL and usually NOT the cause of vertigo
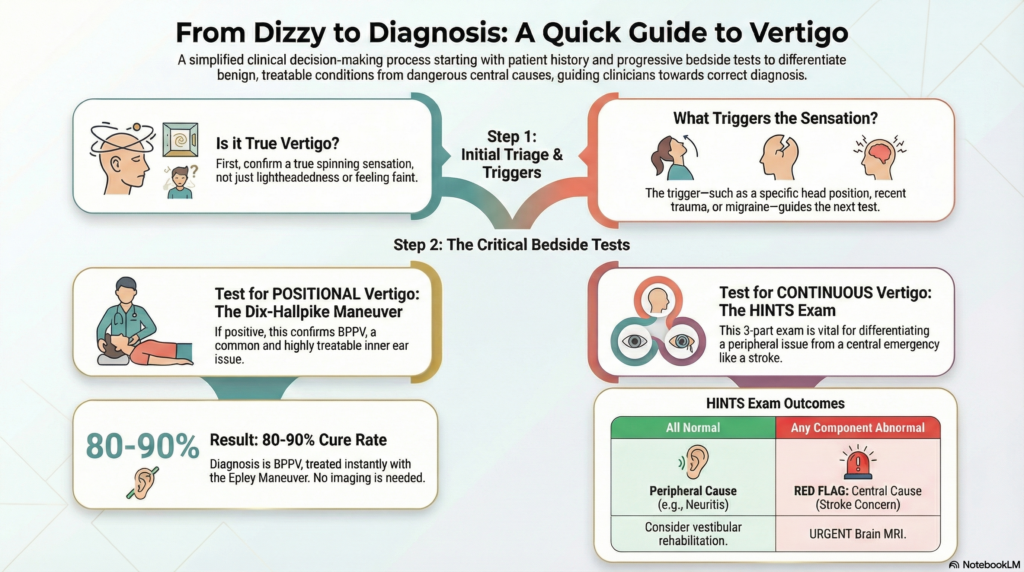
- Most common misdiagnosed cause: BPPV (Benign Paroxysmal Positional Vertigo)—displaced inner ear crystals, NOT a neck problem
- Gold standard test: Dix-Hallpike maneuver (90–95% sensitivity; bedside; FREE; diagnostic AND therapeutic)
- Time to cure: 80–90% of BPPV cases cured within MINUTES with Epley maneuver
- Why imaging misleads: Neck X-rays/CT show bone spurs (incidental in 70–80% of elderly) but CANNOT explain spinning sensation
- Red flag for emergency: Abnormal HINTS exam (3-minute eye movement test) suggests central cause (stroke)—needs MRI urgently
- Action plan: If told you have “cervical vertigo,” request Dix-Hallpike test; if positive, ask for Epley maneuver IMMEDIATELY
ENGLISH VERSION
The Cervical Misdiagnosis Trap: How Neck X-Rays Are Killing Your Vertigo Treatment
Introduction: The Trap That Snares Millions
When a patient complains of “chakkar” (spinning), dizziness, or vertigo, the immediate instinct of many clinicians is to look at the neck. This approach is intuitive, visible, and supported by readily available imaging. Yet it is fundamentally flawed.
The result is a series of neck X-rays or CT scans that reveal age-related wear and tear—spondylosis, osteophytes, disc space narrowing—findings that seem to “explain” the spinning. However, “cervical vertigo” remains one of the most controversial and poorly defined diagnoses in clinical medicine. For many patients, focusing on the neck is a diagnostic trap that leads to years of ineffective treatment—neck collars, unnecessary surgery, anti-inflammatory medications—while the actual, treatable cause of their vertigo (usually located in the inner ear) goes ignored.
This article exposes the cervical misdiagnosis trap and provides you with the knowledge to escape it.
The Myth of the “Bad Neck”
Why Head Movement ≠ Neck Problem
The belief that neck problems cause vertigo is widespread because most patients feel dizzy when they move their heads. This observation seems logically sound: “When I turn my head, I feel spinning. Therefore, my neck causes my vertigo.”
However, this reasoning overlooks a fundamental truth about the vestibular system.
The vestibular system is, by design, a head-movement detection system. The semicircular canals in the inner ear sense rotational acceleration of the head. The utricle and saccule sense linear acceleration and gravity. All of these structures are optimized to detect and report head movements to the brain.
Critically: all head movements must involve neck movement. You cannot rotate your head left or right without rotating your cervical spine. You cannot flex or extend your head without moving your neck. The neck is simply the mechanical link that allows the head to move.
Therefore, any primary vestibular disorder will naturally become more symptomatic when the head moves because head movement is what activates the vestibular system.
This creates a false correlation:
- Patient moves head → patient feels vertigo → patient (and doctor) assume neck is the cause
- X-ray shows cervical spondylosis → diagnosis seems “confirmed”
In reality, the spondylosis is an incidental finding—a normal part of aging in adults over 50—with no causal relationship to the vertigo.
The Evidence: Spondylosis Is Ubiquitous and Usually Innocent
Studies of asymptomatic adults show:
- 70–80% of adults over age 70 have cervical spondylosis on imaging
- 30–40% of adults in their 50s have radiographic changes
- Most of these individuals have no neck pain or vertigo whatsoever
If cervical spondylosis caused vertigo, we would expect an epidemic of spinning among the elderly. Instead, spondylosis is incidental, and the true causes of vertigo (BPPV, vestibular neuritis, central causes) occur independently of cervical degeneration.
BPPV and Cervical Vertigo Misdiagnosis Neck X-Ray Confusion
Why BPPV Looks Like a Neck Problem
BPPV (Benign Paroxysmal Positional Vertigo) is the most common cause of recurrent vertigo in adults, accounting for 20–40% of all vertigo cases. It is also the most frequent generator of the “cervical vertigo trap.”
How BPPV occurs:
- Tiny calcium carbonate crystals (otoconia), normally embedded in the utricle of the inner ear, dislodge
- These crystals migrate into one of the three semicircular canals
- When the head moves in certain directions, the loose crystals shift within the canal, causing false signals of rotation
- The brain perceives violent spinning vertigo (nystagmus is often visible)
Why BPPV mimics a neck problem:
- BPPV is triggered by lying down (moving the head into horizontal extension)
- BPPV is triggered by rolling in bed (head rotation combined with neck extension)
- BPPV is triggered by looking up (cervical extension)
- BPPV is triggered by turning the head side-to-side (cervical rotation)
All of these movements involve the neck. To an untrained observer, it appears obvious that neck movement triggers the spinning, therefore the neck must be the problem.
The Misdiagnosis Cascade
A typical patient journey:
- Patient experiences sudden spinning when rolling in bed (this is BPPV)
- Patient or family attributes it to the “bad neck” (false reasoning)
- Patient gets neck X-rays (revealing age-related spondylosis, which is incidental)
- Doctor diagnoses “cervical vertigo” or “vertebrobasilar insufficiency”
- Patient is prescribed neck stretches, physical therapy focused on neck mobility, possibly a neck collar
- Patient’s symptoms persist (because BPPV hasn’t been treated)
- Patient undergoes weeks or months of futile treatment while suffering needlessly
- Eventually (if lucky), patient sees a vestibular specialist who performs a simple Dix-Hallpike test, which is positive
- Patient receives the Epley maneuver—a simple physical repositioning—and is cured within minutes
The lost opportunity: If the Dix-Hallpike test had been performed on Day 1, the diagnosis would have been made and the patient cured in under 5 minutes.
Why X-Rays Are Fundamentally Misleading
X-Rays Show Bone, Not Function
The core problem is that X-rays show anatomy (bone structure) but not function (nerve activity, blood flow, vestibular mechanics). A normal X-ray cannot prove the neck is healthy; an abnormal X-ray cannot prove the neck caused the vertigo.
Three Critical Misunderstandings
1. Spondylosis Occurs at C4–C7; Rotation Occurs at C1–C2
Many clinicians assume that if cervical degeneration exists, it must explain cervical problems. This is anatomically incorrect.
C4–C7 vertebrae: These lower cervical vertebrae primarily allow flexion and extension (nodding movements). Degenerative changes here narrow disc spaces and may cause compression of nerve roots, but these changes do not directly affect the semicircular canals or vestibular nuclei.
C1–C2 (Atlantoaxial articulation): This is where most head rotation (left-to-right movement) occurs. Degeneration at C1–C2 is less common than lower cervical spondylosis. However, even significant C1–C2 degeneration does not directly cause the mechanical failure of the vestibular system that produces true vertigo.
The disconnect: Even if a patient has severe C4–C7 spondylosis, it does not mechanically explain the sensation of the room spinning.
2. Vertigo Indicates a Problem in the Semicircular Canals or Central Connections, Not the Spine
Vertigo is a hallucination of movement—the illusion that the world is spinning when it is not, or that your body is spinning when it is not. This perceptual error almost always indicates:
- A mechanical problem in the semicircular canals (BPPV, AICA stroke affecting the labyrinth)
- A viral or inflammatory problem in the vestibular nerve (vestibular neuritis)
- A central neurological problem affecting the vestibular nuclei in the brainstem (stroke, multiple sclerosis, tumor)
Bone spurs in the lower cervical spine do not mechanically disrupt any of these structures. A bone spur cannot dislodge otoconia, cannot infect the vestibular nerve, cannot damage the vestibular nuclei.
3. “Red Herrings” Are Common in Aging Patients
The elderly often have multiple simultaneous findings:
- Asymptomatic cervical spondylosis (extremely common)
- Mild orthostatic hypotension (blood pressure drop when standing)
- Presbycusis (age-related hearing loss)
- Mild gait ataxia from other causes (neuropathy, sarcopenia)
When an elderly patient complains of dizziness, the temptation is to attribute it to the most visible finding on imaging (the spondylosis). This is a cognitive error known as “anchoring bias”—fixating on an available, concrete finding rather than considering the full differential diagnosis.
In reality, the true cause might be BPPV (completely unrelated to the spondylosis), vestibular neuritis, or even a central cause like stroke or TIA.
The Whiplash Fallacy: When Trauma Doesn’t Prove the Neck Is Guilty
Whiplash Injury and Post-Traumatic Vertigo
Dizziness following a whiplash injury is another area where the neck is often blamed incorrectly. A car accident, fall, or impact causes the head to accelerate and decelerate rapidly. Intuitively, this involves the neck, so the neck must be responsible for the dizziness.
This reasoning, while intuitive, is incomplete.
What Actually Happens During Whiplash
When the head undergoes rapid acceleration and deceleration:
- Mechanical forces affect the inner ear: The semicircular canals and otolith organs experience rapid acceleration. In some cases, this dislodges otoconia, causing post-traumatic BPPV or traumatic otolith vertigo. This is a peripheral vestibular injury, not a neck injury.
- Mechanical forces affect the brainstem: Severe head acceleration/deceleration can cause concussive injury to the brainstem, affecting the vestibular nuclei. This is a central vestibular injury, not a neck injury.
- Soft tissue injury to the neck: Yes, whiplash does injure neck muscles, ligaments, and facet joints. This causes neck pain, which is a real symptom. However, neck pain does not cause vertigo.
The common error: A patient has both neck pain (real) and dizziness (real) following whiplash. Clinicians assume they share a common cause (the neck injury). In reality, they are separate injuries:
- Neck pain = musculoskeletal injury to the cervical spine and surrounding tissues
- Dizziness = mechanical dislodgement of inner ear crystals OR concussive injury to the brainstem
Post-Traumatic Vertigo: Beyond Whiplash
Post-traumatic vertigo can occur following any head injury, not just whiplash. The mechanisms include:
Post-Traumatic BPPV (PTBPPV)
- Head trauma → force transmitted through semicircular canals
- Otoconia dislodge and migrate into a canal
- Patient experiences positional vertigo similar to spontaneous BPPV
- Treatment: Epley or Semont maneuver (same as spontaneous BPPV)
- Prognosis: Often resolves spontaneously within weeks; if not, maneuver provides cure
Post-Concussion Vertigo / Central Vestibular Injury
- Head trauma with or without loss of consciousness
- Brainstem concussion → vestibular nuclei dysfunction
- Patient experiences continuous dizziness, imbalance, or positional vertigo
- Associated symptoms common: headache, cognitive fog, photophobia, phonophobia
- Recovery: Typically gradual over weeks to months; vestibular rehabilitation accelerates recovery
- Some patients develop persistent postural-perceptual dizziness (PPPD) due to anxiety and deconditioning
Traumatic Brain Injury (TBI) and Vertigo: Red Flags
When dizziness follows head trauma, clinicians must screen for serious central causes:
| Red Flag Symptom | Concern | Action |
|---|---|---|
| Loss of consciousness (any duration) | Moderate-severe TBI | CT/MRI brain |
| Severe headache worsening over hours | Intracranial bleeding | CT brain urgently |
| Vomiting or severe nausea | Increased intracranial pressure | CT brain urgently |
| Altered consciousness or confusion | Diffuse axonal injury or bleeding | CT/MRI brain |
| Seizure after injury | Post-traumatic seizure | CT/MRI + EEG |
| Severe imbalance + positive Dix-Hallpike + nystagmus | BPPV (peripheral, low risk) | Safe for outpatient treatment |
| Constant vertigo + positive HINTS exam (abnormal eye movement) | Central stroke/lesion | MRI brain urgently |
Timeline matters: BPPV post-trauma typically manifests within hours to days. Central post-concussion vertigo develops within the same timeframe but progresses differently. True TBI-related vertigo that worsens over weeks suggests evolving pathology (bleeding, swelling) requiring imaging.
The Danger of Ineffective Treatments for “Cervical Vertigo”
Why Standard Neck Treatments Fail
If a patient has BPPV but is treated for “cervical vertigo,” they will fail to improve. Here’s why:
Neck Collars: Worse Than Useless
In the past (and unfortunately, still sometimes), patients with presumed cervical vertigo were prescribed soft cervical collars to immobilize the neck.
Why this is counterproductive:
- The vestibular system learns through movement. The brain “calibrates” the vestibular system against actual head movements.
- Immobilizing the head prevents this calibration. The brain cannot update its vestibular maps, and dizziness persists.
- Research has shown that immobilization actually prolongs recovery from vestibular disorders.
- For BPPV specifically, immobilization prevents the otoconia from repositioning naturally or with a maneuver.
The paradox: The very intervention intended to stabilize the system actually destabilizes recovery.
Unnecessary Cervical Surgery: High Risk, Low Benefit
In rare cases, patients with attributed “cervical vertigo” are subjected to:
- Anterior cervical discectomy and fusion (ACDF) – removing a degenerated disc and fusing two vertebrae
- Cervical laminectomy – removing part of the vertebra to decompress nerve roots
- Vertebral artery decompression – surgical attempt to relieve presumed vascular compression
The problem:
- These are significant surgical procedures with real risks: infection, bleeding, neurological injury, fusion failure
- Even if the surgery is successful in relieving cervical compression, it will NOT cure vertigo caused by BPPV, vestibular neuritis, or central causes
- Patients undergo these procedures and still have dizziness, having incurred surgical morbidity for no benefit
- True “cervical vertigo” (caused by brainstem ischemia from vertebral artery compression—Bow Hunter’s Syndrome) is so rare that a clinician could practice medicine for decades without seeing it
Delayed Diagnosis of the True Cause
Every day spent treating a “neck problem” is a day lost treating the real cause. For BPPV, this is particularly tragic:
- BPPV is curable with a single maneuver (Epley or Semont) taking less than 10 minutes
- A patient with BPPV can be completely free of vertigo within one office visit
- If that visit is delayed by weeks of neck therapy, the patient suffers needlessly
Bow Hunter’s Syndrome: The ONE Rare Exception
When the Neck Actually Causes Vertigo
Bow Hunter’s Syndrome (BHS) is a legitimate vascular condition where the neck is, indeed, involved in causing vertigo. However, it is exceptionally rare—estimated at perhaps 15 out of 2,000 cases of diagnosed “cervical vertigo.”
Understanding BHS is crucial because:
- It is the only common scenario where cervical imaging is directly relevant to vertigo
- Misdiagnosing BHS as benign BPPV could be dangerous
- Correctly identifying BHS requires specific diagnostic testing and specialist evaluation
What Is Bow Hunter’s Syndrome?
Pathophysiology:
- The vertebral artery runs through small bony canals (transverse foramina) in the cervical vertebrae on its way to the brain
- In some people, a bony spur (osteophyte) grows in a location where it can compress the artery
- When the head is rotated to one side (especially maximally), the bony spur pinches the vertebral artery, temporarily occluding blood flow
- The brainstem becomes partially ischemic (starved of oxygen)
- Vertigo, nystagmus, and other brainstem symptoms occur
Clinical Presentation of Bow Hunter’s Syndrome
Classic features:
- Positional vertigo with head rotation: Unlike BPPV (where vertigo occurs with any head movement), BHS causes vertigo specifically when the head is held in extreme rotation (turned far to one side)
- Positional nystagmus: Eye movements occur that are sustained as long as the head is held in the provocative position
- Brainstem symptoms: May include diplopia (double vision), dysarthria (slurred speech), ataxia (imbalance), or drop attacks (sudden falls without loss of consciousness)
- Symptoms occur while upright: BHS-related symptoms occur when the patient is standing or sitting with the head rotated. This contrasts with BPPV, where symptoms often occur lying down.
- Reproducibility: The symptoms can be reproduced consistently when the examiner rotates the patient’s head to the affected side
Diagnostic Criteria for Bow Hunter’s Syndrome
Imaging:
- Static X-rays or CT scans are NOT diagnostic. Standard imaging may show the bony spur but cannot determine whether it is actually compressing the artery
- Dynamic CT angiography or dynamic MR angiography is required. The patient’s head is rotated while imaging is obtained, and blood flow is monitored in real-time
- The diagnosis is confirmed when blood flow in the vertebral artery stops or severely decreases during head rotation
Clinical examination:
- Rotational vertebral artery occlusion test (RVAO test): Examiner rotates patient’s head to one side and holds for 30–60 seconds while observing for vertigo and nystagmus
- Positive test = vertigo and nystagmus occur and resolve when head is returned to neutral
- However, a positive RVAO test is not specific to BHS (can occur in other conditions); imaging is required to confirm
Management of Bow Hunter’s Syndrome
Conservative management:
- Patient is advised to avoid extreme head rotation
- Activity modification (avoid activities that require sustained head rotation)
- Sometimes effective if patient can comply
Surgical management:
- If conservative measures fail or if symptoms are severe
- Options include:
- Excision of the osteophyte (removing the offending bone spur)
- Cervical fusion (stabilizing the affected vertebra to prevent rotation)
- Suboccipital decompression (widening the space where the vertebral artery travels)
- Success rates vary but can be high (70–90%) if the correct diagnosis was made and the responsible artery is clearly identified
How to Differentiate Bow Hunter’s Syndrome from BPPV
| Feature | BPPV | Bow Hunter’s Syndrome |
|---|---|---|
| Triggered by | Any head movement (lying down, rolling, looking up) | Specific extreme head rotation (one direction) |
| Position when symptoms occur | Often supine or semi-recumbent | While upright (sitting/standing) |
| Duration of nystagmus | Brief (seconds), fatigues with repeated maneuvers | Sustained (as long as head is held rotated) |
| Associated symptoms | Usually none (isolated vertigo/nystagmus) | Often: diplopia, dysarthria, ataxia, drop attacks |
| Diagnosis | Dix-Hallpike test positive | Dynamic angiography positive; RVAO test positive |
| Static imaging finding | None (inner ear crystals not visible) | Bony spur visible, but doesn’t prove occlusion |
| Treatment | Epley/Semont maneuver (cure in minutes) | Activity modification or surgery |
Imaging Comparison: What Each Test Shows
Understanding the Strengths and Limitations of Each Modality
| Imaging Test | What It Shows | Sensitivity for Vertigo Diagnosis | When to Use | Limitations | Cost |
|---|---|---|---|---|---|
| Cervical X-Ray (Plain Radiography) | Bony anatomy (osteophytes, disc space narrowing, vertebral body changes, alignment) | ~5–10% (very low) | Trauma screening, fracture detection, gross deformity assessment | Cannot visualize soft tissues, blood vessels, or function; very high false-positive rate for incidental findings; misses 90%+ of vestibular causes | Low (~$100–200) |
| Cervical CT | High-resolution bony anatomy; can show nerve root compression and vascular calcification | ~5–15% (very low) | Detailed fracture assessment, severe myelopathy suspicion, vertebral artery dissection (if CTA protocol used) | Does not visualize blood flow unless angiography protocol used; radiation exposure; cannot diagnose BPPV or peripheral vestibular disease; high false positive for incidental findings | Moderate (~$300–600) |
| Cervical MRI | Detailed bony and soft tissue anatomy; nerve root compression; disc bulges; brain/brainstem pathology | ~20–30% (still low for vertigo) | Cervical myelopathy, nerve root compression, tumor, demyelinating disease, ischemic stroke in brainstem | Expensive; time-consuming; does not visualize blood flow in detail (unless MRA added); misses BPPV entirely; limited value if vertigo is isolated without cord/neural signs | High (~$1,200–2,500) |
| MR Angiography (MRA) of Vertebral Arteries | Blood vessel anatomy and flow; shows narrowing, dissection, or occlusion of vertebral artery | ~40–50% (moderate, better for vascular lesions) | Suspected vertebrobasilar insufficiency, vertebral artery dissection, Bow Hunter’s Syndrome screening | Static imaging—does NOT show functional occlusion during head movement (misses many BHS cases); expensive; time-consuming; still misses BPPV and peripheral vestibular causes | High (~$1,500–2,500) |
| Dynamic CTA or Dynamic MRA | Blood vessel anatomy during head rotation; shows flow reduction/occlusion during movement | ~80–90% (high for vascular dynamic lesions) | Diagnosis of Bow Hunter’s Syndrome; suspected vertebrobasilar insufficiency with positional component | Requires specialized protocol; not all centers have capability; radiation exposure (CTA); more time-consuming; still does NOT diagnose BPPV | Very High (~$2,000–3,500) |
| Inner Ear MRI (High-Res, T2-Weighted) | Detailed anatomy of semicircular canals, vestibular nerve, labyrinth, cochlea | ~60–70% (moderate-high for labyrinthitis, tumors) | Suspected vestibular neuritis, labyrinthitis, labyrinthine ossification, acoustic neuroma, perilymphatic fistula | Cannot visualize individual otoconia (too small); cannot diagnose BPPV; expensive; requires specific imaging protocol | Very High (~$1,500–2,500) |
| Dix-Hallpike Maneuver (Bedside Positional Test) | Provokes nystagmus if posterior canal BPPV present; no imaging required | 90–95% (very high for posterior canal BPPV) | GOLD STANDARD for BPPV diagnosis; immediate, no cost, diagnostic and therapeutic | Only tests posterior canal (accounts for ~90% of BPPV); central causes can mimic; requires trained examiner | FREE (bedside test) |
| HINTS Exam (Head Impulse, Nystagmus, Test of Skew) | 3 rapid bedside eye movement tests; >96% sensitive/specific for central vs. peripheral vertigo | >96% (very high for ruling out central causes like stroke) | SUPERIOR TO MRI for acute vertigo; rules out stroke at bedside in 60 seconds | Requires training; false positives with ocular dystopia; still requires confirmatory imaging if positive | FREE (bedside test) |
Key Takeaway for Vertigo Diagnosis
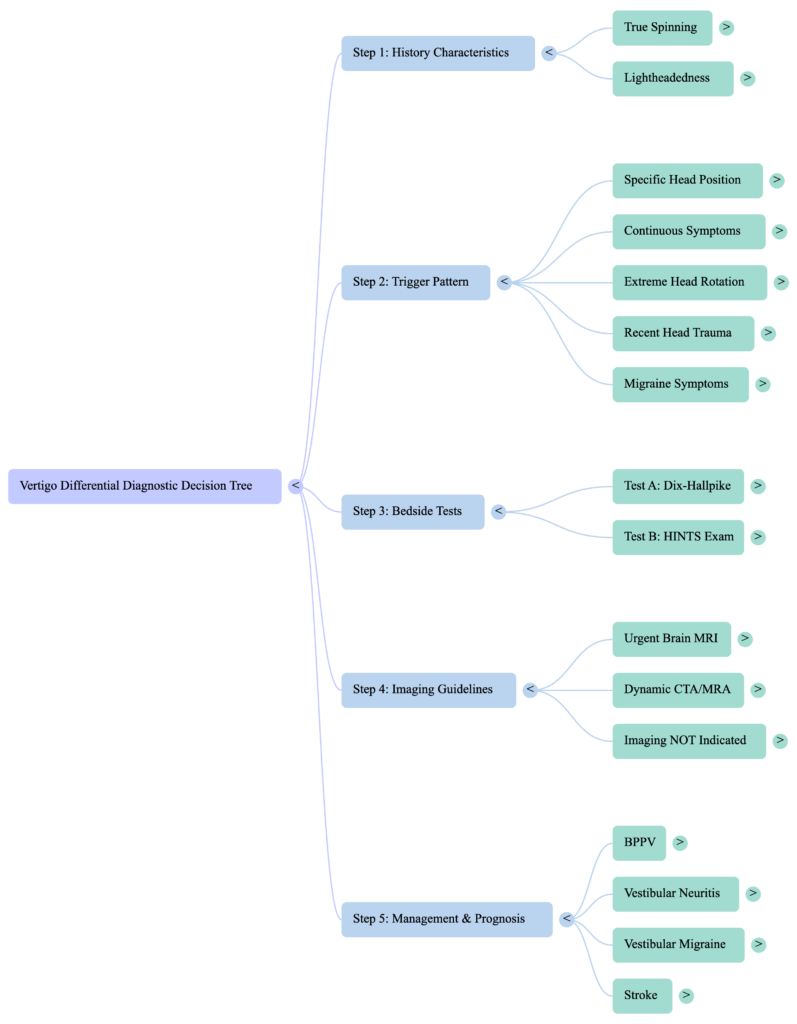
For isolated vertigo without trauma, neurological symptoms, or vascular risk factors:
- First step: Detailed history + physical exam (Dix-Hallpike test + HINTS exam)
- Second step: If Dix-Hallpike positive → BPPV diagnosed, treat with Epley maneuver, no imaging needed
- Third step: If HINTS positive (abnormal eye movement) → MRI brain to rule out stroke
- Fourth step: If Dix-Hallpike and HINTS both negative but vertigo is persistent → inner ear MRI or vestibular testing (caloric, vHIT)
Cervical imaging is NOT a first-line test for isolated vertigo. It is only indicated if there is:
- Neck pain and weakness (suggesting nerve root compression)
- Suspicion of vertebral artery dissection (trauma, extreme pain, neurological symptoms)
- Suspicion of Bow Hunter’s Syndrome (positional vertigo during extreme head rotation, brainstem symptoms)
How to Escape the Cervical Misdiagnosis Trap
The Right Way to Evaluate Vertigo
Step 1: Detailed History
A good history is 80% of the diagnosis.
Ask:
- When did it start? Sudden (BPPV, vestibular neuritis, stroke) vs. gradual (migraine, Menière’s, MS)
- What does it feel like? True spinning/vertigo (inner ear or brainstem) vs. lightheadedness/dizziness (cardiovascular, metabolic)
- What triggers it? Specific positions (BPPV), head movements (migraine, anxiety), sudden standing (hypotension), visual motion (migraine)
- Associated symptoms? Headache, hearing loss, tinnitus, visual symptoms, weakness, numbness, speech difficulty?
- Was there head trauma or whiplash? (post-traumatic BPPV vs. post-concussion vertigo)
- How is it now? Improving, stable, or worsening? (improving suggests BPPV; worsening suggests stroke or tumor)
Key principle: True vertigo (spinning) almost always means a problem in the vestibular system (peripheral) or brainstem/cerebellum (central). Lightheadedness suggests cardiovascular, metabolic, or anxiety causes.
Step 2: The Dix-Hallpike Test—The Gold Standard for BPPV
What it tests: Whether posterior canal BPPV is present
How it’s performed:
- Patient sits upright on edge of examination table
- Examiner turns patient’s head 45° to one side
- Examiner rapidly lowers patient to supine position with head hanging off edge of table
- Examiner observes patient’s eyes for nystagmus (involuntary eye movements)
Positive test:
- Latency: 1–5 second delay before nystagmus appears (important—immediate nystagmus suggests central cause)
- Nystagmus: Rotatory nystagmus (eye rotates clockwise or counterclockwise) + vertical nystagmus (upward component)
- Duration: Usually 10–60 seconds
- Patient reports: Vertigo sensation (room spinning, or self spinning)
If positive: BPPV is diagnosed. Epley or Semont maneuver is performed immediately—curative in 80–90% of cases.
If negative: BPPV is ruled out in the posterior canal. (Note: Anterior canal BPPV requires different testing.)
Step 3: The HINTS Exam—Superior to MRI for Acute Stroke Rule-Out
What it tests: Central vs. peripheral cause of acute vertigo in patients with severe dizziness
The HINTS acronym:
- H: Head Impulse Test – examiner moves head side-to-side while patient fixates on examiner’s nose; assesses whether eyes stay fixed (normal) or drift off target (abnormal)
- I: Nystagmus – what direction is the nystagmus? Upward/downward nystagmus or convergent nystagmus suggests central; pure rotatory/horizontal suggests peripheral
- T: Test of Skew – look for vertical misalignment of the eyes (one eye higher than the other), suggesting brainstem dysfunction
Accuracy:
- Sensitivity ~96% for detecting central causes (stroke, tumor, MS)
- Specificity ~95% for confirming peripheral causes
Clinical impact:
- If HINTS is normal (all three components normal) → peripheral cause → safe to observe, treat conservatively, perform vestibular rehabilitation
- If HINTS is abnormal → central cause → MRI urgently to rule out stroke
Advantage over MRI: HINTS takes 60 seconds at bedside. MRI takes hours and is expensive. Early identification of stroke allows early thrombolytic intervention, which is time-critical.
Step 4: Vestibular Rehabilitation Therapy (VRT)
If BPPV is treated but residual imbalance persists, or if peripheral vestibular loss is confirmed:
VRT is specific exercises that retrain the brain’s balance mechanisms:
- Gaze stabilization exercises – improves eye fixation during head movement
- Balance training – standing on unstable surfaces, tandem stance, single-leg stance
- Habituation exercises – gradual exposure to motion-provocative stimuli (for BPPV recurrence or visual dizziness)
Evidence: VRT is effective in 60–80% of patients with peripheral vestibular disorders.
What NOT to Do
- ❌ Prescribe a cervical collar or suggest neck immobilization
- ❌ Order cervical imaging as a first-line test for isolated vertigo
- ❌ Assume spondylosis on imaging means spondylosis caused the vertigo
- ❌ Delay vestibular-specific testing (Dix-Hallpike, HINTS) to pursue imaging
- ❌ Refer for unnecessary neck surgery without confirmed central cause
Conclusion: Reclaim Your Vertigo Diagnosis
Stop letting your neck X-ray dictate your vertigo treatment. Bony changes in the spine are a normal part of aging, but spinning vertigo is almost always a mechanical problem of the balance system (BPPV, vestibular neuritis) or a neurological problem of the brainstem (stroke, migraine). The spine is rarely the culprit.
If you are trapped in a cycle of neck treatments with no relief:
- Request a vestibular evaluation from your primary care doctor or ENT specialist
- Ask for the Dix-Hallpike test – the gold standard for the most common cause of vertigo
- If Dix-Hallpike is positive, ask for the Epley maneuver immediately – it is diagnostic AND therapeutic
- If symptoms persist, ask for the HINTS exam – to rule out a central cause
- If imaging is obtained, understand what it does and doesn’t show – normal cervical imaging does not mean your vertigo is not real, and abnormal imaging does not mean it caused your vertigo
The right diagnosis leads to the right treatment. The right treatment leads to relief.
HINGLISH VERSION
Cervical Misdiagnosis Trap: Kaise Neck X-Rays Aapke Vertigo Treatment Ko Badh Dete Hain
Introduction: Trap Jo Millions Ko Pakde
Jab koi “chakkar” ya spinning complain karti hai, sabka first instinct neck dekhai hai. Intuitive, visible, imaging available. Lekin fundamentally flawed.
Result? Neck X-rays aur CT scans age-related wear (spondylosis, osteophytes) dikharti hain. Lagta hai “explained”। Lekin “cervical vertigo” ek most controversial diagnosis hai। Patients years tak neck treatment lerti hain—collars, surgery, meds—real cause (usually inner ear) ignore hote hai।
The Myth of the “Bad Neck”
Head Movement ≠ Neck Problem
Sab mante hain neck problems = vertigo kyunke jab head rotate, dizzy hote ho। Logical lagta hai।
Lekin fundamental truth: Vestibular system = head-movement detection system। Semicircular canals = rotational acceleration sense करते। Utricle/saccule = linear acceleration sense।
Critically: all head movements involve neck movement। Left-right rotate nahi kar sakte without cervical spine rotate।
Therefore, ANY primary vestibular disorder more symptomatic होगी when head moves।
False correlation:
- Head move → vertigo → neck = culprit
- X-ray = spondylosis → diagnosis “confirm”
Reality: Spondylosis = incidental, normal aging, NO relationship!
Evidence: Spondylosis Common, Usually Innocent
- 70–80% adults 70+ = cervical spondylosis
- 30–40% adults 50s = radiographic changes
- Most = NO neck pain या vertigo
Agar spondylosis = vertigo, elderly epidemic होना chahiye। Nahi। Spondylosis independent; true causes (BPPV, vestibular neuritis) अलग।
BPPV: Great Mimicker of “Cervical Vertigo”
BPPV Kaise Neck Problem Lagta Hai
BPPV = most common cause of recurrent vertigo (20–40% cases)। Cervical trap = BPPV।
How BPPV:
- Calcium carbonate crystals (otoconia) = normally utricle में embedded
- Dislodge → semicircular canal में migrate
- Head move → crystals shift → false rotation signals
- Brain = violent spinning perceive
Why mimics neck?
- Triggered by lying down (head horizontal extension)
- Triggered by rolling (head rotation + neck extension)
- Triggered by looking up (cervical extension)
- Triggered by head turn (cervical rotation)
All involve neck। Observer assume neck = problem।
Misdiagnosis Cascade
- Bed roll → spinning (BPPV)
- Patient = “bad neck” assume
- Neck X-rays (age-related spondylosis दिखता है)
- Doctor = “cervical vertigo” diagnose
- Neck stretches, collar, PT
- Symptoms persist (BPPV nahi treated!)
- Weeks/months futile treatment
- Finally vestibular specialist → Dix-Hallpike positive
- Epley maneuver → cured in minutes!
Lost opportunity: Day 1 pe Dix-Hallpike = diagnosis + cure in 5 min।
Why X-Rays Misleading
X-Rays = Bone, Not Function
Core problem: X-rays = anatomy (bone) नहीं function (nerves, blood, mechanics)। Normal ≠ healthy; Abnormal ≠ caused।
Three Critical Mistakes
1. Spondylosis = C4–C7; Rotation = C1–C2
C4–C7 = flexion/extension। Degeneration = nerve compression possible, lekin direct effect semicircular canal पर नहीं।
C1–C2 = head rotation (left-right)। Less degenerate, lekin even severe C1–C2 degeneration = vestibular system failure explain नहीं करता।
Disconnect: C4–C7 spondylosis ≠ room spinning।
2. Vertigo = Semicircular Canal या Central Problem, Not Spine
Vertigo = hallucination of movement। Indicates:
- Semicircular canal problem (BPPV, labyrinthitis)
- Vestibular nerve problem (neuritis)
- Brainstem problem (stroke, MS)
Bone spur in cervical spine = none of these disrupt कर सकता। Spur ≠ dislodge otoconia, ≠ infect nerve, ≠ damage nuclei।
3. “Red Herrings” Common in Elderly
Aging patients = multiple findings:
- Asymptomatic spondylosis (common)
- Mild orthostatic hypotension
- Presbycusis (hearing loss)
- Mild gait ataxia
Temptation = visible finding (spondylosis) को culprit मानना। Cognitive bias। True cause = BPPV, vestibular neuritis, या stroke!
Whiplash: Post-Traumatic Vertigo
What Actually Happens
Head acceleration/deceleration → inner ear + brainstem affected:
- Inner ear: Otoconia dislodge → post-traumatic BPPV (peripheral vestibular injury)
- Brainstem: Concussive injury → vestibular nuclei dysfunction (central injury)
- Neck: YES, muscles/ligaments injured → neck pain (real, lekin ≠ vertigo)
Common error: Both pain + dizziness = same cause। WRONG। Separate injuries!
Post-Traumatic Vertigo Types
1. Post-Traumatic BPPV (PTBPPV)
- Head trauma → otoconia dislodge
- Positional vertigo (BPPV-like)
- Treatment: Epley maneuver (same as spontaneous BPPV)
- Prognosis: Weeks में resolve, या maneuver = cure
2. Post-Concussion Vertigo
- Brainstem concussion
- Continuous dizziness या positional
- Associated: Headache, cognitive fog, photophobia, phonophobia
- Recovery: Weeks-months; VRT accelerate करता है
- Risk: PPPD (anxiety + deconditioning)
3. TBI Red Flags
| Red Flag | Concern | Action |
|---|---|---|
| Loss of consciousness | Moderate-severe TBI | CT/MRI brain |
| Worsening headache | Intracranial bleeding | CT urgently |
| Vomiting/severe nausea | ICP increased | CT urgently |
| Altered consciousness | Diffuse axonal injury | CT/MRI brain |
| Seizure | Post-traumatic seizure | CT/MRI + EEG |
| Severe imbalance + Dix-Hallpike+ | BPPV (low risk) | Outpatient safe |
| Constant vertigo + HINTS abnormal | Central stroke | MRI urgently |
Timeline: BPPV post-trauma = hours-days। TBI vertigo worsening over weeks = evolving pathology (imaging needed)।
The Danger of Ineffective Treatments
Neck Collars: Worse Than Useless
Immobilization = vestibular recovery prevent कर देता है। Brain को movement से calibrate करना पड़ता है। Immobilize = no calibration = persistent dizziness!
Paradox: Treatment = recovery actually delay!
Unnecessary Surgery
ACDF, laminectomy, vertebral artery decompression = high-risk procedures:
- Real risks: infection, bleeding, neurological injury
- Won’t cure BPPV, vestibular neuritis, central causes
- Patient = still dizzy + surgical morbidity
Bow Hunter’s Syndrome: ONE Exception
Kab Neck Actually Causes Vertigo
Bow Hunter’s Syndrome (BHS) = ONE rare legitimate case where neck involved।
How:
- Vertebral artery = transverse foramina through cervical spine
- Bony spur grows
- Extreme head rotation → spur pinches artery
- Blood flow blocks → brainstem ischemic
- Vertigo + nystagmus + brainstem symptoms
Rarity: 15 out of 2,000 “cervical vertigo” cases।
Clinical Features
- Positional vertigo: Extreme head rotation करने से (BPPV ≠ specific direction)
- Sustained nystagmus: Head rotated रहने तक (BPPV = brief)
- Brainstem symptoms: Diplopia, speech slurred, ataxia, drop attacks
- Upright symptoms: Sitting/standing, not lying down
- Reproducible: Consistent rotational provocation
Diagnosis
Imaging:
- ❌ Static X-ray/CT = NOT diagnostic
- ✅ Dynamic CTA or dynamic MRA = required (head rotate करते time blood flow देखना)
- ✅ RVAO test (examiner rotate, observe nystagmus)
BPPV vs. BHS
| Feature | BPPV | BHS |
|---|---|---|
| Triggered by | Any head movement | Extreme rotation (one direction) |
| Position | Often supine | Upright |
| Nystagmus | Brief, fatigue | Sustained |
| Associated symptoms | None | Diplopia, dysarthria, ataxia |
| Diagnosis | Dix-Hallpike | Dynamic angiography |
| Treatment | Epley (minutes) | Activity modification या surgery |
Imaging: What Each Shows
Complete Comparison
| Test | Shows | Sensitivity (Vertigo) | When | Limitations | Cost |
|---|---|---|---|---|---|
| Neck X-Ray | Bone (osteophytes, disc narrowing) | 5–10% | Fracture screening | Can’t see soft tissue/blood/function; high false positives | Low |
| Cervical CT | Detailed bone; nerve root | 5–15% | Fracture/deformity | No blood flow; radiation; false positives | Moderate |
| Cervical MRI | Bone + soft tissue; brainstem | 20–30% | Cord compression, tumors, stroke | Expensive; slow; misses BPPV | High |
| MRA | Vertebral artery anatomy | 40–50% | Dissection, insufficiency | Static (not dynamic); misses functional occlusion | High |
| Dynamic CTA/MRA | Blood flow during movement | 80–90% (vascular lesions) | BHS diagnosis | Specialized; radiation (CTA); misses BPPV | Very High |
| Inner Ear MRI | Labyrinth, vestibular nerve | 60–70% | Neuritis, tumors, fistula | Can’t see otoconia; expensive | Very High |
| VNG/EOG | Eye movements | 50–70% | Central vs peripheral | Doesn’t localize; operator-dependent | Low |
| Caloric Test | Vestibular asymmetry | 70–80% | Unilateral loss | Doesn’t diagnose BPPV; uncomfortable | Moderate |
| vHIT | Vestibulo-ocular reflex | 75–85% | Peripheral weakness | Doesn’t diagnose cause | Moderate |
| Posturography | Balance integration | 60–70% | Rehabilitation assessment | Doesn’t diagnose; expensive | High |
| Dix-Hallpike | Posterior canal BPPV | 90–95% | GOLD STANDARD, BPPV | Only posterior canal; requires training | FREE |
| HINTS Exam | Central vs peripheral | >96% | SUPERIOR to MRI, acute stroke | Requires training | FREE |
Key: First Steps
- History + physical (Dix-Hallpike + HINTS)
- Dix-Hallpike positive? → BPPV, Epley, no imaging
- HINTS abnormal? → MRI brain (stroke rule-out)
- Both normal, persistent? → Inner ear MRI या vestibular testing
- Cervical imaging? → केवल trauma/pain/arterial suspicion
How to Escape the Trap
Right Evaluation
1. Detailed History
- When? Sudden (BPPV, neuritis, stroke) vs gradual (migraine, Menière’s)
- Feels like? True spinning (inner ear/brainstem) vs lightheaded (heart/metabolism)
- Triggers? Specific positions (BPPV), head movement (migraine), standing up (hypotension)
- Associated? Headache, hearing, tinnitus, visual, weakness, speech?
- Trauma? Whiplash या head injury?
- Now? Improving (BPPV) या worsening (stroke)?
Key: True vertigo = vestibular (inner ear/brainstem)। Lightheadedness = cardiovascular/metabolic/anxiety।
2. Dix-Hallpike Test—GOLD STANDARD
- Patient sit upright
- Head rotate 45° one side
- Rapidly lower to supine, head hanging
- Observe eyes = nystagmus?
Positive:
- Latency: 1–5 sec
- Rotatory + vertical nystagmus
- Duration: 10–60 sec
- Patient reports: Spinning
Positive = BPPV, Epley, 80–90% cure rate।
3. HINTS Exam—BETTER THAN MRI
3 rapid eye tests:
- H: Head Impulse (eyes stay fixed या drift?)
- I: nystagmus direction (upward = central; rotatory = peripheral)
- T: Test of Skew (vertical eye misalignment = brainstem)
Accuracy:
- 96% sensitivity (detect central/stroke)
- 95% specificity (confirm peripheral)
60 seconds, bedside, free, >96% stroke rule-out।
4. VRT
BPPV treated लेकिन imbalance remain?
VRT = exercise program:
- Gaze stabilization
- Balance training
- Habituation exercises
Efficacy: 60–80% peripheral vestibular disorders।
Conclusion
Stop cervical X-ray को vertigo treatment dictate करने दो। Spondylosis = normal aging; spinning vertigo = balance system (BPPV, neuritis) या brainstem (stroke)।
Trapped in neck treatment cycle?
- Vestibular evaluation request करो
- Dix-Hallpike ask करो (gold standard)
- Positive = Epley immediately (diagnostic + therapeutic)
- Persistent = HINTS exam करो (central rule-out)
- Imaging? Understand: Normal ≠ problem nahi; abnormal ≠ caused।
Right diagnosis = right treatment = relief।
HINDI VERSION
Cervical Misdiagnosis Trap: कैसे Neck X-Rays आपके Vertigo Treatment को मार रहे हैं
Introduction: Trap जो Millions को पकड़ता है
जब कोई “चक्कर” या spinning complain करता है, तो सभी का पहला instinct neck देखना है। Intuitive, visible, imaging available। लेकिन fundamentally flawed।
Result? Neck X-rays और CT scans age-related wear (spondylosis, osteophytes) दिखाते हैं। लगता है “explained”। लेकिन “cervical vertigo” एक most controversial diagnosis है। मरीज़ साल भर neck treatment लेते हैं—collars, surgery, meds—real cause (usually inner ear) ignore होता है।
The Myth of the “Bad Neck”
Head Movement ≠ Neck Problem
सब मानते हैं neck problems = vertigo क्योंकि जब head rotate करते हो, dizzy होते हो। Logical लगता है।
लेकिन fundamental truth: Vestibular system = head-movement detection system। Semicircular canals = rotational acceleration sense करते हैं। Utricle/saccule = linear acceleration sense।
Critically: all head movements involve neck movement। Left-right rotate नहीं कर सकते without cervical spine rotate।
Therefore, ANY primary vestibular disorder अधिक symptomatic होगी when head moves।
False correlation:
- Head move → vertigo → neck = culprit
- X-ray = spondylosis → diagnosis “confirm”
Reality: Spondylosis = incidental, normal aging, NO relationship!
Evidence: Spondylosis Common, Usually Innocent
- 70–80% adults 70+ = cervical spondylosis
- 30–40% adults 50s = radiographic changes
- Most = NO neck pain या vertigo
अगर spondylosis = vertigo, elderly epidemic होना चाहिए। नहीं। Spondylosis independent; true causes (BPPV, vestibular neuritis) अलग।
BPPV: Great Mimicker of “Cervical Vertigo”
BPPV कैसे Neck Problem लगता है
BPPV = most common cause of recurrent vertigo (20–40% cases)। Cervical trap = BPPV।
How BPPV:
- Calcium carbonate crystals (otoconia) = normally utricle में embedded
- Dislodge → semicircular canal में migrate
- Head move → crystals shift → false rotation signals
- Brain = violent spinning perceive
Why mimics neck?
- Triggered by lying down (head horizontal extension)
- Triggered by rolling (head rotation + neck extension)
- Triggered by looking up (cervical extension)
- Triggered by head turn (cervical rotation)
All involve neck। Observer assume neck = problem।
Misdiagnosis Cascade
- Bed roll → spinning (BPPV)
- Patient = “bad neck” assume
- Neck X-rays (age-related spondylosis दिखता है)
- Doctor = “cervical vertigo” diagnose
- Neck stretches, collar, PT
- Symptoms persist (BPPV नहीं treated!)
- Weeks/months futile treatment
- Finally vestibular specialist → Dix-Hallpike positive
- Epley maneuver → cured in minutes!
Lost opportunity: Day 1 पे Dix-Hallpike = diagnosis + cure in 5 min।
Why X-Rays Misleading
X-Rays = Bone, Not Function
Core problem: X-rays = anatomy (bone) नहीं function (nerves, blood, mechanics)। Normal ≠ healthy; Abnormal ≠ caused।
Three Critical Mistakes
1. Spondylosis = C4–C7; Rotation = C1–C2
C4–C7 = flexion/extension। Degeneration = nerve compression possible, लेकिन direct effect semicircular canal पर नहीं।
C1–C2 = head rotation (left-right)। Less degenerate, लेकिन even severe C1–C2 degeneration = vestibular system failure explain नहीं करता।
Disconnect: C4–C7 spondylosis ≠ room spinning।
2. Vertigo = Semicircular Canal या Central Problem, Not Spine
Vertigo = hallucination of movement। Indicates:
- Semicircular canal problem (BPPV, labyrinthitis)
- Vestibular nerve problem (neuritis)
- Brainstem problem (stroke, MS)
Bone spur in cervical spine = none of these disrupt कर सकता। Spur ≠ dislodge otoconia, ≠ infect nerve, ≠ damage nuclei।
3. “Red Herrings” Common in Elderly
Aging patients = multiple findings:
- Asymptomatic spondylosis (common)
- Mild orthostatic hypotension
- Presbycusis (hearing loss)
- Mild gait ataxia
Temptation = visible finding (spondylosis) को culprit मानना। Cognitive bias। True cause = BPPV, vestibular neuritis, या stroke!
Whiplash: Post-Traumatic Vertigo
What Actually Happens
Head acceleration/deceleration → inner ear + brainstem affected:
- Inner ear: Otoconia dislodge → post-traumatic BPPV (peripheral vestibular injury)
- Brainstem: Concussive injury → vestibular nuclei dysfunction (central injury)
- Neck: YES, muscles/ligaments injured → neck pain (real, लेकिन ≠ vertigo)
Common error: Both pain + dizziness = same cause। WRONG। Separate injuries!
Post-Traumatic Vertigo Types
1. Post-Traumatic BPPV (PTBPPV)
- Head trauma → otoconia dislodge
- Positional vertigo (BPPV-like)
- Treatment: Epley maneuver (same as spontaneous BPPV)
- Prognosis: Weeks में resolve, या maneuver = cure
2. Post-Concussion Vertigo
- Brainstem concussion
- Continuous dizziness या positional
- Associated: Headache, cognitive fog, photophobia, phonophobia
- Recovery: Weeks-months; VRT accelerate करता है
- Risk: PPPD (anxiety + deconditioning)
3. TBI Red Flags
| Red Flag | Concern | Action |
|---|---|---|
| Loss of consciousness | Moderate-severe TBI | CT/MRI brain |
| Worsening headache | Intracranial bleeding | CT urgently |
| Vomiting/severe nausea | ICP increased | CT urgently |
| Altered consciousness | Diffuse axonal injury | CT/MRI brain |
| Seizure | Post-traumatic seizure | CT/MRI + EEG |
| Severe imbalance + Dix-Hallpike+ | BPPV (low risk) | Outpatient safe |
| Constant vertigo + HINTS abnormal | Central stroke | MRI urgently |
Timeline: BPPV post-trauma = hours-days। TBI vertigo worsening over weeks = evolving pathology (imaging needed)।
The Danger of Ineffective Treatments
Neck Collars: Worse Than Useless
Immobilization = vestibular recovery prevent कर देता है। Brain को movement से calibrate करना पड़ता है। Immobilize = no calibration = persistent dizziness!
Paradox: Treatment = recovery actually delay!
Unnecessary Surgery
ACDF, laminectomy, vertebral artery decompression = high-risk procedures:
- Real risks: infection, bleeding, neurological injury
- Won’t cure BPPV, vestibular neuritis, central causes
- Patient = still dizzy + surgical morbidity
Bow Hunter’s Syndrome: ONE Exception
कब Neck Actually Causes Vertigo
Bow Hunter’s Syndrome (BHS) = ONE rare legitimate case where neck involved।
How:
- Vertebral artery = transverse foramina through cervical spine
- Bony spur grows
- Extreme head rotation → spur pinches artery
- Blood flow blocks → brainstem ischemic
- Vertigo + nystagmus + brainstem symptoms
Rarity: 15 out of 2,000 “cervical vertigo” cases।
Clinical Features
- Positional vertigo: Extreme head rotation करने से (BPPV ≠ specific direction)
- Sustained nystagmus: Head rotated रहने तक (BPPV = brief)
- Brainstem symptoms: Diplopia, speech slurred, ataxia, drop attacks
- Upright symptoms: Sitting/standing, not lying down
- Reproducible: Consistent rotational provocation
Diagnosis
Imaging:
- ❌ Static X-ray/CT = NOT diagnostic
- ✅ Dynamic CTA or dynamic MRA = required (head rotate करते समय blood flow देखना)
- ✅ RVAO test (examiner rotate, observe nystagmus)
BPPV vs. BHS
| Feature | BPPV | BHS |
|---|---|---|
| Triggered by | Any head movement | Extreme rotation (one direction) |
| Position | Often supine | Upright |
| Nystagmus | Brief, fatigue | Sustained |
| Associated symptoms | None | Diplopia, dysarthria, ataxia |
| Diagnosis | Dix-Hallpike | Dynamic angiography |
| Treatment | Epley (minutes) | Activity modification या surgery |
Imaging: What Each Shows
Complete Comparison
| Test | Shows | Sensitivity (Vertigo) | When | Limitations | Cost |
|---|---|---|---|---|---|
| Neck X-Ray | Bone (osteophytes, disc narrowing) | 5–10% | Fracture screening | Can’t see soft tissue/blood/function; high false positives | Low |
| Cervical CT | Detailed bone; nerve root | 5–15% | Fracture/deformity | No blood flow; radiation; false positives | Moderate |
| Cervical MRI | Bone + soft tissue; brainstem | 20–30% | Cord compression, tumors, stroke | Expensive; slow; misses BPPV | High |
| MRA | Vertebral artery anatomy | 40–50% | Dissection, insufficiency | Static (not dynamic); misses functional occlusion | High |
| Dynamic CTA/MRA | Blood flow during movement | 80–90% (vascular lesions) | BHS diagnosis | Specialized; radiation (CTA); misses BPPV | Very High |
| Inner Ear MRI | Labyrinth, vestibular nerve | 60–70% | Neuritis, tumors, fistula | Can’t see otoconia; expensive | Very High |
| VNG/EOG | Eye movements | 50–70% | Central vs peripheral | Doesn’t localize; operator-dependent | Low |
| Caloric Test | Vestibular asymmetry | 70–80% | Unilateral loss | Doesn’t diagnose BPPV; uncomfortable | Moderate |
| vHIT | Vestibulo-ocular reflex | 75–85% | Peripheral weakness | Doesn’t diagnose cause | Moderate |
| Posturography | Balance integration | 60–70% | Rehabilitation assessment | Doesn’t diagnose; expensive | High |
| Dix-Hallpike | Posterior canal BPPV | 90–95% | GOLD STANDARD, BPPV | Only posterior canal; requires training | FREE |
| HINTS Exam | Central vs peripheral | >96% | SUPERIOR to MRI, acute stroke | Requires training | FREE |
Key: First Steps
- History + physical (Dix-Hallpike + HINTS)
- Dix-Hallpike positive? → BPPV, Epley, no imaging
- HINTS abnormal? → MRI brain (stroke rule-out)
- Both normal, persistent? → Inner ear MRI या vestibular testing
- Cervical imaging? → केवल trauma/pain/arterial suspicion
How to Escape the Trap
Right Evaluation
1. Detailed History
- When? Sudden (BPPV, neuritis, stroke) vs gradual (migraine, Menière’s)
- Feels like? True spinning (inner ear/brainstem) vs lightheaded (heart/metabolism)
- Triggers? Specific positions (BPPV), head movement (migraine), standing up (hypotension)
- Associated? Headache, hearing, tinnitus, visual, weakness, speech?
- Trauma? Whiplash या head injury?
- Now? Improving (BPPV) या worsening (stroke)?
Key: True vertigo = vestibular (inner ear/brainstem)। Lightheadedness = cardiovascular/metabolic/anxiety।
2. Dix-Hallpike Test—GOLD STANDARD
- Patient sit upright
- Head rotate 45° one side
- Rapidly lower to supine, head hanging
- Observe eyes = nystagmus?
Positive:
- Latency: 1–5 sec
- Rotatory + vertical nystagmus
- Duration: 10–60 sec
- Patient reports: Spinning
Positive = BPPV, Epley, 80–90% cure rate।
3. HINTS Exam—BETTER THAN MRI
3 rapid eye tests:
- H: Head Impulse (eyes stay fixed या drift?)
- I: nystagmus direction (upward = central; rotatory = peripheral)
- T: Test of Skew (vertical eye misalignment = brainstem)
Accuracy:
- 96% sensitivity (detect central/stroke)
- 95% specificity (confirm peripheral)
60 seconds, bedside, free, >96% stroke rule-out।
4. VRT
BPPV treated लेकिन imbalance remain?
VRT = exercise program:
- Gaze stabilization
- Balance training
- Habituation exercises
Efficacy: 60–80% peripheral vestibular disorders।
Conclusion
Stop cervical X-ray को vertigo treatment dictate करने दो। Spondylosis = normal aging; spinning vertigo = balance system (BPPV, neuritis) या brainstem (stroke)।
Trapped in neck treatment cycle?
- Vestibular evaluation request करो
- Dix-Hallpike ask करो (gold standard)
- Positive = Epley immediately (diagnostic + therapeutic)
- Persistent = HINTS exam करो (central rule-out)
- Imaging? Understand: Normal ≠ problem नहीं; abnormal ≠ caused।
Right diagnosis = right treatment = relief।
IMAGING COMPARISON: WHAT EACH TEST SHOWS
(Reference Table – Diagnostic Accuracy & When to Use)
Complete Imaging Decision Matrix
For clinicians and informed patients: Understanding when each test is appropriate and what it reveals (and hides).
| Imaging Modality | Primary Visibility | Diagnostic Sensitivity for Vertigo | Specificity | Best Use Case | Critical Limitations | Radiation Exposure | Typical Cost | Time Required |
|---|---|---|---|---|---|---|---|---|
| Cervical Spine X-Ray (Plain Radiography) | Bony structures: vertebral bodies, disc spaces, osteophytes, alignment, foraminal narrowing | 5–10% (very low) | 15–20% (very low) | Trauma screening, fracture detection, gross deformity assessment | Cannot visualize soft tissue, blood vessels, or functional pathology; extremely high false-positive rate from incidental spondylosis; misses 90%+ of vestibular causes | Low (single AP/lateral) | $100–200 | 5–10 min |
| Cervical Spine CT | High-resolution bone detail, disc material, foraminal narrowing, vertebral artery calcification visible | 5–15% (low) | 20–25% (low) | Detailed fracture assessment, severe myelopathy suspicion, vertebral artery dissection (if CTA protocol used) | Does not visualize blood flow unless angiography protocol used; radiation exposure; cannot diagnose BPPV or peripheral vestibular disease; high false positive for incidental findings | Moderate (cervical spine dose ~2 mSv) | $300–600 | 10–20 min |
| Cervical Spine MRI (Standard Protocol) | Bone marrow, spinal cord, nerve roots, discs, ligaments, brainstem detail | 20–30% (still low for vertigo) | 40–50% (moderate) | Cervical myelopathy, nerve root compression, tumor, demyelinating disease, ischemic stroke in brainstem | Expensive; time-consuming; cannot visualize blood flow in detail (unless MRA added); misses BPPV entirely; limited value if vertigo is isolated without cord/neural signs; false positives common | None | $1,200–2,500 | 30–60 min |
| MR Angiography (MRA) of Vertebral Arteries | Vertebral artery and basilar artery anatomy, luminal diameter, flow dynamics, dissection detection | 40–50% (moderate, better for vascular lesions) | 70–75% (better for vascular pathology) | Suspected vertebrobasilar insufficiency, vertebral artery dissection, Bow Hunter’s Syndrome screening | Static imaging—does NOT show functional occlusion during head movement (misses many BHS cases); expensive; time-consuming; still does NOT diagnose BPPV, AICA stroke, or peripheral vestibular disease | None (MRI-based) | $1,500–2,500 | 20–40 min |
| Dynamic CTA or Dynamic MRA (Head Rotation During Scan) | Blood flow in vertebral arteries during actual head rotation; real-time occlusion visualization | 80–90% (high for vascular dynamic lesions) | 85–90% (high specificity for BHS) | Definitive diagnosis of Bow Hunter’s Syndrome, vertebral artery compression, functional vertebrobasilar insufficiency | Requires specialized imaging protocol not available at all centers; CTA = radiation exposure; still CANNOT diagnose BPPV; time-consuming and expensive | High (CTA protocol ~10 mSv effective dose) | $2,000–3,500 | 45–90 min |
| High-Resolution Inner Ear MRI (3T, T2-Weighted, Thin Sections) | Detailed anatomy of semicircular canals, vestibular nerve, endolymphatic sac, cochlea, membranous labyrinth detail | 60–70% (moderate, varies by pathology) | 65–75% (depends on pathology type) | Vestibular neuritis, labyrinthitis, acoustic neuroma, labyrinthine ossification, perilymphatic fistula, endolymphatic hydrops | CANNOT visualize individual otoconia (too small ~10 micrometers); CANNOT diagnose BPPV; expensive; requires specific imaging protocol; false positives possible with motion artifact | None | $1,500–2,500 | 30–45 min |
| Videonystagmography (VNG) / Electro-Oculography (EOG) | Eye movement patterns, nystagmus direction, velocity, symmetry; gaze-evoked nystagmus | 50–70% (depends on type of nystagmus) | 60–75% (depends on pattern specificity) | Documenting nystagmus type, differentiating central vs peripheral patterns, bedside examination during consultation | Does NOT localize lesion anatomically; requires trained operator and patient cooperation; cannot replace structural imaging; findings nonspecific without clinical context | None | $200–400 | 15–30 min |
| Caloric Testing (Warm & Cold Water in External Auditory Canal) | Vestibular system function asymmetry; detects unilateral peripheral vestibular weakness | 70–80% (high for detecting unilateral loss) | 75–85% (good when asymmetry present) | Diagnosing unilateral peripheral vestibular loss (vestibular neuritis, acoustic neuroma), documenting vestibular dysfunction | Time-consuming; uncomfortable for patient; contraindicated if eardrum perforated; does NOT diagnose BPPV; abnormal result does NOT identify specific etiology; sensitive to patient effort | None | $300–600 | 45–90 min |
| Video Head Impulse Test (vHIT) | Vestibulo-ocular reflex (VOR) gain; detects impaired eye fixation during rapid head rotation | 75–85% (high for peripheral vestibular weakness) | 78–88% (good for detecting deficit) | Quantifying peripheral vestibular weakness, differentiating central vs peripheral causes, monitoring recovery after vestibular insult | Does NOT diagnose specific underlying cause; operator and equipment dependent; requires patient cooperation and understanding; cannot visualize anatomy | None | $250–500 | 15–25 min |
| Dynamic Posturography (Computerized Balance Assessment) | Balance system integration (vestibular, visual, proprioceptive contributions); fall risk assessment | 60–70% (moderate, functional measure) | 65–75% (functional outcome variable) | Post-vestibular injury rehabilitation assessment, predicting fall risk, quantifying functional recovery, guiding therapy | Does NOT diagnose specific anatomical or vascular lesion; expensive; time-consuming; requires specialized equipment and trained technician; useful for rehabilitation tracking, not diagnosis | None | $800–1,500 | 45–60 min |
| Dix-Hallpike Maneuver (Bedside Positional Test, No Imaging) | Provokes nystagmus if posterior semicircular canal BPPV present; diagnostic and therapeutic | 90–95% (very high for posterior canal BPPV) | 92–96% (very high specificity when positive) | GOLD STANDARD for BPPV diagnosis; immediate, inexpensive, both diagnostic and therapeutic | Only tests posterior canal (accounts for ~90% of BPPV); anterior and horizontal canal BPPV require different testing; central causes can rarely mimic; requires trained examiner; nystagmus must be observed (cannot be missed) | None (bedside only) | FREE (bedside test, no cost) | 2–5 min |
| HINTS Exam (Head Impulse, Nystagmus, Test of Skew, Bedside—No Imaging) | Three rapid eye movement tests combined; superior to MRI at ruling out central causes in acute vertigo | >96% (very high for ruling out central/stroke) | >95% (very high specificity for peripheral) | SUPERIOR TO MRI for acute vertigo rule-out; 60-second bedside stroke differentiation; cost-effective screening | Requires training and experience to perform correctly; false positives with pre-existing ocular dystopia; still requires confirmatory imaging if abnormal (cannot replace MRI) | None (bedside only) | FREE (bedside test, no cost) | 1–2 min |
Key Clinical Decision Rules
For patients presenting with isolated vertigo (no trauma, no neurological symptoms):
| Clinical Scenario | Recommended First Step | Expected Sensitivity | Next Step if Negative | Approximate Timeline to Diagnosis |
|---|---|---|---|---|
| Acute vertigo, patient can tolerate positioning | Dix-Hallpike test (free, bedside) | 90–95% for posterior BPPV | If negative: HINTS exam | 5–10 min |
| Dix-Hallpike positive | Epley maneuver immediately (diagnostic + therapeutic) | — | Follow-up in 1 week if incomplete resolution | Cure often within minutes |
| Dix-Hallpike negative, but high suspicion for BPPV | Anterior/horizontal canal specific tests (Dix-Hallpike variant) or imaging | 75–85% (lateral/anterior canal) | If still negative + persistent: VNG, caloric, vHIT | 15–30 min |
| Constant vertigo (not positional) | HINTS exam (free, bedside) | >96% for ruling out stroke | If HINTS normal: Caloric, vHIT, consider MRI if persistent | 5–20 min |
| HINTS abnormal (suggests central cause) | MRI brain with DWI sequences (rule out acute stroke) | 85–95% for acute ischemia | If MRI normal: Consider vascular imaging (MRA or CTA) | 1–2 hours |
| Post-traumatic vertigo | Dix-Hallpike test first (BPPV from trauma common) | 80–85% for post-traumatic BPPV | If positive: Epley। If negative: HINTS + CT brain (if LOC or severe symptoms) | 15–30 min |
| Positional vertigo + extreme head rotation provocation | RVAO test, then dynamic angiography if positive | 60–70% (RVAO test) | Dynamic CTA or MRA to confirm BHS | 1–2 hours |
When Cervical Imaging IS Appropriate
Cervical X-ray, CT, or MRI is indicated when:
✅ Neck pain + neurological deficits (weak arm, numbness)
✅ Trauma + concern for fracture or instability
✅ Suspected vertebral artery dissection (sudden severe headache + neck pain + neurological symptoms)
✅ Myelopathy symptoms (progressive weakness, loss of fine motor control)
✅ Before planned neck surgery (for other indications)
Cervical imaging is NOT a first-line test for:
❌ Isolated vertigo without neck pain
❌ BPPV (diagnosis is clinical—Dix-Hallpike)
❌ Vestibular neuritis
❌ Acute stroke (use MRI brain, not cervical spine)
❌ Suspected Bow Hunter’s Syndrome without dynamic angiography
Red Flag Symptoms: When to Seek Urgent Imaging
| Red Flag | Concern | Action |
|---|---|---|
| Worst headache of life + vertigo | Subarachnoid hemorrhage | Emergency CT brain |
| Severe headache worsening over hours + vomiting + vertigo | Increased ICP (bleeding, edema) | Emergency CT brain |
| Vertigo + facial droop + arm weakness + speech slurred | Acute stroke (AICA or vertebrobasilar) | Emergency MRI brain + neurology |
| Loss of consciousness + vertigo + head trauma | Moderate-severe TBI | Emergency CT brain |
| Vertigo + fever + stiff neck | Meningitis or labyrinthitis | Emergency CT ± LP, antibiotics |
| Progressive vertigo + hearing loss + tinnitus over weeks | Acoustic neuroma, MS, neoplasm | MRI inner ear + brain |
| Vertigo + vision loss + eye pain | Optic neuritis (possible MS) | MRI brain + orbits |
| Vertigo only with extreme head rotation (far turn) + sustained nystagmus | Bow Hunter’s Syndrome | Dynamic angiography |
| Positional vertigo + positive Dix-Hallpike + nausea but NO neurological deficits | BPPV (low risk, treat outpatient) | Epley maneuver, no imaging needed |
Patient Handout Version
If your doctor says you have “cervical vertigo,” ask these questions:
- ✓ Did they perform the Dix-Hallpike maneuver? (If positive → BPPV, not cervical)
- ✓ Did they perform the HINTS exam? (If abnormal → needs MRI brain, not cervical)
- ✓ Did they refer to a vestibular specialist? (ENT or neuro-specialist with vestibular training)
- ❌ Did they order cervical imaging first? (If only cervical imaging done → request vestibular testing)
- ❌ Do you have a specific positional trigger? (If yes → likely BPPV, not cervical)
- ❌ Did they prescribe a neck collar? (If yes → ask for VRT instead; collars delay recovery)
If you’re told you need neck surgery for vertigo, get a second opinion from a vestibular specialist.
FAQs
ENGLISH FAQs (20 Questions)
1. What is the main difference between “cervical vertigo” and true vestibular vertigo?
Answer: “Cervical vertigo” is a poorly defined and highly controversial diagnosis. True vertigo—spinning sensation—is almost always caused by a problem in the inner ear (vestibular system) or brainstem, NOT the neck. Neck problems cause neck pain and sometimes arm pain/weakness, but the spinning sensation itself does not originate from bone spurs or cervical degeneration. Many cases labeled “cervical vertigo” are actually BPPV, vestibular neuritis, or migraine that have been misattributed to the neck based on incidental X-ray findings.
2. Why do neck X-rays show abnormal findings in most adults, yet most people don’t have vertigo?
Answer: Cervical spondylosis (bone spurs, disc space narrowing, osteophytes) is an extremely common, age-related finding—present in 70–80% of adults over 70 and 30–40% of adults in their 50s. Most of these people have NO vertigo, neck pain, or neurological symptoms whatsoever. This demonstrates that spondylosis is incidental and does not cause spinning. When a patient with spondylosis develops vertigo, the spondylosis is usually a red herring, and the true cause (BPPV, vestibular neuritis, etc.) remains undiagnosed.
3. How do I know if my vertigo is truly from BPPV and not my neck?
Answer: The Dix-Hallpike maneuver is the gold standard test. A doctor positions you upright, turns your head to one side, then rapidly lowers you backward with your head hanging. If positional vertigo is caused by BPPV (displaced inner ear crystals), you will experience nystagmus (involuntary eye movements) within 1–5 seconds, and the vertigo will last 10–60 seconds. If the test is positive, BPPV is confirmed—regardless of what your neck X-ray shows. The Epley maneuver (physical repositioning of the crystals) then provides cure in 80–90% of cases.
4. Why is immobilizing the neck with a collar counterproductive for vertigo?
Answer: The vestibular system learns and recalibrates through movement. When the head and neck are immobilized, the brain cannot update its internal model of balance based on actual head movements. This prevents natural compensation and recovery. Research shows that neck collars actually PROLONG recovery from vestibular disorders. Patients are often harmed by this treatment, which delays the correct diagnosis and true recovery.
5. Can cervical surgery cure vertigo?
Answer: In the vast majority of cases, NO. Surgical decompression of the cervical spine (ACDF, laminectomy, etc.) is a high-risk procedure that does not address the true causes of vertigo—which are almost always in the inner ear or brainstem. Even if the surgery successfully relieves cervical compression, it will NOT cure BPPV, vestibular neuritis, or migraine-related dizziness. Patients undergo surgery and still have vertigo, having incurred surgical risks for no benefit. The only exception is Bow Hunter’s Syndrome (extremely rare), where surgery may help if the correct diagnosis has been confirmed with dynamic angiography.
6. What is Bow Hunter’s Syndrome and how is it different from typical “cervical vertigo”?
Answer: Bow Hunter’s Syndrome is a rare, legitimate vascular condition where a bony spur in the cervical spine pinches the vertebral artery during head rotation, temporarily blocking blood flow to the brainstem. This causes vertigo and brainstem symptoms (diplopia, slurred speech, imbalance). However, it is exceptionally rare—perhaps 15 out of 2,000 cases labeled “cervical vertigo.” Diagnosis requires dynamic angiography (imaging during head rotation), not static X-rays. Unlike typical “cervical vertigo,” Bow Hunter’s Syndrome vertigo occurs only during extreme head rotation while upright, and nystagmus is sustained (as long as the head is held rotated).
7. How do you differentiate Bow Hunter’s Syndrome from BPPV?
Answer: Key differences: BPPV is triggered by any head movement and often occurs supine; Bow Hunter’s vertigo occurs only during extreme rotation in one direction while upright. BPPV nystagmus is brief (seconds) and fatigues; Bow Hunter’s nystagmus is sustained (as long as the head is held rotated). BPPV has no associated brainstem symptoms; Bow Hunter’s often includes diplopia, dysarthria, or drop attacks. Diagnosis: BPPV = positive Dix-Hallpike + clinical diagnosis. Bow Hunter’s = positive RVAO test + dynamic angiography confirmation.
8. What should I do if I was told I have cervical vertigo but I’m not getting better?
Answer: Request a formal vestibular evaluation. Ask your doctor to perform the Dix-Hallpike maneuver—the gold standard for diagnosing BPPV, the most common cause of vertigo. If positive, request the Epley maneuver, which is diagnostic and therapeutic. If negative, ask for the HINTS exam, a 60-second bedside test superior to MRI for ruling out a central cause (stroke). If both are negative but symptoms persist, vestibular testing (caloric testing, video head impulse test) or inner ear MRI may be appropriate. Do NOT continue indefinite neck therapy without confirmation that the neck is actually the problem.
9. Why is the Dix-Hallpike test superior to imaging for diagnosing BPPV?
Answer: The Dix-Hallpike test directly provokes the vertigo mechanism (displaced inner ear crystals moving within the semicircular canal) and is 90–95% sensitive and specific for BPPV. It takes 2–5 minutes, costs nothing, and is both diagnostic AND therapeutic (the maneuver can be immediately followed by the Epley repositioning). In contrast, X-rays, CT scans, and even MRI cannot visualize the microscopic otoconia (calcium carbonate crystals) that cause BPPV. You could have a completely normal MRI and still have BPPV that is easily cured with an Epley maneuver.
10. What is the HINTS exam and why is it better than MRI for acute vertigo?
Answer: HINTS (Head Impulse, Nystagmus, Test of Skew) is a 60-second bedside examination that differentiates central from peripheral causes of acute vertigo with >96% sensitivity and specificity for ruling out stroke. It requires NO imaging and costs nothing. In contrast, MRI takes hours, costs $1,200–2,500, and is often unavailable immediately. The HINTS exam can be performed at the bedside during initial evaluation, allowing rapid identification of central causes (stroke, tumor) that require urgent treatment, versus peripheral causes (BPPV, vestibular neuritis) that are low-risk and can be observed or treated conservatively.
11. Is it safe to treat BPPV at home with the Epley maneuver if I’ve been diagnosed positively?
Answer: If a trained healthcare provider has confirmed BPPV with a positive Dix-Hallpike test, yes—many patients successfully self-treat with the Epley maneuver after receiving instruction. However, a professional demonstration is strongly recommended for the first maneuver to ensure proper technique. Some patients require multiple maneuvers or variations (Semont maneuver) if symptoms persist. If you attempt self-treatment and symptoms worsen or do not improve within 1–2 weeks, seek professional evaluation.
12. What is post-traumatic BPPV and how does it relate to whiplash?
Answer: Whiplash involves rapid head acceleration and deceleration, which can physically dislodge the calcium carbonate crystals in the inner ear, causing BPPV. This is called post-traumatic BPPV or traumatic otolith vertigo. The patient may have both legitimate neck pain (from muscle and ligament injury) AND vertigo (from inner ear crystal dislodgement). These are separate injuries with different treatments. Treating neck pain does not treat BPPV—a Dix-Hallpike test and Epley maneuver are needed for the vertigo component.
13. What are the red flags for serious central causes of vertigo that require urgent imaging?
Answer: Seek urgent imaging (CT or MRI brain) if vertigo is associated with: sudden worst headache of life, progressive worsening, facial drooping, arm/leg weakness, speech difficulty, vision loss, loss of consciousness, fever with stiff neck, or vomiting with worsening headache. Also perform HINTS exam—if abnormal (abnormal head impulse, vertical nystagmus, or vertical eye misalignment), urgent MRI is indicated. The combination of vertigo + any of these neurological findings suggests a central cause (stroke, hemorrhage, tumor) requiring urgent evaluation.
14. Can you have both cervical spondylosis AND BPPV at the same time?
Answer: Yes, absolutely. Many older adults have age-related cervical spondylosis (common and usually asymptomatic) AND separate BPPV unrelated to the neck. The problem is that when both are present, clinicians may incorrectly assume they are related, attributing the vertigo to the spondylosis. This leads to inappropriate neck therapy while BPPV goes untreated. The solution: If a patient with known spondylosis develops vertigo, perform the Dix-Hallpike test to assess for BPPV independently. If Dix-Hallpike is positive, treat the BPPV with an Epley maneuver, regardless of spondylosis findings.
15. What is the role of vestibular rehabilitation therapy (VRT) in treating vertigo from peripheral vestibular causes?
Answer: VRT is an exercise-based program that retrains the brain’s balance mechanisms when peripheral vestibular function is damaged or lost (e.g., vestibular neuritis, post-BPPV residual imbalance). Specific exercises promote “habituation” (decreased response to dizziness triggers) and “compensation” (relying more on visual and proprioceptive input and less on damaged vestibular signals). VRT is particularly effective for persistent imbalance after acute vestibular events and improves outcomes in 60–80% of patients. VRT is NOT a treatment for BPPV itself (which is cured by Epley maneuver), but it may help residual imbalance if symptoms persist.
16. How does post-concussion vertigo differ from BPPV after a head injury?
Answer: Post-traumatic BPPV (from crystal dislodgement) is triggered by specific head positions and can be cured with the Epley maneuver. Post-concussion vertigo (from brainstem concussive injury) is continuous or triggered by head movement generally (not position-specific) and is associated with other concussion symptoms (headache, cognitive fog, photophobia, phonophobia). Post-concussion vertigo recovers gradually over weeks to months with vestibular rehabilitation, whereas post-traumatic BPPV often resolves quickly with the Epley maneuver. A positive Dix-Hallpike suggests post-traumatic BPPV; a negative Dix-Hallpike + continuous symptoms suggests post-concussion vertigo.
17. Can vertebrobasilar insufficiency cause vertigo, and how is it diagnosed?
Answer: Yes, insufficient blood flow through the vertebrobasilar arteries (vertebral and basilar) can cause vertigo and brainstem symptoms. However, it is controversial and often overdiagnosed in patients labeled with “cervical vertigo.” True vertebrobasilar insufficiency typically causes additional brainstem signs (diplopia, weakness, speech difficulty), not isolated vertigo. Static imaging (X-rays, standard MRA) cannot diagnose functional vascular insufficiency. Dynamic angiography (imaging during head movements) can show temporary occlusion during extreme rotation (Bow Hunter’s Syndrome). Isolated vertigo without other brainstem signs is rarely due to vascular insufficiency alone.
18. What is the relationship between vestibular migraine and “cervical vertigo”?
Answer: Vestibular migraine can mimic “cervical vertigo” because head movements (which necessarily involve the neck) can trigger migraine-related dizziness. However, vestibular migraine is triggered by migraine mechanisms (neuronal hyperexcitability, spreading depression), not by mechanical cervical pathology. Patients with vestibular migraine benefit from migraine-specific preventative medications, VRT, and cognitive behavioral therapy—NOT neck treatments. If a patient is diagnosed with “cervical vertigo” but has a history of migraines or associated headache/photophobia/phonophobia, the true diagnosis may be vestibular migraine rather than cervical disease.
19. Should I get cervical imaging if I have persistent vertigo?
Answer: Not as a first-line test. If you have isolated vertigo (spinning sensation without neck pain, weakness, or neurological symptoms), cervical imaging is unlikely to reveal the cause. Instead, start with: (1) detailed history and physical exam, (2) Dix-Hallpike test (if positional vertigo suspected), (3) HINTS exam (if continuous vertigo suspected). If HINTS is abnormal, MRI brain (not cervical spine) is indicated to rule out stroke. Cervical imaging is appropriate ONLY if: neck pain + neurological symptoms (weakness, numbness), trauma with concern for fracture, or suspected vertebral artery dissection (with sudden pain + neurological signs).
20. If my vertigo doesn’t respond to standard treatments, what should I do?
Answer: Ensure the diagnosis is correct: (1) Ask for Dix-Hallpike test + HINTS exam if not already done. (2) If BPPV is confirmed but Epley didn’t work, try again or see a physical therapist for additional maneuvers (Semont, Gans). (3) If a clear diagnosis hasn’t been established, request referral to a vestibular specialist (ENT or neurologist with vestibular training). (4) Request vestibular-specific testing: caloric test, video head impulse test, posturography, or inner ear MRI. (5) Consider secondary diagnoses (vestibular migraine, Menière’s disease, demyelinating disease) if primary peripheral causes are ruled out. Persistent symptoms without a confirmed diagnosis warrant specialist evaluation, NOT indefinite nonspecific treatment.
HINGLISH FAQs (20 Questions)
1. “Cervical vertigo” aur true vestibular vertigo mein kya difference hai?
Answer: “Cervical vertigo” = poorly defined, controversial diagnosis। True vertigo (spinning) = almost always inner ear या brainstem, NOT neck। Neck problems = neck pain + arm pain/weakness; lekin spinning sensation nahi। Many “cervical vertigo” cases = actually BPPV, vestibular neuritis, migraine jo neck X-ray mein incidental spondylosis se misattribute हो गए।
2. Kyun sabke neck X-rays abnormal dikhti hain lekin vertigo nahi hai?
Answer: Cervical spondylosis (bone spurs, disc narrowing) = super common, age-related। 70–80% adults 70+ में = present। 30–40% adults 50s में = present। Most = NO vertigo, no pain, no symptoms। Proves spondylosis = incidental, no cause vertigo। Patient + spondylosis + vertigo = usually true cause (BPPV, neuritis) undiagnosed!
3. Kaise pata chalega mera vertigo BPPV hai, neck se nahi?
Answer: Dix-Hallpike test = gold standard। Doctor = head turn, then rapid lower backward। BPPV positive = nystagmus in 1–5 sec, spinning 10–60 sec। Positive = BPPV confirmed (regardless of neck X-ray!)। Epley maneuver = cure 80–90% cases।
4. Kyun neck collar immobilize करने से vertigo worse हो जाता है?
Answer: Vestibular system = movement से सीखता है। Immobilize = no learning = no compensation = persistent dizziness। Research = neck collars actually PROLONG recovery! Patient = harmed, correct diagnosis delayed, true recovery blocked।
5. Kya cervical surgery = vertigo cure कर सकता है?
Answer: Majority = NO। Surgery (ACDF, laminectomy) = high-risk lekin BPPV, neuritis, migraine address नहीं करता। Even successful surgery = still dizzy + surgical risks! Exception = Bow Hunter’s Syndrome (extremely rare, confirmed with dynamic angiography)।
6. Bow Hunter’s Syndrome kya hai aur typical “cervical vertigo” से alag kyun?
Answer: Bow Hunter’s = rare, legitimate vascular। Bony spur pinches vertebral artery during head rotation → blood flow blocked → brainstem ischemic → vertigo + brainstem symptoms (diplopia, slurred speech)। Extremely rare (15 out of 2,000 “cervical vertigo”)। Diagnosis = dynamic angiography (NOT static X-ray)। Vertigo = केवल extreme rotation, upright, नystagmus sustained।
7. Bow Hunter’s और BPPV में differentiate कैसे करते हो?
Answer: BPPV = any head movement, often supine, brief nystagmus, no brainstem symptoms। Bow Hunter’s = extreme rotation केवल एक direction, upright, sustained nystagmus, often diplopia/dysarthria/drop attacks। Diagnosis: BPPV = Dix-Hallpike। Bow Hunter’s = RVAO test + dynamic angiography।
8. Agar mujhe cervical vertigo बताया गया है लेकिन improve नहीं हो रहा?
Answer: Request vestibular evaluation। Ask for Dix-Hallpike (gold standard BPPV)। Positive = Epley maneuver। Negative = HINTS exam (better than MRI, 60-second stroke rule-out)। Both negative + persistent = vestibular testing या inner ear MRI। Don’t continue indefinite neck therapy without confirmation neck = problem।
9. Kyun Dix-Hallpike imaging से better है BPPV diagnose करने के लिए?
Answer: Dix-Hallpike = directly provokes vertigo (displaced crystals moving)। 90–95% sensitive/specific। 2–5 min, FREE, diagnostic + therapeutic (immediately Epley do सकते हो)। X-ray/CT/MRI = cannot see otoconia (too small)। Normal MRI + positive Dix-Hallpike = BPPV, treatable with Epley!
10. HINTS exam kya है aur MRI से better kyun?
Answer: HINTS = 3 rapid eye tests, 60 seconds, bedside, FREE। >96% sensitivity stroke rule-out। MRI = hours, $1,200–2,500, often unavailable immediately। HINTS = immediate central vs peripheral differentiate। Central abnormal = urgent MRI। Peripheral normal = safe observation/VRT।
11. Kya safe है self-treat BPPV घर पे Epley से?
Answer: Agar professional = confirmed BPPV with positive Dix-Hallpike, हाँ—बहुत patients self-treat after instruction। Professional demonstration = first time recommended। Persistent symptoms = PT visit या repeat maneuver। Worse = seek evaluation immediately।
12. Post-traumatic BPPV kya hai aur whiplash से connection?
Answer: Whiplash = head acceleration/deceleration → crystals dislodge → BPPV। Patient = both legitimate neck pain (muscles/ligaments) AND vertigo (inner ear)। Separate injuries! Neck treatment ≠ BPPV cure। Dix-Hallpike + Epley = correct treatment for spinning।
13. Red flags कौन हैं serious central causes के लिए?
Answer: Urgent imaging (CT/MRI) if: worst headache ever, worsening, facial drop, arm/leg weakness, speech difficulty, vision loss, LOC, fever + stiff neck, vomiting + worsening। HINTS abnormal (abnormal head impulse, vertical nystagmus, skew) = urgent MRI। Vertigo + neuro signs = central (stroke, bleed, tumor)।
14. Kya simultaneously cervical spondylosis AND BPPV हो सकता है?
Answer: हाँ, absolutely! Elderly = common spondylosis (usually asymptomatic) AND separate BPPV। Problem = clinicians मानते हैं related, wrongly attribute vertigo to spondylosis। Solution: Dix-Hallpike perform करो। Positive = treat BPPV with Epley (regardless of spondylosis)।
15. VRT (Vestibular Rehabilitation Therapy) का role क्या है?
Answer: VRT = exercise program जो brain के balance mechanisms को retrain करता है। Habituation (dizziness triggers को decrease response) + compensation (visual/proprioceptive reliance increase)। Peripheral vestibular loss के लिए effective। 60–80% improvement। BPPV के लिए NOT (Epley cure करता है) lekin residual imbalance में helps।
16. Post-concussion vertigo BPPV post-trauma से कैसे अलग?
Answer: Post-traumatic BPPV (crystals) = position-triggered, Epley से cure। Post-concussion (brainstem injury) = continuous/general head movement triggered, associated symptoms (headache, cognitive fog, photophobia)। Recovery = weeks–months with VRT। Positive Dix-Hallpike = post-traumatic BPPV। Negative + continuous = post-concussion।
17. Kya vertebrobasilar insufficiency vertigo cause कर सकता है?
Answer: Hाँ, but often overdiagnosed in “cervical vertigo”। True = additional brainstem signs (diplopia, weakness, speech)। Static imaging = cannot diagnose। Dynamic angiography = functional occlusion show कर सकता है (Bow Hunter’s)। Isolated vertigo + no brainstem signs = rarely vascular alone।
18. Vestibular migraine aur “cervical vertigo” relationship?
Answer: Vestibular migraine = head movements (neck से) trigger कर सकते हैं migraine dizziness। But mechanism = migraine (neuronal, NOT mechanical cervical)। Treatment = migraine preventatives, VRT, CBT (NOT neck treatment)। History of migraine + headache/photophobia/phonophobia = vestibular migraine, NOT cervical!
19. Kya persistent vertigo के लिए cervical imaging लूँ?
Answer: NOT first-line। Isolated vertigo (no neck pain/weakness/neuro) = cervical imaging unlikely helpful। Start: history + Dix-Hallpike (positional) + HINTS (continuous)। HINTS abnormal = MRI brain (not cervical spine)। Cervical imaging = केवल if neck pain + neuro symptoms, trauma, या vertebral artery dissection suspected।
20. Agar standard treatments से vertigo respond नहीं हो रहा?
Answer: Ensure correct diagnosis: Dix-Hallpike + HINTS if not done। BPPV confirmed + Epley failed = repeat या PT। No clear diagnosis = specialist referral (ENT/neuro vestibular)। Request: caloric, vHIT, posturography, inner ear MRI। Consider secondary: migraine, Menière’s, demyelinating। Persistent = specialist, NOT indefinite nonspecific treatment।
HINDI FAQs (20 Questions)
1. “Cervical vertigo” और true vestibular vertigo में क्या अंतर है?
Answer: “Cervical vertigo” = poorly defined, controversial diagnosis। True vertigo (spinning) = लगभग हमेशा inner ear या brainstem, NOT neck। Neck problems = neck pain + arm pain/weakness; लेकिन spinning sensation नहीं। Many “cervical vertigo” cases = actually BPPV, vestibular neuritis, migraine जो neck X-ray में incidental spondylosis से misattribute हो गए।
2. क्यों सब के neck X-rays abnormal दिखती हैं लेकिन vertigo नहीं है?
Answer: Cervical spondylosis (bone spurs, disc narrowing) = super common, age-related। 70–80% adults 70+ में = present। 30–40% adults 50s में = present। Most = NO vertigo, कोई pain नहीं, कोई symptoms नहीं। Proves spondylosis = incidental, vertigo का कारण नहीं। Patient + spondylosis + vertigo = आमतौर पर true cause (BPPV, neuritis) undiagnosed!
3. कैसे पता चलेगा मेरा vertigo BPPV है, neck से नहीं?
Answer: Dix-Hallpike test = gold standard। Doctor = head turn, फिर तेजी से पीछे lower करो। BPPV positive = nystagmus in 1–5 sec, spinning 10–60 sec। Positive = BPPV confirmed (regardless of neck X-ray!)। Epley maneuver = cure 80–90% cases।
4. क्यों neck collar से immobilization करने से vertigo worse हो जाता है?
Answer: Vestibular system = movement से सीखता है। Immobilize = कोई learning नहीं = कोई compensation नहीं = persistent dizziness। Research = neck collars actually PROLONG recovery! Patient = harmed, correct diagnosis delayed, true recovery blocked।
5. क्या cervical surgery vertigo को cure कर सकता है?
Answer: बहुत सारे cases में = नहीं। Surgery (ACDF, laminectomy) = high-risk लेकिन BPPV, neuritis, migraine को address नहीं करता। Even successful surgery = still dizzy + surgical risks! Exception = Bow Hunter’s Syndrome (extremely rare, dynamic angiography से confirmed)।
6. Bow Hunter’s Syndrome क्या है और typical “cervical vertigo” से अलग क्यों?
Answer: Bow Hunter’s = rare, legitimate vascular। Bony spur pinches vertebral artery during head rotation → blood flow blocked → brainstem ischemic → vertigo + brainstem symptoms (diplopia, slurred speech)। Extremely rare (15 out of 2,000 “cervical vertigo”)। Diagnosis = dynamic angiography (NOT static X-ray)। Vertigo = केवल extreme rotation, upright, sustained nystagmus।
7. Bow Hunter’s और BPPV में differentiate कैसे करते हो?
Answer: BPPV = any head movement, often supine, brief nystagmus, कोई brainstem symptoms नहीं। Bow Hunter’s = extreme rotation केवल एक direction, upright, sustained nystagmus, often diplopia/dysarthria/drop attacks। Diagnosis: BPPV = Dix-Hallpike। Bow Hunter’s = RVAO test + dynamic angiography।
8. अगर मुझे cervical vertigo बताया गया है लेकिन सुधार नहीं हो रहा?
Answer: Request vestibular evaluation। Ask for Dix-Hallpike (gold standard BPPV)। Positive = Epley maneuver। Negative = HINTS exam (better than MRI, 60-second stroke rule-out)। Both negative + persistent = vestibular testing या inner ear MRI। Don’t continue indefinite neck therapy बिना confirmation के कि neck = problem।
9. क्यों Dix-Hallpike imaging से बेहतर है BPPV diagnose करने के लिए?
Answer: Dix-Hallpike = directly provokes vertigo (displaced crystals moving)। 90–95% sensitive/specific। 2–5 min, FREE, diagnostic + therapeutic (immediately Epley कर सकते हो)। X-ray/CT/MRI = cannot see otoconia (बहुत छोटे)। Normal MRI + positive Dix-Hallpike = BPPV, Epley से treatable!
10. HINTS exam क्या है और MRI से बेहतर क्यों है?
Answer: HINTS = 3 rapid eye tests, 60 seconds, bedside, FREE। >96% sensitivity stroke rule-out। MRI = hours, $1,200–2,500, often immediately unavailable। HINTS = immediate central vs peripheral differentiate। Central abnormal = urgent MRI। Peripheral normal = safe observation/VRT।
11. क्या safe है self-treat करना BPPV को घर पर Epley से?
Answer: अगर professional ने confirmed BPPV with positive Dix-Hallpike, हाँ—बहुत patients self-treat करते हैं instruction के बाद। Professional demonstration = पहली बार recommended। Persistent symptoms = PT visit या repeat maneuver। Worse = immediately seek evaluation।
12. Post-traumatic BPPV क्या है और whiplash से connection?
Answer: Whiplash = head acceleration/deceleration → crystals dislodge → BPPV। Patient = both legitimate neck pain (muscles/ligaments) AND vertigo (inner ear)। Separate injuries! Neck treatment ≠ BPPV cure। Dix-Hallpike + Epley = correct treatment spinning के लिए।
13. Red flags कौन हैं serious central causes के लिए?
Answer: Urgent imaging (CT/MRI) if: worst headache ever, worsening, facial drop, arm/leg weakness, speech difficulty, vision loss, LOC, fever + stiff neck, vomiting + worsening। HINTS abnormal (abnormal head impulse, vertical nystagmus, skew) = urgent MRI। Vertigo + neuro signs = central (stroke, bleed, tumor)।
14. क्या simultaneously cervical spondylosis AND BPPV हो सकता है?
Answer: हाँ, absolutely! Elderly = common spondylosis (usually asymptomatic) AND separate BPPV। Problem = clinicians मानते हैं related, wrongly attribute vertigo को spondylosis से। Solution: Dix-Hallpike perform करो। Positive = treat BPPV with Epley (regardless of spondylosis)।
15. VRT (Vestibular Rehabilitation Therapy) की भूमिका क्या है?
Answer: VRT = exercise program जो brain के balance mechanisms को retrain करता है। Habituation (dizziness triggers को decrease response) + compensation (visual/proprioceptive reliance increase)। Peripheral vestibular loss के लिए effective। 60–80% improvement। BPPV के लिए NOT (Epley cure करता है) लेकिन residual imbalance में helps।
16. Post-concussion vertigo BPPV post-trauma से कैसे अलग है?
Answer: Post-traumatic BPPV (crystals) = position-triggered, Epley से cure। Post-concussion (brainstem injury) = continuous/general head movement triggered, associated symptoms (headache, cognitive fog, photophobia)। Recovery = weeks–months with VRT। Positive Dix-Hallpike = post-traumatic BPPV। Negative + continuous = post-concussion।
17. क्या vertebrobasilar insufficiency vertigo cause कर सकता है?
Answer: हाँ, लेकिन अक्सर “cervical vertigo” में overdiagnosed। True = additional brainstem signs (diplopia, weakness, speech)। Static imaging = cannot diagnose। Dynamic angiography = functional occlusion show कर सकता है (Bow Hunter’s)। Isolated vertigo + कोई brainstem signs नहीं = rarely vascular alone।
18. Vestibular migraine और “cervical vertigo” का relationship?
Answer: Vestibular migraine = head movements (neck से) trigger कर सकते हैं migraine dizziness। But mechanism = migraine (neuronal, NOT mechanical cervical)। Treatment = migraine preventatives, VRT, CBT (NOT neck treatment)। History of migraine + headache/photophobia/phonophobia = vestibular migraine, NOT cervical!
19. क्या persistent vertigo के लिए cervical imaging लूँ?
Answer: NOT first-line। Isolated vertigo (कोई neck pain/weakness/neuro नहीं) = cervical imaging unlikely helpful। Start: history + Dix-Hallpike (positional) + HINTS (continuous)। HINTS abnormal = MRI brain (not cervical spine)। Cervical imaging = केवल अगर neck pain + neuro symptoms, trauma, या vertebral artery dissection suspected।
20. अगर standard treatments से vertigo respond नहीं हो रहा?
Answer: Ensure correct diagnosis: Dix-Hallpike + HINTS if not done। BPPV confirmed + Epley failed = repeat या PT। कोई clear diagnosis नहीं = specialist referral (ENT/neuro vestibular)। Request: caloric, vHIT, posturography, inner ear MRI। Consider secondary: migraine, Menière’s, demyelinating। Persistent = specialist, NOT indefinite nonspecific treatment।
📞 PRIME ENT CENTER CONTACT INFORMATION
Dr. Prateek Porwal, MBBS, MS, DNB, CAMVD (Yenepoya)
Senior ENT Specialist | Vestibular Disorders & Neuro-Otology
University Certified Neurotologist (India)
11 Years of Clinical Experience
PRIME ENT Center
Clinic Location:
Nagheta Road, Near Income Tax Office
Jindpeer Chauraha, Hardoi
Uttar Pradesh 241001, India
Contact Details:
- Phone: +91 73930 62200
- Email: primeenthdi@gmail.com
- Website: https://primeentcenter.in
Consultation Timings:
- Monday to Saturday: 11:00 AM–04:00 PM | 06:00 PM–08:00 PM
- Sunday: Closed
- Emergency Services: Available through main contact number
Why Choose PRIME ENT Center for Vertigo & Balance Disorders?
✓ Specialist-Led Vestibular Evaluation – Diagnosis in a single visit using gold-standard bedside tests (Dix-Hallpike, HINTS exam)
✓ In-Office Diagnostic Testing – Comprehensive vestibular assessment without unnecessary imaging
✓ Evidence-Based Treatment Protocols – Epley maneuver, vestibular rehabilitation, preventative medication management, CGRP therapy coordination
✓ Advanced Imaging Coordination – Direct access to high-resolution MRI, CT, dynamic angiography through trusted partner centers
✓ Comprehensive 4-Step Management – Lifestyle optimization + prophylactic medications + vestibular rehabilitation + psychological support
✓ 3-Language Care – English, Hindi, Hinglish patient education and counseling
✓ Telehealth Consultations Available – Follow-up appointments and second opinions via secure video consultation
✓ Patient Education Focus – Detailed diagnostic explanations, downloadable resources, personalized treatment plans
Book Your Consultation Today
For appointments, vestibular assessment, second opinions, or urgent vertigo concerns:
📱 Call: +91 73930 62200
💬 WhatsApp: +91 73930 62200
📧 Email: primeenthdi@gmail.com
🌐 Website: https://primeentcenter.in
What to Bring to Your Appointment
- Previous Medical Imaging: X-rays, CT scans, MRI reports (if available)
- Complete Medication List: All current medications, supplements, dosages
- Symptom Diary or Tracking Sheet: If available from previous tracking (see downloadable resources)
- Insurance Information: Insurance card and coverage details
- Referral Letter: From your primary care doctor (if applicable)
- Medical History Summary: Recent illnesses, surgeries, hospitalizations
About Dr. Prateek Porwal
Dr. Prateek Porwal is a highly experienced, board-certified ENT specialist with advanced training in vestibular disorders, neuro-otology, and balance medicine. With over 11 years of dedicated clinical practice, Dr. Porwal brings expertise in diagnostic vestibular testing, evidence-based treatment protocols, and patient education to every consultation.
Key Qualifications:
- MBBS – Bachelor of Medicine, Bachelor of Surgery
- MS (ENT) – Master of Surgery, Otorhinolaryngology
- DNB – Diplomate of National Board, ENT
- CAMVD (Yenepoya) – Certificate in Advanced Mastoid and Vestibular Disorders
- University Certified Neurotologist (India) – Specialized certification in vestibular neurology and inner ear pathophysiology
Dr. Porwal has successfully diagnosed and managed thousands of patients with spinning vertigo, dizziness, balance disorders, and associated complications. His practice combines rigorous clinical assessment, advanced diagnostic testing, and the latest therapeutic innovations (including CGRP monoclonal antibodies for vestibular migraine) with a commitment to patient education and informed decision-making.
Common Conditions Treated at PRIME ENT Center
✓ BPPV (Benign Paroxysmal Positional Vertigo)
✓ Vestibular Neuritis
✓ Vestibular Migraine
✓ Menière’s Disease
✓ Persistent Postural-Perceptual Dizziness (PPPD)
✓ Post-Traumatic Vertigo (Whiplash, TBI)
✓ Mal de Debarquement Syndrome
✓ Bilateral Vestibular Hypofunction
✓ Acoustic Neuroma
✓ Superior Semicircular Canal Dehiscence
✓ Vertigo Related to Hearing Loss
✓ Age-Related Balance Disorders
Stop guessing about your vertigo. Get a definitive diagnosis and proven treatment today. Contact PRIME ENT Center.
