Spinning migraine causes are often misunderstood, leading to ineffective treatments.TL;DR: Vestibular migraine is a spinning form of migraine where vertigo and imbalance are often more disabling than the headache, and standard pain drugs like triptans frequently fail to control the dizziness. Effective treatment usually needs a 4‑pillar plan: strict trigger and diet control, daily preventive migraine medicines (including newer CGRP therapies when needed), customized vestibular rehabilitation, and psychological support such as CBT to retrain the brain’s balance and pain networks. For patients in Hardoi, working with a vertigo‑focused migraine specialist allows this full protocol to be tailored to your specific triggers, comorbid anxiety, and lifestyle so that attacks become shorter, less intense, and less frightening over time
External Resources & References
For further reading on vestibular migraine and related conditions, please refer to these authoritative medical resources:
- Bárány Society – Official organization for otosurgery and neurotology: https://www.otoneurology.org/
- International Headache Society / IHS Classification: https://www.ichd-3.org/
- American Academy of Neurology (AAN) Migraine Guidelines: https://www.aan.com/
- Mayo Clinic – Vestibular Migraine Information: https://www.mayoclinic.org/
- NIH/PubMed Central – Vestibular Migraine Research: https://pubmed.ncbi.nlm.nih.gov/
- Vestibular Disorders Association (VeDA): https://vestibular.org/
These resources provide evidence-based information on vestibular migraine pathophysiology, diagnosis, and treatment options recommended by leading international organizations.
ENGLISH VERSION
The Migraine That Spins: Why Headache Medications Fail (And What Actually Works)
Understanding Vestibular Migraine: A Hidden Epidemic
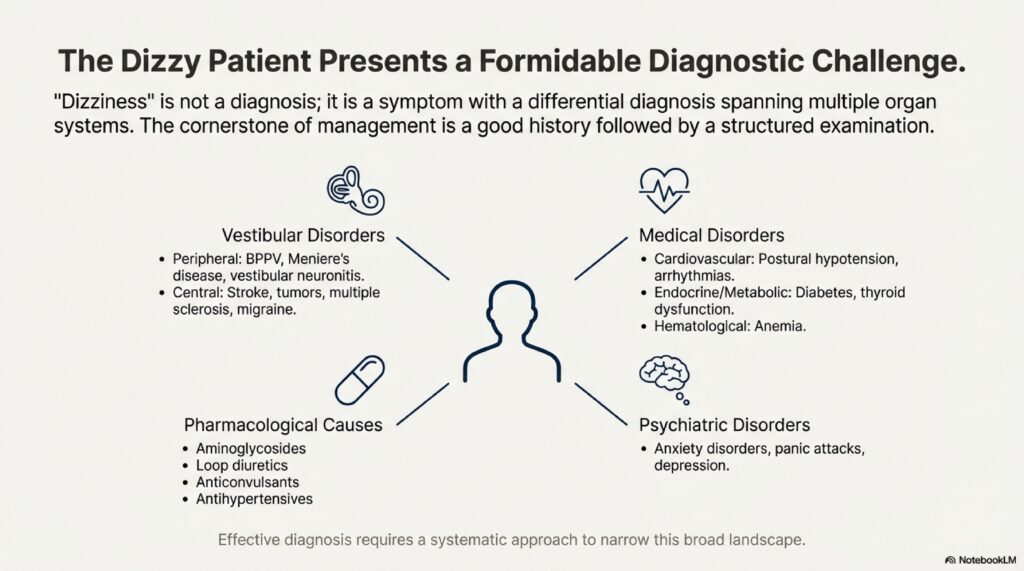
Dizziness and balance disorders are among the most common reasons patients seek medical advice, yet they remain some of the most misunderstood conditions in modern medicine. For millions of people worldwide, a migraine is not just a severe headache; it is a violent, spinning experience known as vestibular migraine (VM).
This condition is now recognized as the second most common cause of recurrent vertigo, affecting approximately 1% of the general population (though some estimates suggest higher prevalence in patients who visit balance clinics). Despite its prevalence, patients often find that standard headache treatments—triptans, NSAIDs, even opioids—do little to stop the world from spinning. This creates a frustrating cycle: the patient endures days of disability while conventional medications fail, leaving them confused about why treatments that work for regular migraines are ineffective for their dizziness.
This article explores the unique nature of the “spinning migraine,” why traditional approaches fail, and the multidisciplinary strategies that actually provide relief.
What is Vestibular Migraine?
Diagnostic Criteria: Moving Beyond the Headache-Centric Definition
Vestibular migraine is a specialized form of migraine where the primary symptoms are balance-related rather than pain-centered. This is the critical distinction that most physicians and patients miss.
The Bárány Society and the International Headache Society have established strict diagnostic criteria to help clinicians identify this elusive disorder. To be diagnosed with definite vestibular migraine, a patient must meet the following criteria:
- At least five episodes of vestibular symptoms of moderate or severe intensity
- Duration: Symptoms lasting between 5 minutes and 72 hours
- Migraine history: Current or past history of migraine with or without aura
- Migrainous features: At least one migrainous feature during at least 50% of the vertigo episodes
Migrainous features include:
- Photophobia (sensitivity to light)
- Phonophobia (sensitivity to sound)
- Visual aura (flashing lights, zigzag patterns)
- Headache (though notably absent in up to 30% of VM attacks)
- Nausea or vomiting
The Diversity of Vestibular Migraine Presentations
Remarkably, vestibular migraine presents in four distinct clinical subtypes, and many patients cycle through multiple types throughout their lives:
Type 1: Spontaneous Vertigo
- Patient feels they are spinning while sitting perfectly still
- Often the most distressing form because there is no obvious environmental trigger
- Can last from 5 minutes to days
- May be accompanied by nausea so severe the patient cannot stand
Type 2: Positional Vertigo
- Triggered by specific head movements (rolling in bed, tilting head back)
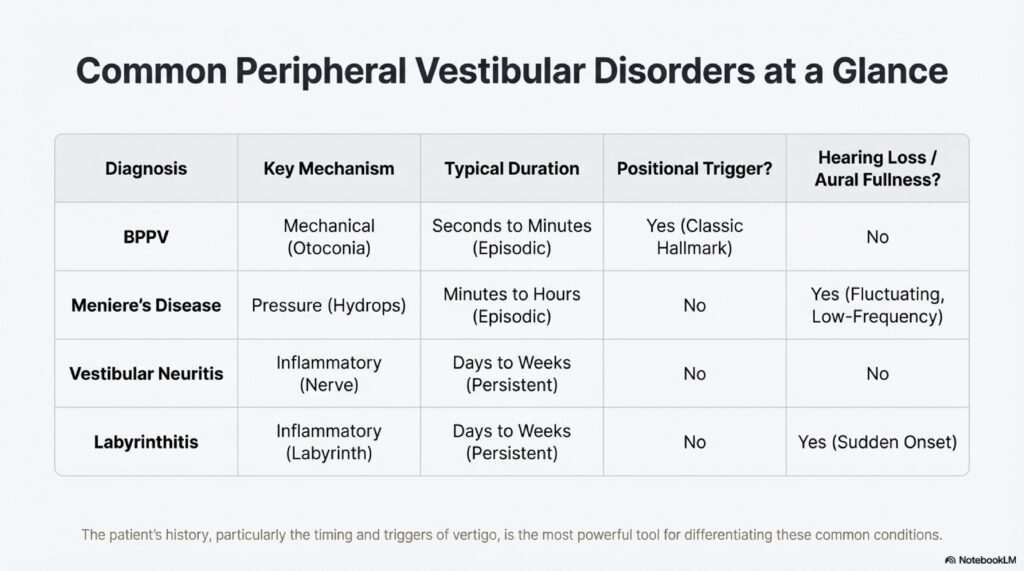
- Can mimic BPPV (Benign Paroxysmal Positional Vertigo), leading to misdiagnosis
- Unlike BPPV, the vertigo in VM is often longer-lasting (minutes to hours, not seconds)
- May occur in clusters (repeated episodes over hours or days)
Type 3: Head-Motion Dizziness
- A distorted sensation of spatial orientation during self-motion
- Patient feels “off-balance” or as if the floor is tilting while walking or moving the head
- Particularly disabling because it prevents normal daily activities like walking, driving, or exercise
Type 4: Visual Vertigo (Visual Dependence)
- Symptoms triggered by complex or moving visual environments
- Classic triggers: busy supermarket aisles, escalators, striped patterns, moving cars
- Watching action movies or scrolling through social media can provoke attacks
- Often overlooked because patients don’t link environmental visuals to their dizziness
The Science of the Spin: Why Vestibular Migraine Feels Different
The Neurobiological Basis: Beyond Simple Pain
The reason vestibular migraine is so disorienting—and why it responds differently to medications—lies in how it affects the brain’s processing centers.
Standard Migraines primarily involve:
- The trigeminovascular system (trigeminal nerve + blood vessel interactions)
- Release of CGRP (calcitonin gene-related peptide) and other inflammatory mediators
- Activation of pain pathways in the thalamus and cortex
- Result: severe headache, photophobia, nausea
Vestibular Migraines involve a broader activation:
- The vestibular nuclei in the brainstem (balance processing centers)
- The cerebellum (coordination and fine-tuning of balance)
- The vestibular cortex in the temporal lobe (perception of motion and spatial orientation)
- The visual-vestibular integration pathways (how the brain combines eye and balance signals)
- Result: vertigo, imbalance, visual disturbances, and sometimes headache
Three Leading Theories of Vestibular Migraine Pathophysiology
Theory 1: Cortical Spreading Depression
The most accepted theory suggests that vestibular migraine involves a “spreading depression” of neuronal activity that cascades across the brain.
- In regular migraines, spreading depression occurs in the cortex, causing the aura (visual symptoms) and triggering trigeminal activation
- In VM, this wave of reduced neuronal activity spreads to include the vestibular cortex and cerebellar regions
- As neural activity “quiets down,” the brain loses its ability to integrate balance signals properly, leading to vertigo
- This explains why VM attacks can last hours to days—the spreading depression is slower to resolve than in typical migraines
Theory 2: Vasospasm of the Internal Auditory Artery
An alternative theory proposes that the internal auditory artery (IAA), which supplies blood to the inner ear and portions of the brainstem, may undergo vasospasm (temporary narrowing).
- This leads to transient dysfunction of the vestibular sensors and balance processing centers
- The attack resolves as blood flow is restored
- This theory would explain why some VM patients experience sudden hearing loss during an attack—a symptom that overlaps with another condition, sudden sensorineural hearing loss (SSNHL)
- However, this theory is less widely accepted because most VM patients do not have confirmed vasospasm on imaging
Theory 3: Channelopathy (Ion Channel Dysfunction)
Emerging evidence suggests that some patients with VM may have a genetic defect in ion channels—the cellular “gates” that regulate how nerves fire.
- Mutations in potassium or calcium channels can make neurons hyperexcitable
- This “hyperexcitability” lowers the threshold for migraine activation
- In these patients, vestibular neurons are particularly sensitive to triggering stimuli
- This explains why some families have multiple members with VM (genetic predisposition)
- It also explains why some VM patients respond to anticonvulsants (which stabilize ion channels) when other medications fail
The Signal-to-Noise Problem
Imagine a radio receiver in a noisy room. When the radio works properly, it filters out background noise and focuses on the signal. In vestibular migraine, the brain’s ability to filter out irrelevant balance information becomes impaired. The signal-to-noise ratio becomes permanently altered, making the brain hypersensitive to:
- Normal head movements
- Visual motion
- Changes in body position
- Even subtle shifts in air pressure or temperature
This is why VM patients often report that triggers become more sensitive over time and why environmental modifications (staying in quiet, dimly lit spaces) provide temporary relief.
Why Standard Headache Medications Often Fail in Vestibular Migraine
Understanding the failures of conventional migraine treatments is crucial to appreciating why a different approach is needed.
Reason 1: The Timing Mismatch
Traditional migraine auras (visual symptoms, tingling) typically last between 5 and 60 minutes. Vestibular symptoms in VM can persist for days or even weeks.
- Triptans and other abortive medications are designed for short bursts of pain (3-24 hours)
- When taken during a VM attack, they may abort the headache component (if present) but leave the vertigo untouched
- The patient experiences “partial relief”—the head pain resolves, but the world continues spinning
- By the time the patient realizes the triptan didn’t work on the dizziness, the medication has already been absorbed and metabolized
Clinical Example: A patient takes sumatriptan at the onset of a migraine. The headache resolves within 30 minutes. However, the vertigo that began simultaneously persists for 3 more days. The patient attributes this to “incomplete response” when, in fact, they needed a different medication strategy.
Reason 2: Lack of Specific Vestibular Evidence in Clinical Trials
Most major clinical trials for migraine medications—including trials for triptans, beta-blockers, and anticonvulsants—focused on headache reduction as the primary outcome measure.
- Researchers measured pain scores, photophobia, nausea
- Few trials specifically measured vertigo severity or balance function
- While triptans are excellent at constricting blood vessels and stopping head pain, their effect on the complex neuronal “overdrive” in the vestibular system remains unclear and often inconclusive
- This creates a treatment gap: medications are approved for migraine but never tested for vestibular symptoms specifically
Reason 3: The Absorption Problem
VM attacks are frequently accompanied by severe nausea and vomiting, which disrupts normal stomach function.
- Gastric motility (the stomach’s ability to move food and medication forward) decreases dramatically during a vestibular migraine attack
- A patient swallows a pill during an attack hoping for relief, but the medication sits in the stomach and never gets absorbed
- By the time nausea subsides (hours or days later), the acute attack has already passed
- The patient concludes the medication “didn’t work” when, in fact, it was never absorbed
This is why rescue medications for VM are increasingly prescribed as:
- Suppositories (absorbed through rectal tissue, bypassing the stomach)
- Nasal sprays (absorbed through nasal mucosa, rapid onset)
- Subcutaneous injections (injected directly under the skin for immediate delivery)
Reason 4: Misdiagnosis Leading to Wrong Treatment
Because vestibular migraine can mimic other conditions, patients often receive the wrong diagnosis and therefore the wrong treatment.
Example 1: BPPV Misdiagnosis
- Patient presents with positional vertigo lasting hours
- Doctor performs the Dix-Hallpike test (positive result)
- BPPV is assumed, Epley maneuver is performed
- The Epley maneuver may provide temporary relief (due to placebo effect or concurrent resolution of the migraine) but doesn’t address the underlying migraine
- Attack recurs days later; patient is told to repeat the Epley maneuver
- Correct treatment (preventative migraine medication) is never started
Example 2: Menière’s Disease Misdiagnosis
- Patient experiences attacks of vertigo + hearing loss + tinnitus
- Doctor assumes Menière’s disease and recommends salt restriction
- Patient follows a strict low-sodium diet but attacks continue
- The underlying migraine (which can cause temporary hearing loss) is never treated
Reason 5: Over-Reliance on Vestibular Suppressants
Many patients—and unfortunately, some well-intentioned physicians—reach for vestibular suppressants like meclizine (Dramamine), dimenhydrinate, or even diazepam.
Why this is problematic:
- While these medications can quiet symptoms during a violent 24-hour attack, they work by suppressing the balance system’s activity
- The brain’s natural ability to “re-calibrate” and compensate for balance deficits requires intact vestibular signaling
- Long-term use of suppressants prevents this compensation process from occurring
- The patient becomes dependent on the medication, and when they stop taking it, symptoms return—sometimes worse than before
- This creates a vicious cycle: more dizziness → more suppressants → less compensation → persistent dizziness
The paradox: The medication that provides short-term relief may actually delay long-term recovery.
The 4-Step Approach That Actually Works
Success in managing vestibular migraine requires a paradigm shift from “stopping the spin” once it starts to “preventing the spin” from occurring in the first place.
Step 1: The Foundation—Lifestyle Modification and Trigger Management
The most effective long-term strategy for VM is establishing a “migraine lifestyle.” The brain of a VM patient is hyperexcitable and thrives on regularity and consistency.
Sleep Hygiene
- Target: 7–9 hours of consistent sleep per night, same bedtime and wake time daily
- Mechanism: Sleep deprivation lowers the migraine threshold; irregular sleep triggers cascades of dysregulation
- Practical: No sleeping in on weekends; maintain consistency even during vacation
Stress Management
- Target: Identify personal stress triggers and develop coping mechanisms
- Mechanism: Stress hormones (cortisol, adrenaline) activate the fight-or-flight response, priming the nervous system for migraine
- Practical methods: Meditation, yoga, progressive muscle relaxation, cognitive behavioral therapy, exercise
Hormonal Triggers in Menstruating Individuals
- Pattern: Many women report migraines clustered around menstruation (menstrual migraine)
- Timing: Attacks often occur 2 days before to 3 days after the start of menstruation
- Mechanism: Fluctuating estrogen levels destabilize the neurochemical balance
- Management options:
- Timed preventative medication starting 2 days before expected menstruation
- Continuous hormonal contraception (to avoid hormonal fluctuations)
- Consultation with gynecologist to optimize hormone timing
Migraine Trigger Foods (See Downloadable Table Below)
Certain foods and beverages contain chemical compounds that trigger migraines in susceptible individuals:
High-Tyramine Foods:
- Aged cheeses (cheddar, blue cheese, feta)
- Fermented foods (sauerkraut, kimchi, miso)
- Cured meats (salami, pepperoni, bacon)
- Alcohol (red wine, beer, aged spirits)
High-Nitrite Foods:
- Processed meats (hot dogs, deli meats, sausages)
- Smoked foods (smoked salmon, bacon)
MSG and Food Additives:
- Monosodium glutamate (MSG)—common in Asian cuisine, processed foods
- Aspartame (artificial sweetener)
- Tartrazine (yellow food coloring)
Caffeine Paradox:
- Acute use: Caffeine can abort a developing migraine by constricting blood vessels
- Chronic use: Regular caffeine consumption raises the baseline migraine frequency; withdrawal causes rebound headaches
- Recommendation for VM: Limit to ≤100mg per day (roughly one cup of weak tea or half a cup of coffee) and maintain consistent daily intake
Hydration and Meals
- Dehydration: Even 2–3% dehydration can trigger a migraine in susceptible individuals
- Hypoglycemia: Skipping meals causes blood sugar drops, destabilizing the nervous system
- Practical: Eat small, regular meals (every 3–4 hours) and drink 2–3 liters of water daily
Environmental Triggers
- Visual: Flickering lights (some people are sensitive to 60Hz fluorescent lights), high-contrast patterns, busy visual scenes
- Auditory: Loud or sudden noises, particular frequencies
- Olfactory: Strong perfumes, chemical smells
- Weather: Barometric pressure changes, extreme heat or cold
Step 2: Prophylactic (Preventative) Medications
When attacks are frequent (more than two per month) or severely disabling, preventative medication becomes necessary. These medications are taken every day to raise the “seizure-like” threshold of the brain, making it less reactive to triggers.
Key principle: Preventative medications take 4–12 weeks to show benefit; they are not meant to abort individual attacks.
First-Line: Beta-Blockers
Mechanism: Reduce heart rate, blood pressure, and nervous system hyperreactivity
Most Common Agents:
| Drug | Starting Dose | Typical Maintenance | Advantages | Side Effects | Dr Prateek Porwal |
|---|---|---|---|---|---|
| Propranolol | 40 mg daily | 120–240 mg/day (divided) | Long track record, also effective for hypertension | Fatigue, depression, sexual dysfunction, bradycardia | Often first choice; non-selective beta-blocker |
| Metoprolol | 25 mg daily | 100–200 mg/day | Selective for heart (β1), fewer lung side effects | Similar to propranolol but slightly less CNS side effects | Good for patients with asthma/COPD |
| Timolol | 5 mg daily | 20–30 mg/day | Short half-life, easy to adjust | Fatigue, dizziness (ironic for VM patients), bradycardia | Use cautiously in VM; dizziness can worsen symptoms |
Success Rate: 40–60% reduction in migraine frequency
Timeline to Benefit: 4–8 weeks
Contraindications: Asthma, COPD, uncontrolled diabetes, bradycardia, decompensated heart failure
Second-Line: Tricyclic Antidepressants
Mechanism: Block reuptake of serotonin and norepinephrine; modulate pain pathways; have anticholinergic effects
Most Common Agents:
| Drug | Starting Dose | Typical Maintenance | Advantages | Side Effects | Dr Prateek Porwal |
|---|---|---|---|---|---|
| Amitriptyline | 10–25 mg at bedtime | 50–150 mg/day (usually single dose at night) | Dual benefit: prevents migraine AND improves insomnia/anxiety | Drowsiness (often desired for sleep), dry mouth, weight gain, urinary retention, anticholinergic effects | Excellent choice if patient also has insomnia; helps with anxiety-related dizziness |
| Nortriptyline | 10–25 mg at bedtime | 50–100 mg/day | Similar to amitriptyline but slightly less sedating, fewer anticholinergic effects | Dry mouth, drowsiness, weight gain | Alternative if amitriptyline causes excessive sedation |
Success Rate: 40–60% reduction in migraine frequency
Timeline to Benefit: 6–12 weeks (slower than beta-blockers but equally effective)
Special Consideration: Particularly useful in VM patients with comorbid Persistent Postural-Perceptual Dizziness (PPPD) due to anxiety/catastrophizing component
Third-Line: Anticonvulsants
Mechanism: Stabilize neuronal electrical activity; block ion channels; reduce excitatory neurotransmission
Most Common Agents:
| Drug | Starting Dose | Typical Maintenance | Advantages | Side Effects | Dr Prateek Porwal |
|---|---|---|---|---|---|
| Topiramate | 25 mg daily (increase slowly) | 75–200 mg/day (divided) | Cognitive benefits (weight loss, possible mood improvement); particularly effective for VM; once-daily dosing available | Cognitive dulling (“topiramate fog”—slowed thinking, word-finding difficulties), numbness/tingling, kidney stone risk, narrow-angle glaucoma risk | EXCELLENT for VM; start slowly to minimize cognitive effects; monitor hydration to prevent stones |
| Valproate (Depakote) | 250 mg daily | 500–1500 mg/day (divided) | Highly effective for migraines; FDA-approved for migraine prevention | Tremor, hair loss, weight gain, liver toxicity (monitor LFTs), teratogenicity in pregnancy, blood dyscrasias | High efficacy but more side effects; requires regular lab monitoring |
| Levetiracetam | 250 mg daily | 500–1500 mg/day (divided) | Fewer drug interactions; no liver metabolism | Behavioral changes, irritability, dizziness (can paradoxically worsen VM), somnolence | Use cautiously in VM; monitor for mood changes |
Success Rate: 40–70% reduction in migraine frequency
Timeline to Benefit: 4–12 weeks
Special Consideration for Topiramate in VM: Multiple mechanisms benefit balance—stabilizes ion channels, reduces neuronal hyperexcitability, and may improve cerebellar function
Fourth-Line: Calcium Channel Blockers
Mechanism: Block calcium entry into cells; reduce vascular reactivity; modulate neurotransmitter release
Most Common Agents:
| Drug | Starting Dose | Typical Maintenance | Advantages | Side Effects | Dr Prateek Porwal |
|---|---|---|---|---|---|
| Verapamil | 120 mg daily (sustained-release) | 240–480 mg/day | FDA-approved for migraine; excellent for migraine with aura; also effective for hypertension | Constipation (can be severe), bradycardia, hypotension, ankle edema, drug interactions | PARTICULARLY EFFECTIVE for VM; less side-effect burden than other prophylactics in some patients |
| Flunarizine | 5 mg at bedtime | 5–10 mg/day | Highly effective for migraine and VM; unique mechanism; once-daily dosing | Drowsiness, weight gain, depression, tardive dyskinesia risk (with long-term use), slower onset | NOT FDA-approved in USA but widely used internationally; excellent efficacy in VM |
Success Rate: 40–60% reduction in migraine frequency
Timeline to Benefit: 4–8 weeks for verapamil; 2–4 weeks for flunarizine
Special Note: Verapamil may be underutilized in VM despite strong evidence of efficacy
Step 3: Vestibular Rehabilitation Therapy (VRT) and Visual Desensitization
VRT is an exercise-based program that retrains the brain to ignore the incorrect signals it receives during a migraine. It is NOT a cure, but it significantly accelerates compensation and recovery.
The Mechanism: Habituation
The brain’s balance system relies on three inputs:
- Vestibular system (inner ear)
- Visual system (eyes)
- Proprioceptive system (body position sensors)
In VM, the vestibular system sends corrupted signals. Through repeated, controlled exposure to the stimuli that cause dizziness, the brain learns to:
- Downweight the corrupted vestibular input
- Rely more heavily on vision and proprioception
- Eventually stop producing the vertigo response altogether
This process is called habituation, and it requires consistent, graduated exposure to the dizziness-inducing stimulus.
Visual Desensitization Exercises
For patients whose VM is triggered by complex visual environments:
- Week 1–2: Look at simple moving patterns (e.g., scrolling vertical lines on a screen) for 1–2 minutes, multiple times daily
- Week 3–4: Progress to more complex moving patterns (checkerboards, horizontal motion)
- Week 5–6: Introduce real-world visual stimuli (watching busy crowds via video, moving vehicles)
- Week 7+: Gradual exposure to actual triggering environments (supermarkets, traffic, crowded spaces)
Key principle: Exercises should produce mild dizziness (3–4/10 intensity), not severe vertigo. The brain needs to habituate, not be overwhelmed.
Gaze Stabilization Exercises
Improves the vestibulo-ocular reflex (VOR), the reflex that keeps your eyes fixed on a target while your head moves.
Simple Exercise:
- Fixate on a target (wall poster, mark on wall)
- Move head side-to-side (or up-and-down) at increasing speeds while keeping eyes on target
- 5 minutes daily
Balance and Proprioceptive Training
- Standing on progressively unstable surfaces (foam, balance ball)
- Tandem stance (one foot in front of the other)
- Single-leg stance
- Walking heel-to-toe
Best Practice: VRT should be delivered by a physical therapist trained in vestibular disorders. PRIME ENT Center can provide referrals to certified vestibular rehabilitation specialists.
VRT + Medication Synergy
Patients who undergo VRT while on proper preventative medication often report significantly better outcomes (60–80% improvement) than those using medication alone (40–50% improvement). The medication stabilizes the nervous system while VRT retrains it.
Step 4: Addressing the Psychological Component
Persistent dizziness creates a “threat response” in the brain, leading to health anxiety, fear of falling, and avoidance behaviors.
Understanding PPPD (Persistent Postural-Perceptual Dizziness)
PPPD is a condition that develops in up to 25% of VM patients. Characterized by:
- Constant unsteadiness between migraine attacks
- “Phantom” dizziness (feeling dizzy without active migraine)
- Catastrophizing: “Will this ever end?” “Am I having a stroke?” “I’ll never be normal again”
- Avoidance: Stopping exercise, staying home, avoiding driving
The cycle:
- VM attack occurs (legitimate neurological cause)
- Patient experiences severe dizziness (real)
- Fear and health anxiety develop (psychological amplification)
- Patient avoids activities, becomes sedentary (deconditioning)
- Deconditioning and muscle weakness worsen dizziness (vicious cycle)
- Between attacks, patient feels “on edge,” anticipating the next one
Cognitive Behavioral Therapy (CBT) for VM and PPPD
CBT helps patients:
- Recognize the thought-feeling-behavior loop: “I feel dizzy → I think I’m having a stroke → I avoid activity → I feel worse”
- Challenge catastrophic thoughts: “What is the actual evidence that I’m having a stroke? The neurologist said my imaging is normal. My heart rate is fine. This is a migraine, not a stroke.”
- Gradually re-engage in activities: Using “graded exposure” similar to VRT, but for psychological resilience
- Develop acceptance: Understanding that some dizziness may persist, but it is not dangerous and can be managed
Outcome: Patients who combine VRT + preventative medication + CBT often report the best results. The medication stabilizes the nervous system, VRT retrains balance, and CBT removes the psychological amplification.
The New Frontier: CGRP Monoclonal Antibodies
What are CGRP Inhibitors?
CGRP (Calcitonin Gene-Related Peptide) is a neuropeptide released during migraine attacks. It causes:
- Vasodilation (blood vessel widening)
- Inflammation in the meninges (brain covering)
- Sensitization of pain pathways
CGRP monoclonal antibodies are laboratory-engineered proteins that bind to CGRP (or its receptor) and block its activity. Four are currently FDA-approved for migraine prevention:
| Drug | Target | Dosing | Mechanism |
|---|---|---|---|
| Erenumab (Aimovig) | CGRP Receptor | Monthly subcutaneous injection (70 or 140 mg) | Binds receptor, blocks CGRP signaling |
| Fremanezumab (Ajovy) | CGRP Peptide | Monthly or quarterly subcutaneous injection | Monoclonal antibody against CGRP |
| Galcanezumab (Emgality) | CGRP Peptide | Monthly subcutaneous injection | Humanized monoclonal antibody |
| Eptinezumab (Vyepti) | CGRP Peptide | Quarterly IV infusion | Humanized monoclonal antibody |
Efficacy in Vestibular Migraine
Emerging research suggests CGRP inhibitors may be particularly effective for VM:
Study Findings:
- VM patients treated with CGRP inhibitors show 50–70% reduction in vestibular symptoms
- This exceeds the typical 40–50% reduction seen with traditional preventatives
- Benefit emerges within 4 weeks (faster than most other medications)
- Both headache AND vertigo improve simultaneously (unlike triptans)
Proposed Mechanism in VM:
- CGRP is released not just in pain pathways but also in vestibular nuclei
- Blocking CGRP may directly stabilize the neuronal hyperexcitability in balance centers
- This explains superior efficacy compared to medications that primarily target pain or blood vessels
Practical Advantages
- Once-monthly or quarterly dosing (excellent adherence)
- Subcutaneous or IV administration (bypasses absorption issues)
- Well-tolerated with few systemic side effects
- No significant drug-drug interactions
- No cognitive side effects (unlike topiramate or anticonvulsants)
Disadvantages and Limitations
- Cost: Extremely expensive ($500–800 per month); often requires insurance approval
- Delayed onset: Benefits typically emerge at 4 weeks; full effect by 12 weeks
- Not a cure: Requires ongoing treatment; symptoms often recur if stopped
- Limited long-term data: CGRP inhibitors have been available for only 5 years; long-term safety data still emerging
- Injection/infusion burden: Monthly or quarterly clinic visits for some patients
CGRP Inhibitors at PRIME ENT Center Hardoi
If you are considering CGRP therapy for vestibular migraine:
- Confirm the diagnosis with a vestibular specialist (HINTS exam, audiometry, MRI if indicated)
- Discuss with your neurologist or headache specialist whether you qualify (typically reserved for patients with ≥4 migraine days per month despite prophylactic medication trials)
- PRIME ENT Center can provide coordination with your neurologist to monitor vestibular outcomes during CGRP therapy
Abortive (Rescue) Strategies: What to Do During an Active Attack
While prevention is key, patients still need a plan for managing an acute vestibular migraine attack.
Anti-Nausea Medication
Critical principle: Because gastric motility is severely impaired during an attack, oral pills are often ineffective.
Preferred formulations:
| Medication | Route | Advantages | Limitations |
|---|---|---|---|
| Ondansetron (Zofran) | IV, IM, or rectal suppository | Highly effective, no sedation, fast onset | Requires clinic/ER access for IV; constipation possible |
| Metoclopramide (Reglan) | IV, IM, or oral (dissolved under tongue) | Aids stomach emptying, allowing other meds to absorb; helps nausea | Dystonic reactions rare but scary; tardive dyskinesia with long-term use |
| Dimenhydrinate (Dramamine) | Suppository or IM injection | Antihistamine + anticholinergic; helps nausea and dizziness | Sedation (can be beneficial or unwanted); anticholinergic side effects |
Vestibular Sedatives for Acute Attack
Use only for short term (≤3 days) during peak attack intensity.
| Medication | Route | Dose | Use in VM |
|---|---|---|---|
| Dimenhydrinate | IM, IV, or rectal | 50–100 mg every 4–6 hours | Short-term relief; anticholinergic effects help nausea |
| Meclizine | Oral (if tolerated) | 25–50 mg every 4–6 hours | Better tolerated than dimenhydrinate but less effective |
| Diazepam | IV (ER only), oral, or rectal | 2–5 mg every 6 hours | Muscle relaxant; GABA agonist; use only for severe, disabling attacks |
Important caveat: These medications should NOT be used long-term because they prevent the brain’s natural compensation mechanisms.
Early Intervention: The “Prodrome Window”
Many VM patients experience a “prodrome” (warning period) before a full attack:
- Ear fullness
- Mild dizziness
- Visual symptoms (flickering lights, shimmering)
- Neck stiffness
If you take rescue medication during the prodrome (before vomiting starts), the attack may be aborted or significantly reduced.
Optimal rescue plan:
- At first sign of prodrome, take metoclopramide (to enhance stomach emptying) + anti-nausea medication (suppository preferred)
- Lie down in a dark, quiet room
- Apply ice pack to back of neck
- If attack escalates despite these measures, go to ER for IV anti-nausea and vestibular sedative
Conclusion: Reclaiming Your Balance and Your Life
Vestibular migraine is a complex, multisensory syndrome that requires a completely different approach than treating a typical headache. If you suffer from spinning sensations that do not respond to standard painkillers or if you experience dizziness that seems disconnected from any headache, it is time to reevaluate your diagnosis and treatment strategy.
The “Three-Legged Stool” of Effective VM Management consists of:
- Lifestyle optimization (sleep, stress, diet, trigger avoidance)
- Preventative medication (beta-blockers, tricyclics, anticonvulsants, or calcium channel blockers—ideally with CGRP inhibitors for severe cases)
- Vestibular rehabilitation therapy (retraining the brain’s balance pathways)
- Psychological support (CBT to address health anxiety and PPPD)
Expected outcomes: Most patients achieve a 50–70% reduction in symptom frequency and severity within 3–6 months of starting a comprehensive program. Some achieve complete remission, while others maintain low-frequency attacks that are manageable with lifestyle modification alone.
The key is early diagnosis, targeted treatment, and patience. There is no instant cure for a migraine that spins, but there is a pathway back to a steady, confident life. By understanding the mechanical, chemical, and neurological roots of the spin, you transform from a victim of the dizziness into an informed patient who can advocate for the right treatment and reclaim your balance.
HINGLISH VERSION
The Migraine That Spins: Kyun Headache Medicines Fail Aur Kya Actually Kaam Karti Hai
Vestibular Migraine: Ek Hidden Problem
Lakhon logo ke liye, migraine sirf ek severe headache nahi hota. Yeh ek violent, spinning experience hota hai—vestibular migraine (VM).
Yeh second most common cause of recurrent vertigo hai aur lagbhag 1% of population ko affect karti hai. Dikkat yeh hai: standard headache medicines bilkul kaam nahi karti spinning ko rokne ke liye. Patient ko triptans dete ho, patient 3 days tak ghat spinning mein rehta hai. Frustration!
Yeh article samjhata hai: vestibular migraine kya hai, kyun normal migraine medicines fail karti hain, aur kya actually kaam karti hai.
Vestibular Migraine Kya Hota Hai?
Diagnostic Criteria: Pain Ke Baad Balance
Vestibular migraine = migraine jismein primary problem balance hai, pain nahi.
Strict criteria:
- Minimum 5 episodes of vestibular symptoms (moderate-severe)
- Duration: 5 minutes to 72 hours
- Migraine history: Current or past migraine
- Migrainous features: Light sensitivity, sound sensitivity, visual aura, headache (sometimes absent), nausea
Four Types of Vestibular Migraine
Type 1: Spontaneous Vertigo
- Bilkul still baithe bhi spinning lag rahi hai
- Most distressing kyunke no clear trigger
Type 2: Positional Vertigo
- Bed se roll over, head tilt → spinning
- BPPV mimic kar sakti hai (misdiagnosis risk)
- Lekin BPPV se longer duration (minutes-hours, not seconds)
Type 3: Head-Motion Dizziness
- Walking mein “off-balance” feel
- Floor tilting jaise lag raha hai
- Prevents normal activity
Type 4: Visual Vertigo
- Busy supermarket aisle, moving cars, action movies → dizzy
- Visual environment trigger karti hai
Science of the Spin: Kya Different Hota Hai
Why Vestibular Migraine Alag Hota Hai
Normal migraine:
- Trigeminovascular system activate
- CGRP release
- Pain pathways trigger
- Headache
Vestibular migraine:
- Vestibular nuclei (balance centers) activate
- Cerebellum (coordination) activate
- Vestibular cortex (spatial orientation) activate
- Visual-vestibular pathways affect
- Result: spinning, imbalance, sometimes pain
Three Theories
Theory 1: Spreading Depression
- Wave of reduced neuronal activity spreads to vestibular cortex
- Brain loses balance signal integration
- Days tak chalti hai attack
Theory 2: Vasospasm (Blood Vessel Narrowing)
- Internal auditory artery (inner ear supply) narrows
- Inner ear + brainstem dysfunction
- Blood flow restore hote hi theek hota hai
Theory 3: Channelopathy (Ion Channel Defect)
- Genetic mutation = neurons overexcitable
- Family history possible
- Anticonvulsants kaam karti hain
Kyun Standard Migraine Medicines Fail
Reason 1: Timing Mismatch
- Aura = 5–60 minutes
- VM = days-weeks
- Triptans = short attacks ke liye designed
- Long VM attacks mein headache go karti hai, spinning rehti hai
Reason 2: Trials Mein Headache Hi Measure Karte Hain
- Vertigo ko specifically test nahi karte
- Medicines “work” head pain ke liye lekin vertigo pe proven nahi
Reason 3: Nausea = No Absorption
- Severe nausea mein stomach work nahi karti
- Pill swallow → stomach mein sit karti hai → absorb nahi hoti
- By time nausea theek, attack over
Solution: Suppositories, nasal sprays, injections use karte hain
Reason 4: Misdiagnosis
BPPV assume: Epley maneuver do (helps temporarily, doesn’t address migraine)
Menière’s assume: Salt restrict kro (kaam nahi karti, real problem = migraine)
Reason 5: Over-Suppressant Use
- Meclizine, diazepam = short-term help
- Lekin long-term use = brain compensation slow
- Patient dependent ban jaata hai medications pe
- Stop karti ho toh symptoms worse
4-Step Approach That Works
Step 1: Lifestyle—The Foundation
Sleep
- 7–9 hours, same time daily
- Irregular sleep = migraine trigger
Stress
- Meditation, yoga, exercise
- Stress hormones = migraine priming
Hormonal (Women)
- Menstruation = migraine cluster
- Solution: Timed meds or continuous contraception
Migraine Trigger Foods (See Table Below)
- Aged cheese, cured meats, MSG
- Alcohol (red wine, beer)
- Caffeine = paradox (short-term help, long-term worse)
Hydration + Meals
- 2–3 liters water daily
- Eat every 3–4 hours (blood sugar drops trigger migraine)
Environment
- Flickering lights, busy visuals, loud noise
- Barometric pressure, extreme heat/cold
Step 2: Preventative Medications
Take every day to raise migraine threshold. Benefits in 4–12 weeks.
Beta-Blockers (First-Line)
| Drug | Dose Range | Good For | Bad Effect |
|---|---|---|---|
| Propranolol | 120–240 mg/day | High BP + migraine | Fatigue, depression |
| Metoprolol | 100–200 mg/day | Asthma patients | Similar to propranolol |
| Timolol | 20–30 mg/day | Quick adjustment | Can worsen VM dizziness |
Efficacy: 40–60% reduction, 4–8 weeks
Tricyclic Antidepressants (Second-Line)
| Drug | Dose | Good For | Bad Effect |
|---|---|---|---|
| Amitriptyline | 50–150 mg bedtime | Insomnia + migraine | Drowsy, dry mouth, weight gain |
| Nortriptyline | 50–100 mg bedtime | Less sedating option | Dry mouth, weight gain |
Efficacy: 40–60% reduction, 6–12 weeks
Special: Great if anxiety + PPPD (fear-based dizziness)
Anticonvulsants (Third-Line)
| Drug | Dose | Good For | Bad Effect |
|---|---|---|---|
| Topiramate | 75–200 mg/day | Weight loss + VM | “Topiramate fog” (slow thinking), numbness, kidney stones |
| Valproate | 500–1500 mg/day | High efficacy | Hair loss, tremor, liver monitoring needed |
| Levetiracetam | 500–1500 mg/day | Fewer interactions | Dizziness, mood changes |
Efficacy: 40–70% reduction, 4–12 weeks
VM-Specific: Topiramate = EXCELLENT; stabilizes ion channels + improves cerebellar function
Calcium Channel Blockers (Fourth-Line)
| Drug | Dose | Good For | Bad Effect |
|---|---|---|---|
| Verapamil | 240–480 mg/day | VM + high BP | Constipation, bradycardia |
| Flunarizine | 5–10 mg/day | Highly effective VM | Drowsy, weight gain, depression |
Efficacy: 40–60% reduction, 4–8 weeks
VM-Specific: Verapamil PARTICULARLY effective for VM
Step 3: Vestibular Rehabilitation Therapy (VRT)
VRT = exercise program jo brain ko dizziness signals ko ignore karna sikhati hai.
Visual Desensitization
- Week 1–2: Simple moving patterns (scrolling lines)
- Week 3–4: Complex patterns (checkerboards)
- Week 5–6: Real-world visuals (busy crowds video)
- Week 7+: Actual environments (supermarket)
Key: Mild dizziness (3–4/10), not severe. Brain habituation needed.
Gaze Stabilization
- Target fix karo, head move karo side-to-side
- 5 min daily
Balance Training
- Unstable surfaces, tandem stance, single-leg
- Best with certified vestibular therapist
VRT + Medication = BEST
- 60–80% improvement (vs. 40–50% with meds alone)
Step 4: Psychology—CBT for Health Anxiety
Problem: Persistent dizziness = health anxiety, fear of falling, avoidance
Result: PPPD (constant dizziness between attacks)
PPPD Cycle
- VM attack (real)
- Fear (real)
- Avoidance (behavior)
- Deconditioning (worse dizziness)
- Constant anticipation (anxiety)
CBT Solution
- Recognize loop: Dizzy → Stroke? → Avoid activity → Worse
- Challenge thoughts: “MRI normal. Doctor says migraine. Heart rate fine. Not stroke.”
- Gradual re-engagement: Slow exposure to activities
- Acceptance: Dizziness possible lekin manageable, not dangerous
Best outcome: VRT + meds + CBT = 70–80% improvement
CGRP Monoclonal Antibodies: New Frontier
What Are They?
CGRP = neuropeptide released in migraine. Causes vasodilation, inflammation, pain sensitization.
CGRP inhibitors = antibodies jo CGRP ko block karti hain.
FDA-Approved Drugs
| Drug | Target | How | Dosing |
|---|---|---|---|
| Erenumab (Aimovig) | CGRP Receptor | Blocks receptor | Monthly injection |
| Fremanezumab (Ajovy) | CGRP Peptide | Monoclonal antibody | Monthly or quarterly |
| Galcanezumab (Emgality) | CGRP Peptide | Humanized antibody | Monthly |
| Eptinezumab (Vyepti) | CGRP Peptide | Humanized antibody | Quarterly IV |
Efficacy in Vestibular Migraine
- 50–70% reduction in vestibular symptoms (better than traditional meds!)
- Benefits within 4 weeks (faster)
- Both headache AND spinning improve
Why It Works in VM
- CGRP released in pain pathways AND vestibular nuclei
- Blocking CGRP stabilizes neuronal hyperexcitability in balance centers
- Direct effect on vestibular system (not just pain)
Advantages
- Monthly/quarterly dosing (adherence good)
- Injection/IV (bypasses stomach issues)
- Well-tolerated, no cognitive side effects
- No drug interactions
Disadvantages
- Cost: $500–800/month (insurance approval needed)
- Delayed onset: 4 weeks to benefit; 12 weeks for full effect
- Not permanent: Symptoms return if stopped
- Limited long-term data: Only 5 years available
Abortive (Rescue) Strategies: Active Attack
Anti-Nausea Medication
Principle: Pills fail (stomach motility down). Use suppositories/injections!
| Med | Route | Why |
|---|---|---|
| Ondansetron (Zofran) | IV/IM/suppository | Highly effective, no sedation |
| Metoclopramide (Reglan) | IV/IM/sublingual | Aids stomach, helps nausea |
| Dimenhydrinate (Dramamine) | Suppository/IM | Antihistamine + anticholinergic |
Vestibular Sedatives (Short-Term Only)
| Med | Dose | Use |
|---|---|---|
| Dimenhydrinate | 50–100 mg every 4–6 hrs | IM/IV/rectal, short-term |
| Meclizine | 25–50 mg every 4–6 hrs | Oral if tolerated |
| Diazepam | 2–5 mg every 6 hrs | ER only, severe attacks |
Important: Don’t use long-term! Prevents brain compensation.
Early Intervention: Prodrome Window
Prodrome (warning):
- Ear fullness
- Mild spinning
- Visual flashing
- Neck stiffness
If meds taken during prodrome, attack may be aborted or reduced!
Optimal plan:
- Prodrome sign → Take metoclopramide + anti-nausea (suppository)
- Dark, quiet room + ice pack
- If worse → ER for IV meds
Conclusion: Apna Balance Wapas Paao
Vestibular migraine = complex, multisensory syndrome. Different approach needed.
“Three-Legged Stool” of Management:
- Lifestyle (sleep, stress, diet, trigger avoidance)
- Preventative meds (beta-blockers, tricyclics, anticonvulsants, CCB, CGRP inhibitors)
- VRT (brain retraining)
- CBT (psychology support)
Expected outcome: 50–70% improvement in 3–6 months. Some get complete remission; others manage with lifestyle alone.
Key: Early diagnosis + targeted treatment + patience = back to steady, confident life!
HINDI VERSION
जो माइग्रेन घूमता है: क्यों सिरदर्द की दवाएं विफल होती हैं (और क्या वास्तव में काम करता है)
Vestibular Migraine: एक छिपी समस्या
लाखों लोगों के लिए, माइग्रेन सिर्फ एक गंभीर सिरदर्द नहीं है। यह एक हिंसक, घूमने वाला अनुभव है—vestibular migraine (VM)।
यह दूसरा सबसे आम कारण है आवर्ती vertigo का और लगभग 1% जनसंख्या को प्रभावित करता है। समस्या: मानक सिरदर्द की दवाएं घूमने को रोकने में बिल्कुल काम नहीं करती। डॉक्टर triptans देते हैं, रोगी 3 दिन तक घूमने में रहता है। निराशा!
यह लेख समझाता है: vestibular migraine क्या है, क्यों सामान्य माइग्रेन दवाएं विफल होती हैं, और क्या वास्तव में काम करता है।
Vestibular Migraine क्या होता है?
निदान मानदंड: दर्द के बाद संतुलन
Vestibular migraine = माइग्रेन जिसमें प्राथमिक समस्या संतुलन है, दर्द नहीं।
कठोर मानदंड:
- कम से कम 5 एपिसोड vestibular लक्षणों का (मध्यम-गंभीर)
- अवधि: 5 मिनट से 72 घंटे
- माइग्रेन इतिहास: वर्तमान या पिछला माइग्रेन
- माइग्रेन विशेषताएं: प्रकाश संवेदनशीलता, ध्वनि संवेदनशीलता, दृश्य aura, सिरदर्द (कभी-कभी अनुपस्थित), मतली
चार प्रकार का Vestibular Migraine
Type 1: Spontaneous Vertigo
- बिल्कुल स्थिर बैठे भी घूमना महसूस हो रहा है
- सबसे परेशान करने वाला क्योंकि कोई स्पष्ट ट्रिगर नहीं
Type 2: Positional Vertigo
- बिस्तर से पलट जाना, सिर झुकाना → घूमना
- BPPV का नकल कर सकता है (गलत निदान का जोखिम)
- लेकिन BPPV से लंबी अवधि (मिनट-घंटे, सेकंड नहीं)
Type 3: Head-Motion Dizziness
- चलने में “असंतुलित” महसूस
- फर्श झुकता जैसा लगता है
- सामान्य गतिविधि को रोकता है
Type 4: Visual Vertigo
- व्यस्त सुपरमार्केट aisle, चलती कारें, action movies → चक्कर
- दृश्य environment ट्रिगर करता है
घूमने का विज्ञान: क्या अलग होता है
Vestibular Migraine अलग क्यों होता है
सामान्य माइग्रेन:
- Trigeminovascular system सक्रिय
- CGRP release
- दर्द पथ ट्रिगर
- सिरदर्द
Vestibular माइग्रेन:
- Vestibular nuclei (संतुलन केंद्र) सक्रिय
- Cerebellum (समन्वय) सक्रिय
- Vestibular cortex (स्थानिक अभिविन्यास) सक्रिय
- दृश्य-vestibular पथ प्रभावित
- Result: घूमना, असंतुलन, कभी-कभी दर्द
तीन सिद्धांत
सिद्धांत 1: Spreading Depression
- न्यूरॉनल गतिविधि में कमी की wave vestibular cortex तक फैलती है
- दिमाग संतुलन संकेत integration खो देता है
- दिनों तक attack चलती है
सिद्धांत 2: Vasospasm (Blood Vessel Narrowing)
- Internal auditory artery (आंतरिक कान supply) संकीर्ण हो जाती है
- आंतरिक कान + ब्रेनस्टेम dysfunction
- Blood flow restore हो जाता है तो ठीक हो जाता है
सिद्धांत 3: Channelopathy (Ion Channel Defect)
- आनुवंशिक उत्परिवर्तन = neurons overexcitable
- Family history संभव
- Anticonvulsants काम करती हैं
क्यों सामान्य माइग्रेन दवाएं विफल होती हैं
कारण 1: समय Mismatch
- Aura = 5–60 मिनट
- VM = दिन-हफ्ते
- Triptans = छोटे attacks के लिए डिज़ाइन किए गए
- Long VM attacks में headache चली जाती है, spinning रहती है
कारण 2: Trials में Headache ही Measure करते हैं
- Vertigo को विशेष रूप से परीक्षण नहीं करते
- दवाएं “काम” head pain के लिए लेकिन vertigo पर proven नहीं
कारण 3: Nausea = No Absorption
- गंभीर मतली में stomach काम नहीं करता
- Pill निगल → stomach में बैठ जाता है → absorb नहीं होता
- By time नausea ठीक, attack खत्म
समाधान: Suppositories, nasal sprays, injections use करते हैं
कारण 4: Misdiagnosis
BPPV assume: Epley maneuver दो (अस्थायी मदद, migraine address नहीं)
Menière’s assume: नमक restrict करो (काम नहीं करता, असली समस्या = माइग्रेन)
कारण 5: Over-Suppressant Use
- Meclizine, diazepam = short-term मदद
- लेकिन long-term use = brain compensation धीमा
- रोगी medications पर निर्भर बन जाता है
- बंद करने से लक्षण बदतर
4-Step Approach जो काम करती है
Step 1: Lifestyle—आधार
नींद
- 7–9 घंटे, same time daily
- अनियमित नींद = माइग्रेन ट्रिगर
तनाव
- Meditation, yoga, exercise
- Stress hormones = माइग्रेन priming
हार्मोनल (महिलाएं)
- Menstruation = माइग्रेन cluster
- समाधान: Timed meds या continuous contraception
Migraine Trigger Foods (नीचे तालिका देखें)
- Aged cheese, cured meats, MSG
- Alcohol (red wine, beer)
- Caffeine = विरोधाभास (short-term मदद, long-term बदतर)
Hydration + Meals
- 2–3 लीटर पानी daily
- हर 3–4 घंटे खाएं (blood sugar drops माइग्रेन trigger करते हैं)
Environment
- Flickering lights, busy visuals, loud noise
- Barometric pressure, extreme heat/cold
Step 2: Preventative दवाएं
हर दिन लें migraine threshold बढ़ाने के लिए। 4–12 weeks में लाभ।
Beta-Blockers (First-Line)
| Drug | Dose Range | अच्छा है | बुरा असर |
|---|---|---|---|
| Propranolol | 120–240 mg/day | High BP + माइग्रेन | Fatigue, depression |
| Metoprolol | 100–200 mg/day | Asthma रोगी | Propranolol जैसा |
| Timolol | 20–30 mg/day | जल्दी adjustment | VM को बदतर कर सकता है |
Efficacy: 40–60% reduction, 4–8 weeks
Tricyclic Antidepressants (Second-Line)
| Drug | Dose | अच्छा है | बुरा असर |
|---|---|---|---|
| Amitriptyline | 50–150 mg bedtime | Insomnia + माइग्रेन | Drowsy, dry mouth, weight gain |
| Nortriptyline | 50–100 mg bedtime | कम sedating विकल्प | Dry mouth, weight gain |
Efficacy: 40–60% reduction, 6–12 weeks
विशेष: Anxiety + PPPD (fear-based dizziness) के लिए बेहतरीन
Anticonvulsants (Third-Line)
| Drug | Dose | अच्छा है | बुरा असर |
|---|---|---|---|
| Topiramate | 75–200 mg/day | Weight loss + VM | “Topiramate fog” (slow thinking), numbness, kidney stones |
| Valproate | 500–1500 mg/day | High efficacy | Hair loss, tremor, liver monitoring |
| Levetiracetam | 500–1500 mg/day | कम interactions | Dizziness, mood changes |
Efficacy: 40–70% reduction, 4–12 weeks
VM-विशिष्ट: Topiramate = EXCELLENT; ion channels को stabilize करता है + cerebellar function improve करता है
Calcium Channel Blockers (Fourth-Line)
| Drug | Dose | अच्छा है | बुरा असर |
|---|---|---|---|
| Verapamil | 240–480 mg/day | VM + high BP | Constipation, bradycardia |
| Flunarizine | 5–10 mg/day | Highly effective VM | Drowsy, weight gain, depression |
Efficacy: 40–60% reduction, 4–8 weeks
VM-विशिष्ट: Verapamil PARTICULARLY VM के लिए प्रभावी
Step 3: Vestibular Rehabilitation Therapy (VRT)
VRT = व्यायाम कार्यक्रम जो दिमाग को dizziness signals को ignore करना सिखाता है।
Visual Desensitization
- Week 1–2: सरल moving patterns (scrolling lines)
- Week 3–4: Complex patterns (checkerboards)
- Week 5–6: Real-world visuals (busy crowds video)
- Week 7+: वास्तविक environments (supermarket)
Key: हल्का dizziness (3–4/10), गंभीर vertigo नहीं। Brain habituation चाहिए।
Gaze Stabilization
- Target fix करो, head move करो side-to-side
- 5 min daily
Balance Training
- Unstable surfaces, tandem stance, single-leg
- certified vestibular therapist के साथ सर्वश्रेष्ठ
VRT + Medication = BEST
- 60–80% improvement (vs. 40–50% with meds alone)
Step 4: Psychology—CBT for Health Anxiety
समस्या: Persistent dizziness = health anxiety, falling का डर, avoidance
Result: PPPD (attacks के बीच constant dizziness)
PPPD Cycle
- VM attack (वास्तविक)
- डर (वास्तविक)
- Avoidance (व्यवहार)
- Deconditioning (बदतर dizziness)
- Constant anticipation (चिंता)
CBT समाधान
- Loop recognize करो: Dizzy → Stroke? → Activity avoid → बदतर
- Thoughts challenge करो: “MRI सामान्य है। डॉक्टर कहते हैं माइग्रेन। Heart rate ठीक है। Stroke नहीं है।”
- Gradual re-engagement: Activities के लिए slow exposure
- Acceptance: Dizziness संभव लेकिन manageable, dangerous नहीं
सर्वश्रेष्ठ परिणाम: VRT + meds + CBT = 70–80% improvement
CGRP Monoclonal Antibodies: नया Frontier
वे क्या हैं?
CGRP = neuropeptide माइग्रेन में release होता है। Vasodilation, inflammation, दर्द sensitization करता है।
CGRP inhibitors = antibodies जो CGRP को block करते हैं।
FDA-Approved ड्रग्स
| Drug | Target | कैसे | Dosing |
|---|---|---|---|
| Erenumab (Aimovig) | CGRP Receptor | Receptor को block | Monthly injection |
| Fremanezumab (Ajovy) | CGRP Peptide | Monoclonal antibody | Monthly या quarterly |
| Galcanezumab (Emgality) | CGRP Peptide | Humanized antibody | Monthly |
| Eptinezumab (Vyepti) | CGRP Peptide | Humanized antibody | Quarterly IV |
Vestibular Migraine में Efficacy
- 50–70% reduction vestibular लक्षणों में (traditional meds से बेहतर!)
- 4 weeks में लाभ (faster)
- Both headache AND spinning improve
VM में कैसे काम करता है
- CGRP release होता है pain pathways में AND vestibular nuclei में
- CGRP को block करना stabilize करता है neuronal hyperexcitability को balance centers में
- Vestibular system पर direct असर (केवल pain नहीं)
फायदे
- Monthly/quarterly dosing (अच्छी adherence)
- Injection/IV (stomach issues bypass)
- Well-tolerated, कोई cognitive side effects नहीं
- कोई drug interactions नहीं
नुकसान
- Cost: $500–800/month (insurance approval चाहिए)
- Delayed onset: 4 weeks लाभ; 12 weeks full effect
- Permanent नहीं: बंद करने से लक्षण return
- Limited long-term data: केवल 5 साल
Abortive (Rescue) रणनीतियां: सक्रिय Attack
Anti-Nausea दवा
सिद्धांत: Pills fail (stomach motility down)। Suppositories/injections use करो!
| Med | Route | क्यों |
|---|---|---|
| Ondansetron (Zofran) | IV/IM/suppository | Highly effective, कोई sedation नहीं |
| Metoclopramide (Reglan) | IV/IM/sublingual | Stomach मदद, nausea में मदद |
| Dimenhydrinate (Dramamine) | Suppository/IM | Antihistamine + anticholinergic |
Vestibular Sedatives (केवल Short-Term)
| Med | Dose | Use |
|---|---|---|
| Dimenhydrinate | 50–100 mg हर 4–6 hr | IM/IV/rectal, short-term |
| Meclizine | 25–50 mg हर 4–6 hr | Oral if tolerated |
| Diazepam | 2–5 mg हर 6 hr | ER only, गंभीर attacks |
महत्वपूर्ण: Long-term न करो! Brain compensation को रोकता है।
Early Intervention: Prodrome Window
Prodrome (चेतावनी):
- Ear fullness
- Mild spinning
- दृश्य flashing
- Neck stiffness
Prodrome के दौरान meds लिए गए तो attack abort या कम हो सकता है!
Optimal plan:
- Prodrome sign → Metoclopramide + anti-nausea लो (suppository)
- Dark, quiet room + ice pack
- Worse होने पर → ER for IV meds
निष्कर्ष: Apna Balance Wapas Paao
Vestibular migraine = complex, multisensory syndrome। अलग approach चाहिए।
“Three-Legged Stool” of Management:
- Lifestyle (नींद, तनाव, आहार, trigger avoidance)
- Preventative meds (beta-blockers, tricyclics, anticonvulsants, CCB, CGRP inhibitors)
- VRT (brain retraining)
- CBT (psychology support)
अपेक्षित परिणाम: 3–6 महीनों में 50–70% सुधार। कुछ को complete remission; अन्य lifestyle से ही manage करते हैं।
कुंजी: शीघ्र निदान + targeted treatment + धैर्य = steady, confident life वापसी!
MIGRAINE TRIGGER FOODS REFERENCE
(Downloadable Table)
🚫 Foods to Avoid or Limit for Vestibular Migraine Prevention
| Category | High-Risk Foods | Chemical | Avoid/Limit | Safer Alternatives |
|---|---|---|---|---|
| CHEESES | Aged/Hard Cheeses | Tyramine | Cheddar, Blue, Feta, Swiss, Parmesan, Aged Mozzarella | Fresh mozzarella, Cream cheese, Ricotta, Cottage cheese |
| CURED MEATS | Processed Meats | Nitrites/Nitrates | Salami, Pepperoni, Bacon, Ham, Hot dogs, Deli meats, Sausages, Prosciutto | Fresh chicken breast, Turkey, Lean beef, Fish |
| FERMENTED FOODS | Pickled/Fermented | Tyramine | Sauerkraut, Kimchi, Miso, Tempeh, Soy sauce, Tamari, Marmite | Fresh vegetables, Homemade salads |
| ALCOHOL | Alcoholic Beverages | Tyramine/Histamine | Red wine, Beer, Aged spirits, Sherry, Vermouth | White wine (occasional), Vodka (occasional, use cautiously) |
| CHOCOLATE | Dark Chocolate, Cocoa | Phenylethylamine, Caffeine | Dark chocolate (>70%), Cocoa powder, Hot chocolate | Milk chocolate (occasional), Carob |
| CAFFEINE | Coffee, Tea, Energy Drinks | Caffeine | High-caffeine coffee (>100mg/serving), Energy drinks, Strong tea | Decaf coffee (<25mg), Herbal tea, Water |
| ARTIFICIAL SWEETENERS | Artificial Additives | Aspartame, Saccharine | Diet sodas, Sugar-free desserts with aspartame | Stevia, Honey, Sugar (in moderation) |
| FOOD ADDITIVES | MSG, Dyes | Monosodium Glutamate, Tartrazine, Food colorings | Asian restaurant food (high MSG), Processed foods, Yellow/Red #5/#40 dyed foods | Home-cooked meals, Natural foods, Organic products |
| CITRUS | Acidic Fruits | Citric acid (in some individuals) | Excess orange juice, Lemon, Lime | Apples, Pears, Berries, Bananas, Grapes |
| CURED/SMOKED FISH | Smoked Salmon, Sardines | Histamine, Tyramine | Smoked salmon, Anchovies, Sardines, Herring | Fresh salmon, White fish, Tuna (fresh, not canned) |
| SOY PRODUCTS | Fermented Soy | Tyramine | Soy sauce, Miso, Tempeh | Fresh tofu (occasional), Edamame (fresh) |
| NUTS | Certain Nuts | Tyramine, Phenylethylamine | Peanuts, Peanut butter, Almonds (large quantities) | Sunflower seeds, Macadamia nuts (small amounts) |
| YEAST | Yeast-Containing Foods | Tyramine | Bread, Donuts, Yeast extracts, Nutritional yeast | Fresh bread, Yeast-free alternatives |
| DAIRY | Full-Fat Dairy (in some) | Fat, Tyramine | Full-fat milk, Whole milk yogurt | Low-fat or non-fat versions, Plant-based milk alternatives |
✅ SAFE, MIGRAINE-FRIENDLY FOODS
Proteins:
- Chicken breast (fresh)
- Turkey (fresh)
- Fish (fresh: salmon, white fish, tuna—fresh, not canned/smoked)
- Eggs (preparation methods vary; some tolerate better than others)
- Lean beef (fresh)
- Plant-based: Lentils, chickpeas, fresh tofu
Grains:
- White rice, Brown rice
- Oats
- Whole wheat bread (fresh, yeast-free versions if sensitive)
- Pasta
Fruits:
- Apples, Pears
- Berries (fresh)
- Bananas
- Grapes, Watermelon
- Peaches, Plums
Vegetables:
- Leafy greens (spinach, lettuce)
- Broccoli, Cauliflower
- Carrots, Bell peppers
- Zucchini, Green beans
- Potatoes
Dairy (if tolerated):
- Low-fat or non-fat milk
- Low-fat yogurt (plain, no additives)
- Fresh mozzarella, Ricotta, Cottage cheese
Fats/Oils:
- Olive oil
- Coconut oil
- Avocado (moderate)
Beverages:
- Water (primary)
- Herbal tea (chamomile, peppermint—caffeine-free)
- Decaffeinated coffee (limit)
- Coconut water
📋 CAFFEINE CONTENT GUIDE (Keep ≤100mg/day for VM)
| Beverage | Serving | Caffeine Content |
|---|---|---|
| Coffee (brewed, regular) | 8 oz | 80–100 mg |
| Coffee (brewed, strong) | 8 oz | 120–180 mg |
| Espresso | 1 shot (1 oz) | 63–75 mg |
| Tea (black, brewed) | 8 oz | 25–50 mg |
| Tea (green, brewed) | 8 oz | 25–35 mg |
| Tea (herbal, caffeine-free) | 8 oz | 0 mg ✅ |
| Chocolate (dark, 70%+) | 1 oz | 12–26 mg |
| Soft drink (cola) | 12 oz | 30–40 mg |
| Energy drink | 8–12 oz | 80–300 mg |
| Coffee (decaffeinated) | 8 oz | 2–5 mg ✅ |
🎯 PRACTICAL TIPS FOR TRIGGER MANAGEMENT
- Keep a Food Diary for 2–4 weeks:
- Note foods eaten each day
- Record migraine attacks (date, time, severity)
- Identify patterns
- Elimination Phase (4 weeks):
- Avoid all high-risk foods simultaneously
- Track if migraine frequency decreases
- Reintroduction Phase:
- Reintroduce one food every 3–5 days
- Observe if attack occurs
- Identify personal triggers (not everyone reacts the same way)
- Create a Personal Trigger List:
- Document which foods trigger your attacks
- Share with family and healthcare providers
- Read Labels Carefully:
- Look for MSG, artificial sweeteners, food dyes
- Check for hidden tyramine sources in processed foods
- Restaurant Navigation:
- Ask about preparation methods
- Request no MSG, no added salt
- Specify fresh (not aged) cheese
MIGRAINE TRIGGERS PERSONAL CHECKLIST
(Personal Tracking Tool)
📊 MIGRAINE TRIGGER IDENTIFICATION & TRACKING
Use this checklist to identify YOUR personal triggers over 4 weeks. Not all triggers affect all people—this helps you find YOUR specific pattern.
WEEK: | TRACKING PERIOD: to __
DAILY TRACKING SHEET
Day/Date: ____
☑️ Sleep & Circadian Rhythm
- ☐ Slept < 6 hours last night
- ☐ Slept > 10 hours last night
- ☐ Woke at different time than usual
- ☐ Took nap today (unusual)
- ☐ Jet lag or shift work today
- Notes: _____________________
☑️ Food & Drink
- ☐ Aged cheese consumed
- ☐ Cured/processed meat consumed
- ☐ Alcohol consumed (type: ) (amount: drinks)
- ☐ High-caffeine beverage (coffee, strong tea, energy drink)
- ☐ MSG-containing food (Asian food, processed food, restaurant meal)
- ☐ Artificial sweetener consumed (aspartame, saccharine)
- ☐ Skipped meals or ate late
- ☐ Dehydrated (< 2 liters water consumed)
- Notes: _____________________
☑️ Stress & Emotions
- ☐ High stress day (work, family, finances)
- ☐ Major life event (positive or negative)
- ☐ Anxiety/panic symptoms present
- ☐ Depression/low mood present
- ☐ Arguments or conflicts
- ☐ Public speaking or performance
- Stress level (1–10): _
- Notes: _____________________
☑️ Hormonal (Women/Menstruating Individuals)
- ☐ Menstruation started today (day _ of cycle)
- ☐ Period expected within 3 days
- ☐ Premenstrual symptoms (bloating, mood change)
- ☐ Hormonal contraceptive taken today
- ☐ Missed contraceptive dose
- Notes: _____________________
☑️ Environmental Factors
- ☐ Fluorescent lights present (office, store)
- ☐ Flickering lights
- ☐ High-contrast or striped patterns viewed
- ☐ Busy/crowded environment
- ☐ Loud sounds or noise exposure
- ☐ Strong perfumes or chemical smells
- ☐ Weather change (temperature, humidity, barometric pressure shift)
- ☐ Screen time > 3 hours
- Notes: _____________________
☑️ Physical Activity & Exercise
- ☐ Intense exercise performed
- ☐ No exercise (sedentary day)
- ☐ Unusual physical exertion
- ☐ Neck/shoulder tension present
- Type of activity: _____________
- Duration: ____
- Notes: _____________________
☑️ Medications & Supplements
- ☐ New medication started
- ☐ Medication dose changed
- ☐ Skipped usual medication
- ☐ Supplement taken (which: ______)
- Notes: _____________________
☑️ Illness & Health
- ☐ Cold or flu symptoms
- ☐ Fever
- ☐ Allergies present (nasal congestion, itching)
- ☐ Sinus issues (congestion, pressure)
- Notes: _____________________
☑️ MIGRAINE OUTCOME TODAY
- ☐ No migraine ✅
- ☐ Mild dizziness (1–3/10 intensity) – no vertigo
- ☐ Moderate dizziness (4–6/10) – some vertigo
- ☐ Severe migraine (7–10/10) – disabling vertigo
- ☐ Attack characteristics:
- Duration: __ hours
- Type: ☐ Spontaneous spinning ☐ Positional ☐ Head-motion dizziness ☐ Visual vertigo
- Associated headache: ☐ Yes ☐ No
- Nausea/vomiting: ☐ Yes ☐ No
- Hearing loss: ☐ Yes ☐ No
- Visual symptoms (flashing, aura): ☐ Yes ☐ No
- Time of onset: __
- Time of resolution: __
- Medications taken: __________________
- What helped: __________________
- What made it worse: __________________
WEEKLY SUMMARY (End of Each Week)
Week #: _
| Trigger Category | Days Present (0–7) | Confidence Level (Low/Medium/High) | Personal Notes |
|---|---|---|---|
| Sleep issues | _ days | ☐ Low ☐ Med ☐ High | ____ |
| Food triggers | _ days | ☐ Low ☐ Med ☐ High | ____ |
| Stress | _ days | ☐ Low ☐ Med ☐ High | ____ |
| Hormonal | _ days | ☐ Low ☐ Med ☐ High | ____ |
| Environmental | _ days | ☐ Low ☐ Med ☐ High | ____ |
| Exercise | _ days | ☐ Low ☐ Med ☐ High | ____ |
| Medications | _ days | ☐ Low ☐ Med ☐ High | ____ |
| Illness/Allergies | _ days | ☐ Low ☐ Med ☐ High | ____ |
Migraine frequency this week: _ attacks
Average severity: _ /10
Total hours disabled: __
4-WEEK PATTERN ANALYSIS
After 4 weeks of tracking, review your data:
Most Common Triggers (Rank by Frequency)
- ____ (appeared _ times in 4 weeks)
- ____ (appeared _ times in 4 weeks)
- ____ (appeared _ times in 4 weeks)
Strongest Correlations
(Which triggers ALWAYS preceded attacks?)
- ____
- ____
Safe Days (No Migraine)
What did you do differently on days with NO migraine?
- ____
- ____
- ____
Personal Trigger Severity Ranking
(Rate your top 3 triggers from WORST to LEAST WORST)
- ____ – AVOID COMPLETELY
- ____ – LIMIT/REDUCE
- ____ – MONITOR
ACTION PLAN (Based on Your Tracking)
Primary Triggers to Eliminate:
- __________________
- __________________
- __________________
Secondary Triggers to Limit:
- __________________
- __________________
Lifestyle Changes to Implement:
- ☐ Sleep schedule: bedtime _ wake time _
- ☐ Stress management: _ minutes daily (activity: ______)
- ☐ Hydration goal: __ liters per day
- ☐ Caffeine limit: ≤ 100 mg/day (__ servings max)
- ☐ Exercise routine: _ minutes, _ days/week
- ☐ Other: __________________
SUBMIT TO PRIME ENT CENTER HARDOI
Print or photograph this completed 4-week tracking sheet and bring it to your appointment. Dr. Prateek Porwal and Dr. Harshita Singh will review your personal trigger patterns to create a targeted prevention plan.
This takes your treatment from “generic migraine management” to “YOUR migraine management.”
FAQs
ENGLISH FAQs (20 Questions)
1. What is the main difference between regular migraine and vestibular migraine?
Answer: Regular migraine is pain-centered; the primary symptom is headache. Vestibular migraine is balance-centered; the primary symptom is vertigo or dizziness. Notably, up to 30% of vestibular migraine patients have NO headache at all—only spinning. This distinction is crucial because treatments differ: pain medications are ineffective for balance-centered attacks, requiring instead preventative medications and vestibular rehabilitation.
2. Why don’t triptans work for vestibular migraine?
Answer: Triptans are designed to abort short-duration attacks (pain resolves within 2–4 hours). Vestibular migraine symptoms last hours to days. While a triptan may reduce headache, the vertigo persists because: (1) the medication may not absorb properly due to nausea, (2) the vestibular nucleus requires different neurochemical intervention than pain pathways, and (3) triptans haven’t been tested specifically for vertigo outcomes in clinical trials.
3. What is CGRP and how do CGRP inhibitors help vestibular migraine?
Answer: CGRP (Calcitonin Gene-Related Peptide) is a neuropeptide released during migraine attacks. It causes blood vessel dilation, inflammation, and sensitization of pain pathways—but also affects vestibular nuclei in the brainstem. CGRP inhibitors (monoclonal antibodies) block this peptide, reducing both headache AND vestibular dysfunction. Studies show 50–70% symptom reduction in vestibular migraine patients, superior to traditional prophylactic medications.
4. How long does it take for preventative medications to work in vestibular migraine?
Answer: Most preventative medications take 4–12 weeks to show benefit. Beta-blockers and calcium channel blockers typically show benefit within 4–8 weeks. Tricyclic antidepressants and anticonvulsants may take 6–12 weeks. CGRP inhibitors show benefit within 4 weeks. Importantly, these medications do not work by aborting individual attacks; they raise the overall “seizure threshold” of the brain, making it less reactive to triggers.
5. Is topiramate (Topamax) specifically beneficial for vestibular migraine?
Answer: Yes. Topiramate is particularly effective for vestibular migraine because it: (1) stabilizes ion channels (beneficial for the “channelopathy” theory), (2) reduces neuronal hyperexcitability specifically in vestibular nuclei, (3) may improve cerebellar function, and (4) can cause weight loss (beneficial if weight is a contributing factor). Typical dose range is 75–200 mg/day. The main drawback is cognitive side effects (“topiramate fog”), which improve if the dose is increased slowly.
6. What is the role of vestibular rehabilitation therapy (VRT) in vestibular migraine?
Answer: VRT retrains the brain to ignore or “habituate” to the incorrect balance signals it receives during a migraine. Through graduated exposure to dizziness-inducing stimuli (starting mild and progressing), the brain learns to downweight corrupted vestibular input and rely more on vision and proprioception. Patients on VRT combined with preventative medication show 60–80% improvement vs. 40–50% with medication alone. VRT should be delivered by a certified vestibular rehabilitation specialist.
7. What is PPPD and how does it relate to vestibular migraine?
Answer: PPPD (Persistent Postural-Perceptual Dizziness) is a condition where patients feel constantly unsteady or dizzy between migraine attacks due to health anxiety and catastrophizing. It develops when the original vestibular migraine (legitimate neurological cause) triggers psychological fear (“Will I ever recover?” “Am I having a stroke?”), leading to avoidance and deconditioning, which perpetuates dizziness. Cognitive Behavioral Therapy (CBT) combined with VRT is essential for breaking this cycle.
8. Can vestibular migraine be cured?
Answer: There is no permanent cure, but most patients achieve 50–70% reduction in symptom frequency and severity with comprehensive management (lifestyle optimization + preventative medication + VRT + psychological support). Some achieve complete remission and require no medication. Others maintain low-frequency attacks that are manageable with lifestyle modification alone. The goal is functional improvement, not complete elimination.
9. Are there specific foods that trigger vestibular migraine?
Answer: Yes. Common triggers include aged cheeses (tyramine), cured meats (nitrites), MSG, artificial sweeteners, alcohol (especially red wine and beer), and chocolate. However, triggers are highly individual—not all people with VM are sensitive to the same foods. Keeping a 4-week food and migraine diary (see Downloadable Migraine Triggers Checklist) helps identify YOUR personal triggers, which is more valuable than following generic “migraine diet” rules.
10. How does stress trigger vestibular migraine and what can be done about it?
Answer: Stress activates the sympathetic nervous system, releasing cortisol and adrenaline. These hormones prime the nervous system for migraine by destabilizing neurotransmitter balance. Stress reduction techniques (meditation, yoga, regular exercise, cognitive behavioral therapy) lower baseline nervous system hyperexcitability. Even 10–15 minutes of daily stress management can significantly reduce attack frequency. The key is consistency; irregular stress management is less effective than daily practice.
11. Why do some vestibular migraine patients have hearing loss during attacks?
Answer: The internal auditory artery (IAA) supplies both the inner ear (cochlea) and portions of the brainstem involved in balance. During a migraine, vasospasm of this artery can cause temporary sensorineural hearing loss alongside vertigo. This is particularly relevant because sudden hearing loss + vertigo may suggest AICA (Anterior Inferior Cerebellar Artery) stroke, requiring urgent differentiation from vestibular migraine through medical evaluation and possible imaging.
12. What is the difference between abortive and preventative treatment in vestibular migraine?
Answer: Abortive medication is taken during an active attack to stop or reduce symptoms. Preventative medication is taken daily, regardless of whether an attack is occurring, to reduce overall attack frequency and severity. In vestibular migraine, prevention is more effective than abortion because: (1) absorption issues due to nausea make abortive pills unreliable, (2) vestibular symptoms are harder to abort than headache, and (3) preventative medications directly stabilize the hyperexcitable nervous system.
13. Can caffeine be beneficial for vestibular migraine?
Answer: Caffeine has a paradoxical effect in VM. Acute caffeine use (1 cup of coffee) at the start of an attack may temporarily reduce headache through vasoconstriction. However, chronic daily caffeine use actually increases baseline migraine frequency because it chronically overstimulates the nervous system. For VM patients, the recommendation is to limit caffeine to ≤100 mg/day (roughly one cup of weak tea) and maintain consistent daily intake to avoid withdrawal-induced rebound migraines.
14. How do hormonal fluctuations trigger vestibular migraine in women?
Answer: Estrogen fluctuations during the menstrual cycle destabilize serotonin and other neurotransmitter systems. Many women with VM report attack clusters 2 days before to 3 days after menstruation begins. Management strategies include: (1) timed preventative medication starting 2 days before expected menstruation, (2) continuous hormonal contraception (to avoid monthly fluctuations), or (3) consultation with a gynecologist to optimize hormone timing. Some women benefit from steady-dose hormone replacement rather than fluctuating cycles.
15. What should patients with vestibular migraine do if they cannot tolerate preventative medications?
Answer: If medication side effects are intolerable, the first step is dose optimization—starting with lower doses and increasing gradually often improves tolerability. If medication truly cannot be tolerated, alternative approaches include: (1) intensive lifestyle modification (strict sleep, stress management, trigger diet), (2) aggressive vestibular rehabilitation therapy, (3) cognitive behavioral therapy for anxiety/PPPD, and (4) discussion with your neurologist about trialing a different medication class. CGRP inhibitors, while expensive, have fewer side effects than many traditional preventatives.
16. Is there a connection between migraine with aura and vestibular migraine?
Answer: Yes. Migraine with aura and vestibular migraine likely share the same underlying mechanism: “spreading depression” of neuronal activity. In migraine with aura, spreading depression occurs in the visual cortex (causing visual symptoms). In VM, it occurs in the vestibular cortex (causing balance symptoms). Some patients experience both aura and vestibular symptoms in the same attack. Migraine with aura is a risk factor for stroke, which is why careful neuroimaging is sometimes warranted in VM patients.
17. Can vestibular migraine be diagnosed with imaging (MRI or CT)?
Answer: Imaging is typically normal in vestibular migraine. However, MRI may be warranted to rule out other causes of vertigo (stroke, tumors, multiple sclerosis) if the clinical presentation is atypical or if red flag symptoms are present. Diagnosis of VM is primarily clinical, based on strict diagnostic criteria (5+ attacks, 5 minutes to 72 hours duration, migraine history, and migrainous features). Imaging serves to rule out alternatives, not to confirm VM.
18. How should a vestibular migraine attack be managed if the patient is vomiting and cannot take oral medication?
Answer: Severe nausea and vomiting impair stomach function, making oral medication ineffective. Alternatives include: (1) anti-nausea suppositories (ondansetron, dimenhydrinate), (2) nasal sprays (some formulations of triptans, anti-nausea medications), (3) IV or IM medications (administered in an emergency department), or (4) subcutaneous injections (some triptans, other rescue medications). Many patients benefit from taking metoclopramide (which improves stomach emptying) with anti-nausea medication at the first sign of prodromal symptoms, before severe vomiting develops.
19. What is the “prodrome” in vestibular migraine and why is early intervention important?
Answer: The prodrome is a warning period before a full migraine attack, lasting minutes to hours. Symptoms include ear fullness, mild dizziness, visual flickering, or neck stiffness. Early intervention during the prodrome (before severe symptoms or vomiting develops) can significantly reduce attack severity or abort it entirely. This is why maintaining a “rescue medication kit” and recognizing your personal prodromal symptoms is valuable.
20. How can patients differentiate between vestibular migraine and other causes of recurrent vertigo (BPPV, Menière’s disease)?
Answer: Key differentiators include: (1) Duration—BPPV: seconds to minutes; VM: minutes to days; Menière’s: minutes to hours; (2) Triggers—BPPV: position-dependent; VM: spontaneous or migraine triggers; Menière’s: unpredictable; (3) Hearing loss—BPPV: no; VM: sometimes; Menière’s: yes, often progressive; (4) Migraine history—VM: always present (current or past); (5) Response to treatments—BPPV: Epley maneuver curative; VM: needs preventative medication; Menière’s: salt restriction, diuretics. A vestibular specialist (ENT or neurologist) can differentiate these conditions through clinical examination and diagnostic testing.
HINGLISH FAQs (20 Questions)
1. Regular migraine aur vestibular migraine mein main difference?
Answer: Regular = pain-centered (headache). Vestibular = balance-centered (vertigo/dizziness). Up to 30% VM patients ko headache hi nahi hota—sirf spinning. Different treatment: pain meds fail, preventative + VRT chahiye.
2. Triptans vestibular migraine ke liye kyun fail karti hain?
Answer: (1) Short duration ke liye design (2–4 hrs pain). VM = hours-days. (2) Nausea se absorption fail. (3) Headache to theek karti hain lekin vertigo nahi. (4) Triptans haven’t been tested for vertigo specifically.
3. CGRP kya hai aur CGRP inhibitors vestibular migraine mein kaise help karti hain?
Answer: CGRP = neuropeptide migraine mein release hota hai. Blood vessels dilate, inflammation, pain sensitization—lekin vestibular nuclei bhi affected. Inhibitors = antibodies jo CGRP block karti hain. 50–70% reduction in VM symptoms.
4. Preventative medications kitne time mein work karti hain?
Answer: 4–12 weeks. Beta-blockers/CCB = 4–8 weeks. Tricyclics/anticonvulsants = 6–12 weeks. CGRP inhibitors = 4 weeks. Daily lena padta hai; individual attacks ko nahi roktein, overall threshold badh jaati hai.
5. Topiramate (Topamax) vestibular migraine ke liye particularly beneficial?
Answer: Haan. Ion channels stabilize, neuronal hyperexcitability reduce, cerebellar function improve, weight loss possible. 75–200 mg/day. Downside: cognitive fog (improves slow-dose increase mein).
6. VRT vestibular migraine mein kya role?
Answer: Brain ko train karti hai dizziness signals ko ignore karne. Graduated exposure se habituation. Medication + VRT = 60–80% improvement (vs. 40–50% meds alone). Certified therapist chahiye.
7. PPPD kya hai aur vestibular migraine se relation?
Answer: Persistent PosturalPerceptual Dizziness = constant dizziness between attacks due to health anxiety. Original migraine → fear → avoidance → deconditioning → perpetuated dizziness. Solution: VRT + CBT.
8. Vestibular migraine cure ho sakta hai?
Answer: Cure nahi, lekin 50–70% improvement 3–6 months mein. Some complete remission; others low-frequency + manageable. Goal = functional improvement.
9. Specific foods vestibular migraine trigger karti hain?
Answer: Aged cheese (tyramine), cured meats (nitrites), MSG, artificial sweeteners, alcohol, chocolate. Lekin individual—not everyone reacts same. 4-week food diary = YOUR triggers find karti hai.
10. Stress vestibular migraine ko trigger kaise karti hai?
Answer: Sympathetic nervous system activate → cortisol, adrenaline → neurotransmitter imbalance. Meditation, yoga, exercise 10–15 min daily = stress hormones reduce. Consistent practice key.
11. VM mein hearing loss attacks ke time kyun?
Answer: Internal auditory artery (inner ear + brainstem supply) vasospasm hote hi temporary hearing loss + vertigo. Important: sudden hearing loss + vertigo = possible stroke, urgent evaluation chahiye.
12. Abortive aur preventative treatment difference?
Answer: Abortive = during attack (relieves active symptoms). Preventative = daily (reduces frequency/severity). VM mein prevention better kyunke absorption issues + vestibular symptoms harder to abort.
13. Caffeine vestibular migraine ke liye beneficial hai?
Answer: Paradox. Acute = short-term headache relief possible. Chronic = increases migraine frequency. Recommendation: ≤100 mg/day, consistent intake (avoid withdrawal).
14. Women mein hormonal fluctuations vestibular migraine trigger kaise karti hain?
Answer: Menstrual cycle mein estrogen changes → serotonin instability → attacks cluster menstruation around. Solutions: timed meds, continuous contraception, gynecologist consultation.
15. Agar preventative meds tolerate nahi kar sakte?
Answer: (1) Slow dose increase try karo. (2) Different medication class try. (3) Lifestyle + VRT + CBT aggressive. (4) CGRP inhibitors (fewer side effects, expensive).
16. Migraine with aura aur vestibular migraine connection?
Answer: Same mechanism—spreading depression. Aura = visual cortex. VM = vestibular cortex. Some patients dono mein experience both. Aura = stroke risk, so imaging sometimes warranted.
17. Imaging (MRI/CT) se vestibular migraine diagnose ho sakta hai?
Answer: Normal imaging usually. Lekin MRI stroke, tumors, MS rule out karne ke liye use hoti hai (red flags mein). Diagnosis = clinical, based on strict criteria.
18. Agar vomiting aa raha hai aur oral medication nahi le sakte?
Answer: Suppositories, nasal sprays, IV/IM medications, subcutaneous injections use karte hain. Metoclopramide + anti-nausea at prodrome start (before severe vomiting).
19. “Prodrome” kya hai aur early intervention important kyun?
Answer: Warning period minutes-hours pehle = ear fullness, mild dizziness, visual flickering. Early meds = attack abort or reduce possible. Prodromal symptoms recognize karti ho toh rescue kit ready rakhो.
20. BPPV, Menière’s, Vestibular Migraine mein difference?
Answer: Duration: BPPV = seconds-minutes, VM = minutes-days, Menière’s = minutes-hours. Triggers: BPPV = position, VM = migraine triggers, Menière’s = unpredictable. Hearing: BPPV = no, VM = sometimes, Menière’s = yes. Migraine history: VM = always. Treatment: BPPV = Epley, VM = preventative meds, Menière’s = salt restriction.
HINDI FAQs (20 Questions)
1. Regular migraine और vestibular migraine में मुख्य अंतर?
Answer: Regular = pain-centered (सिरदर्द)। Vestibular = balance-centered (vertigo/चक्कर)। 30% VM रोगियों को सिरदर्द ही नहीं—सिर्फ घूमना। अलग उपचार: pain meds fail, preventative + VRT चाहिए।
2. Triptans vestibular migraine के लिए क्यों विफल होती हैं?
Answer: (1) Short duration के लिए design (2–4 hrs)। VM = दिन-हफ्ते। (2) Nausea से absorption fail। (3) Headache ठीक करती हैं लेकिन vertigo नहीं। (4) Vertigo के लिए specifically परीक्षण नहीं।
3. CGRP क्या है और CGRP inhibitors vestibular migraine में कैसे मदद करती हैं?
Answer: CGRP = neuropeptide माइग्रेन में release होता है। Blood vessels dilate, inflammation, दर्द sensitization—लेकिन vestibular nuclei भी affected। Inhibitors = antibodies जो CGRP को block करती हैं। VM लक्षणों में 50–70% कमी।
4. Preventative medications कितने समय में काम करती हैं?
Answer: 4–12 सप्ताह। Beta-blockers/CCB = 4–8 सप्ताह। Tricyclics/anticonvulsants = 6–12 सप्ताह। CGRP inhibitors = 4 सप्ताह। Daily लेना पड़ता है; individual attacks को नहीं रोकती, overall threshold बढ़ जाती है।
5. Topiramate (Topamax) vestibular migraine के लिए विशेष रूप से लाभकारी?
Answer: हाँ। Ion channels को stabilize करता है, neuronal hyperexcitability कम करता है, cerebellar function improve करता है, weight loss संभव है। 75–200 mg/day। कमी: cognitive fog (धीरे-धीरे dose बढ़ाने से improves)।
6. VRT vestibular migraine में क्या भूमिका है?
Answer: दिमाग को dizziness signals को ignore करना सिखाता है। Graduated exposure से habituation। Medication + VRT = 60–80% improvement (vs. 40–50% meds alone)। Certified therapist चाहिए।
7. PPPD क्या है और vestibular migraine से संबंध?
Answer: Persistent PosturalPerceptual Dizziness = attacks के बीच constant dizziness health anxiety के कारण। Original migraine → डर → avoidance → deconditioning → perpetuated dizziness। समाधान: VRT + CBT।
8. Vestibular migraine ठीक हो सकता है?
Answer: ठीक नहीं, लेकिन 50–70% सुधार 3–6 महीनों में। कुछ को complete remission; अन्य low-frequency + manageable। लक्ष्य = functional improvement।
9. विशिष्ट खाद्य पदार्थ vestibular migraine को ट्रिगर करते हैं?
Answer: Aged cheese (tyramine), cured meats (nitrites), MSG, artificial sweeteners, alcohol, chocolate। लेकिन individual—हर किसी को same react नहीं करते। 4-week food diary = YOUR triggers पता चलते हैं।
10. Stress vestibular migraine को कैसे ट्रिगर करता है?
Answer: Sympathetic nervous system activate → cortisol, adrenaline → neurotransmitter imbalance। Meditation, yoga, exercise 10–15 min daily = stress hormones कम। Consistent practice key।
11. VM में hearing loss attacks के समय क्यों?
Answer: Internal auditory artery (inner ear + brainstem supply) vasospasm हो तो temporary hearing loss + vertigo। महत्वपूर्ण: sudden hearing loss + vertigo = संभावित stroke, urgent evaluation चाहिए।
12. Abortive और preventative treatment में अंतर?
Answer: Abortive = during attack (active symptoms राहत)। Preventative = daily (frequency/severity कम)। VM में prevention बेहतर है क्योंकि absorption issues + vestibular symptoms abort करना कठिन।
13. Caffeine vestibular migraine के लिए लाभकारी है?
Answer: विरोधाभास। Acute = short-term headache relief संभव। Chronic = migraine frequency बढ़ता है। सिफारिश: ≤100 mg/day, consistent intake (withdrawal से बचें)।
14. महिलाओं में हार्मोनल fluctuations vestibular migraine को कैसे ट्रिगर करते हैं?
Answer: Menstrual cycle में estrogen changes → serotonin instability → attacks menstruation के आसपास cluster। समाधान: timed meds, continuous contraception, gynecologist consultation।
15. अगर preventative meds tolerate नहीं कर सकते?
Answer: (1) Slow dose increase try करो। (2) Different medication class try करो। (3) Lifestyle + VRT + CBT aggressive। (4) CGRP inhibitors (कम side effects, expensive)।
16. Migraine with aura और vestibular migraine का संबंध?
Answer: Same mechanism—spreading depression। Aura = visual cortex। VM = vestibular cortex। कुछ रोगियों को दोनों एक ही attack में। Aura = stroke risk, तो कभी-कभी imaging warranted।
17. Imaging (MRI/CT) से vestibular migraine diagnose हो सकता है?
Answer: Normal imaging usually। लेकिन MRI stroke, tumors, MS rule out करने के लिए use होती है (red flags में)। Diagnosis = clinical, strict criteria पर based।
18. अगर vomiting आ रही है और oral medication नहीं ले सकते?
Answer: Suppositories, nasal sprays, IV/IM medications, subcutaneous injections use करते हैं। Metoclopramide + anti-nausea prodrome शुरुआत में (severe vomiting से पहले)।
19. “Prodrome” क्या है और early intervention महत्वपूर्ण क्यों?
Answer: Warning period minutes-hours पहले = ear fullness, mild dizziness, visual flickering। Early meds = attack abort या reduce संभव। Prodromal symptoms पहचानो तो rescue kit ready रखो।
20. BPPV, Menière’s, Vestibular Migraine में अंतर?
Answer: Duration: BPPV = सेकंड-मिनट, VM = मिनट-दिन, Menière’s = मिनट-घंटे। Triggers: BPPV = position, VM = migraine triggers, Menière’s = unpredictable। Hearing: BPPV = नहीं, VM = कभी-कभी, Menière’s = हाँ। Migraine history: VM = always। Treatment: BPPV = Epley, VM = preventative meds, Menière’s = salt restriction।
